Abstract
Despite the increasing use of complementary and alternative medicine (CAM) worldwide, little is known about the factors associated with the interest in receiving CAM education among pharmacy under-graduate students in University of Malaya, Malaysia. The study aimed to describe pharmacy students’ interest for CAM education and determine factors, which predicted interest in receiving CAM education. A cross-sectional survey was conducted among all undergraduate pharmacy students in University of Malaya using a structured questionnaire and face-to-face interview. A logistic regression analysis was used to predict factors associated with the likelihood that students would report their interest in receiving CAM education. About 80% of the total 250 undergraduate pharmacy students wanted CAM to be incorporated into the pharmacy curriculum. Three factors predictive of an interest to receive CAM education were student's year of study, those who previously sought CAM information, and those who indicated that CAM should not be restricted to CAM practitioners. As future healthcare professionals, the incorporation of CAM education may provide a chance for students to have accurate and impartial information on CAM. Further research into the content and focus of CAM education is necessary to meet the educational needs of the future pharmacists.
Keywords: CAM educationpredictorscurriculumpharmacylogistic regression
Introduction
Complementary and Alternative Medicine (CAM) is readily available, affordable and perceived to be effective and safe (James & Bah, 2014). As CAM is increasingly used in both developed and developing countries, the World Health Organisation (WHO) has developed a strategy to support WHO Member States “to implement action plans to strengthen the role of traditional medicine to keep the populations healthy” (WHO, 2013). To be in line with the WHO’s strategy, the Ministry of Health Malaysia has gazetted the Traditional and Complementary Medicine ACT 2016 [ACT 775] for the regulation of CAM products and services in the country (MOH, 2016). All these developments have resulted in changing expectations about the need for healthcare professionals to be trained about CAM in Malaysia.
Faced with an increasing demand for information on CAM, patients expect healthcare professionals particularly pharmacists to discuss CAM usage and limitations as well as any possible side effects (Gaylord & Mann, 2007; Schjøtt & Erdal, 2014). However, one Australian study reported that less than 15% of community pharmacists were comfortable in answering questions regarding safety, interactions, and benefits of CAM. The majority of the pharmacists indicated that their training in CAM was inadequate to meet their needs in providing information regarding CAM use (Semple et al., 2006). It is clear that the need for a comprehensive CAM training for undergraduate pharmacy students is crucial (Fasinu, Bouic, & Rosenkranz, 2012). Besides providing students better understanding of CAM modalities, the addition of CAM modules may broaden their horizon to allow better acceptance and appreciation of the patient’s choice in achieving better health outcomes (Tiralongo & Wallis, 2008b).
The Institute of Medicine's Committee on the use of CAM by the American Public (2005) has recommended that curricula for healthcare professionals incorporate elements about CAM so that they can competently advise patients about safe and alternatives of CAM to maintain and improve health. Similarly, the Pharmacy Board of Malaysia, the body that governs the accreditation and recognition of pharmacy degree programmes has outlined the requirement for curricular elements of CAM for undergraduate pharmacy education programme (Pharmacy Board Malaysia, 2007). Surveys involving pharmacy schools in the US found that the majority of the schools offered some form of CAM training in the curriculum which was primarily offered as electives (Dutta, Daftary, Egba, & Kang, 2003; Scaletta, Ghelani, & Sunny, 2017). Currently, CAM courses are also common in the curricula of pharmacy students in Canada (Johnson et al., 2008) and European countries (Barberis, de Toni, Schiavone, Zicca, & Ghio, 2001).
Surveys done in the US (Noureldin & Blake, 2011), Australia and New Zealand (Tiralongo & Wallis, 2008a; Tiralongo, 2013) and Pakistan (Hussain et al., 2012) showed that generally pharmacy students showed a positive attitude towards the use of CAM and perceived CAM as a core and integral part of their professional degree. The increasing focus on CAM and the widespread incorporation of CAM into pharmacy curricula, make it essential to gain insights into the views and factors associated with interest to receiving CAM education among the undergraduate pharmacy students in Malaysia. Thus, the study aimed to investigate the proportion of pharmacy students who are interested in CAM education and to identify factors, which predicted this interest.
Problem Statement
Despite the increasing use of complementary and alternative medicine (CAM) worldwide, little is known about the factors associated with the interest in receiving CAM education among pharmacy undergraduate students in University of Malaya.
Research Questions
Two research questions were formulated to guide this study:
What is the proportion of pharmacy students at University of Malaya who was interested in receiving CAM education?
What are the factors that significantly predicted the interest in receiving CAM education among the Pharmacy undergraduate students?
Purpose of the Study
The study aimed to identify the proportion of pharmacy undergraduate students who were interested in receiving CAM education and identify the factors, which predicted interest in receiving CAM education.
Research Methods
Study Design
We conducted a descriptive cross-sectional survey involving all undergraduate pharmacy students in the University of Malaya. A pilot study was conducted among eight students in December 2015 to test the feasibility and practicability of the questionnaires and study procedure.
Ethics approval of this study was obtained from the Medical Ethics Committee of the University of Malaya Medical Center (MECID: 201510-1803). Almost all students (n=250) participated in the survey. Before the administration of the questionnaire, participants were briefed about the purpose of the study and their oral consent was obtained. Responses to the self-completed questionnaire were anonymous and confidentiality was strictly maintained.
Instrument
The survey questionnaire consisted of five sections. Section A consists of questions on demographics of respondents (gender, ethnicity, year of study, and medical history, illness, or diseases). Section B contained six questions that were assessed by using the ‘Yes’ or ‘No’ option. Examples of questions asked were the respondents’ previous use of CAM, their perceived view on safety and effectiveness of CAM and whether they felt that CAM education should be restricted to CAM practitioners. Section C asked whether the students have sought information regarding CAM and if yes, their source of information. Section D asked about the perceived barriers to CAM education and multiple responses were allowed. Section E asked whether the respondent was interested in receiving training in CAM education with a ‘Yes’ or ‘No’ response.
Statistical Analysis
Data collected from the completed questionnaires were entered and analysed using the Statistical Package for Social Sciences (SPSS) version 20. Descriptive statistics such as frequencies and percentages were used to describe the data. Chi-square test or Fischer exact test was used to determine the association of the categorical data. The conventional p < 0.05 was used to determine statistical significance
The dependent variable, “Are you interested in receiving CAM education?” was a dichotomous measure. The variables were coded 1 = “Yes” and 0 = “No”. Univariate logistic regression analysis was initially done to identify variables for inclusion into the multivariate logistic regression model. Statistical significance at p < 0.10 level was used to determine significance of variables for inclusion into the model. For ordered categorical data with more than two levels (the year of study), the lowest level (Year 1) was used as the reference group. For the nominal scale variable with more than two levels, (ethnicity) were entered as k-1 dummy variables. For the ethnic variable, Malays was treated as the reference group. For the dichotomous variable, “No” was treated as the reference group. A multivariate logistic regression analysis was performed which included all factors found to be statistically significant (p<0.10) from the univariate logistic regression analysis.
Findings
Characteristics of Respondents
Almost all the pharmacy undergraduate students (n=250) participated and completed the survey. The ethnic distribution of the sample did not reflect the Malaysian population with Chinese respondents making up the majority (Table
Table
Perceived Barriers to CAM education
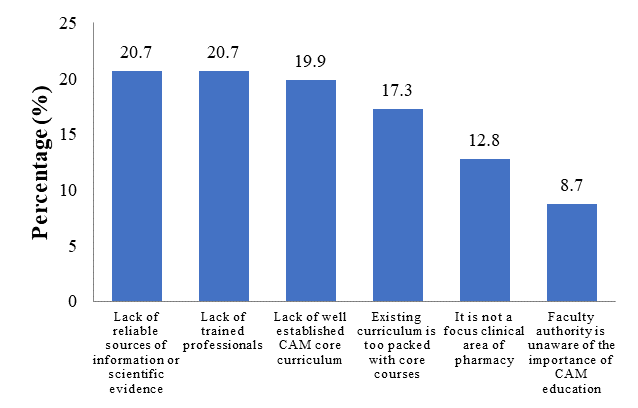
Among the top two barriers to CAM education found were lack of reliable sources of information or scientific evidence and lack of trained professionals (Figure
Sources of CAM Information
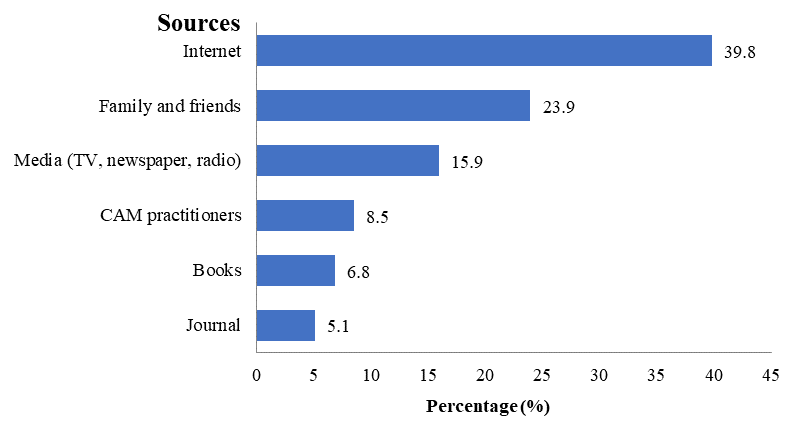
Only 93 (37.2%) of the students had sought CAM information. Of these 93 students, many gave more than one source of obtaining their information. The CAM information was mainly sought from the internet and from family and friends (Fig 2).
Predictors of Interest in CAM Education
A univariate logistic regression analysis indicated interest in receiving CAM education was associated with the year of study, previous use of CAM, had sought information about CAM and the response to the question “CAM education should be restricted to CAM practitioners.” All these variables were included in the multivariate logistic regression model.
Table
Discussion
This study determined the proportion of pharmacy students that was interested in receiving CAM education as well as the factors associated with the interest. Overall, our results showed that the majority of undergraduate pharmacy students were interested in receiving CAM education which is consistent with findings from another Malaysian study (Hasan et al., 2011) and studies from other countries (Freymann, Rennie, Bates, Nebel, & Heinrich, 2006; Pokladnikova & Lie, 2008; James & Bah, 2014). The high proportion of students interested in receiving CAM training could probably be due to their awareness of the lack of CAM knowledge among pharmacist and the lack of student textbook covering a standardised syllabus for CAM education (Bushett, Dickson-Swift, Willis, & Wood 2011; Münstedt, Harren, von Georgi, & Hackethal, 2011). Also, almost 70% of the students disagreed with the statement “CAM education should be restricted to CAM practitioner.” Our finding is similar to another study (Harris Kingston, Rodriguez, & Choudary, 2006) as students probably acknowledged that as future pharmacist, they should be able to advise their patients about the common CAM modalities. Based on the willingness of most of the students in receiving CAM education, this would have a considerable effect for pharmacy programme to incorporate CAM contents when designing the curriculum.
The successful integration of CAM into the curriculum requires a strategic blueprint and that comes with challenges. In our study, the majority of the students perceived lack of trained professionals such as their lecturers as one of the major barriers. Our finding was in agreement with the challenges identified in a study by Lee et.al (2007) that cited the need for qualified faculty members in CAM education. A qualified teaching staff is deemed essential in the CAM integration and implementation process as well as developing communication among pharmacy students. CAM integration remains a major challenge due to lack of academic staff time and resources, a common problem shared with many institution. Our study also identified lack of scientific evidence or information as a major barrier that is consistent with findings from other studies (Hasan et.al, 2011; Scaletta, Ghelani, & Sunny, 2017). The lack of evidence could be attributed to the scarcity of well-designed clinical trials leading to uncertainty over CAM effects or safety. Also, most CAM studies that fit the current double-blind randomised controlled trials yield inconclusive results requiring the need for more rigorous randomized controlled trials before CAM can be incorporated in the curriculum as well as in medical practice (Manheimer, Wieland, Kimbrough, Cheng, & Berman, 2009).
We found that the main source of CAM information was from the internet. The finding is in agreement with another Malaysian study among pharmacy students due to the Internet’s easy accessibility and availability (Wahab, Ali, Zulkifly, & Aziz, 2014). Family and friends were ranked second and we could speculate that the students had parents or other relatives who use CAM.
Our multivariate analysis highlighted some interesting findings. For example, in the univariate analysis interest to receive CAM education was found to be associated with the year of study, previous use of CAM, students seeking CAM information and response to the question that CAM education should not be restricted to CAM practitioners. However, when the influence of other potential predictors was adjusted in the multivariate analysis, the variable “previous use of CAM” did not show statistically significant influence. Being a Year 3 student is the strongest predictor of interest in receiving CAM education compared to being Year 1 student. The interest could be generated as a result of their exposure to CAM topics in pharmacognosy classes in Year 3. Similarly, one study involving medical students found that students exposed to CAM education were more likely to be interested in CAM integration in the curriculum compared to those who had no exposure (Furnham et al., 2003).
Our study had several limitations. One, since the study design is a cross-sectional survey, the students were not followed longitudinally to assess whether their interest in CAM education remains stable as the study progresses. Two, the sample is limited to the undergraduate pharmacy students in University Malaya and thus does not represent the pharmacy students in Malaysia. Three, the students were asked about previous used of CAM or whether they sought CAM information in the previous year, which is prone to recall bias, as they may find it difficult to remember exactly what products were used. However, the findings from this study are useful for the Department of Pharmacy, the University of Malaya to consider integrating CAM topics into the curriculum to make its graduates competitive with current national and global trend.
Conclusion
A high proportion of pharmacy students was interested in receiving CAM education and they perceived lack of trained professionals, and a lack of a reliable source of information or scientific evidence as the main barriers to CAM education. CAM education needs to be integrated into the pharmacy curriculum to produce pharmacists with capabilities to provide CAM information in line with the rising use of CAM products. Future studies should look at the preferences of the students for appropriate learning methods and the content and focus of CAM education to meet the educational needs of our future pharmacists. The findings from this study are useful for the Department of Pharmacy, the University of Malaya in its preparation for the next curriculum review.
References
- Ameade, E.P.K., Amalba, A., Helegbe, G.K. & Mohammed, B.S. (2016). Medical students' knowledge and attitude towards complementary and alternative medicine–A survey in Ghana. Journal of Traditional and Complementary Medicine, 6(3), 230-236.
- Barberis, L., de Toni, E., Schiavone, M., Zicca, A. & Ghio, R. (2001). Unconventional medicine teaching at the Universities of the European Union. The Journal of Alternative & Complementary Medicine, 7(4), 337-343.
- Brinkhaus, B., Witt, C.M., Jena, S., Bockelbrink, A., Ortiz, M. & Willich, S.N. (2011). Integration of complementary and alternative medicine into medical schools in Austria, Germany and Switzerland–Results of a cross-sectional study. Wiener Medizinische Wochenschrift, 161 (1-2), 32-43.
- Bushett, N. J., Dickson-Swift, V. A., Willis, J. A., & Wood, P. (2011). Rural Australian community pharmacists' views on complementary and alternative medicine: a pilot study. BioMed Central Complementary and Alternative Medicine, 11(1), 103.
- Dutta, A.P., Daftary, M.N., Egba, P.A., & Kang, H. (2003). State of CAM education in U.S. schools of pharmacy: results of a national survey. Journal of the American Pharmaceutical Association, 42(6), 81-83.
- Fasinu, P.S., Bouic, P.J. & Rosenkranz, B. (2012). An overview of the evidence and mechanisms of herb drug interactions. Frontiers in Pharmacology, 3, 69.
- Freymann, H., Rennie, T., Bates, I., Nebel, S., & Heinrich, M. (2006). Knowledge and use of complementary and alternative medicine among British undergraduate pharmacy students. Pharmacy World and Science, 28, 13-18.
- Gaylord, S.A. & Mann, J.D. (2007). Rationales for CAM education in health professions training programs. Academic Medicine, 82(10), 927-933.
- Harris, I. M., Kingston, R. L., Rodriguez, R., & Choudary, V. (2006). Attitudes towards complementary and alternative medicine among pharmacy faculty and students. American Journal of Pharmaceutical Education, 70(6), 129.
- Hasan, S.S., Yong, C.S., Babar, M.G., Naing, C.M., Hameed, A., Baig, M.R., Iqbal, S.M. & Kairuz, T. (2011). Understanding, perceptions and self-use of complementary and alternative medicine (CAM) among Malaysian pharmacy students. BMC Complementary and Alternative Medicine, 11, 95.
- Hussain, S., Malik, F., Hameed, A., Ahmed, S., Riaz, H., Abbasi, N. & Malik, M. (2012). Pakistani pharmacy students’ perception about complementary and alternative medicine. American Journal of Pharmaceutical Education, 76(2), 21.
- Institute of Medicine (US) Committee on the Use of Complementary and Alternative Medicine by the American Public. Complementary and Alternative Medicine in the United States. Washington (DC): National Academies Press (US); 2005. 8, Educational Programs in CAM. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK83809 accessed 25 May 2018.
- Institute of Medicine (US) Committee on the Use of Complementary and Alternative Medicine by the American Public. (2005). Complementary and Alternative Medicine in the United States. Washington (DC): National Academies Press (US); 2005. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK83799/doi: 10.17226/11182 accessed 27 May 2018.
- James, P.B. & Bah, A.J. (2014). Awareness, use, attitude and perceived need for Complementary and Alternative Medicine (CAM) education among undergraduate pharmacy students in Sierra Leone: a descriptive cross-sectional survey. BMC Complementary and Alternative Medicine, 14,438.
- Johnson, T., Boon, H., Jurgens, T., Austin, Z., Moineddin, R., Eccott, L. & Heschuk, S. (2008). Canadian pharmacy students' knowledge of herbal medicine. American Journal of Pharmaceutical Education, 72(4), 75.
- Lee, M.Y., Benn, R., Wimsatt, L., Cornman, J., Hedgecock, J., Gerik, S., Zeller, J., Kreitzer, M.J., Allweiss, P., Finklestein, C. & Haramati, A. (2007). Integrating complementary and alternative medicine instruction into health professions education: organizational and instructional strategies. Academic Medicine, 82(10), 939-945.
- Manheimer, E., Wieland, S., Kimbrough, E., Cheng, K. & Berman, B.M. (2009). Evidence from the Cochrane Collaboration for traditional Chinese medicine therapies. The Journal of Alternative and Complementary Medicine, 15(9), 1001-1014.
- Ministry of Health Malaysia (2016). Traditional and Complementary Act 2016. Retrieved at http://tcm.moh.gov.my/en/index.php/akta-pt-k-2016/akta2016 accessed 27 May 2018.
- Münstedt, K., Harren, H., von Georgi, R., & Hackethal, A. (2011). Complementary and alternative medicine: comparison of current knowledge, attitudes and interest among German medical students and doctors. Evidence-based Complementary and Alternative Medicine, 2011, 1-7.
- Noureldin, M., Murawski, M.M., Mason, H.L. & Plake, K.S. (2013). Student pharmacists’ attitudes toward complementary and alternative medicine. Journal of the American Pharmacists Association, 53(6), 618-625.
- Pharmacy Board Malaysia (2007). Guidelines on approval and recognition of a Pharmacy program. Retrieved at https://www.pharmacy.gov.my/v2/sites/default/files/document-upload/guidelines-approval-and-recognition-pharmacy-program_0.pdf accessed 27 May 2017.
- Rouse, M. J. (2004). Continuing professional development in pharmacy. American Journal of Health-System Pharmacy, 61, 2069-2076.
- Pokladnikova, J. & Lie, D. (2008). Comparison of attitudes, beliefs, and resource-seeking behavior for CAM among first- and third-year Czech pharmacy students. American Journal of Pharmacy Education, 72(2), 24.
- Scaletta, A., Ghelani, N., & Sunny, S. (2017). Complementary and alternative medicine education in U.S. schools and colleges of pharmacy. Currents in Pharmacy Teaching and Learning, 9(4), 521-527.
- Schjøtt, J. & Erdal, H. (2014). Questions about complementary and alternative medicine to the Regional Medicines Information and Pharmacovigilance Centres in Norway (RELIS): a descriptive pilot study, BMC Complementary and Alternative Medicine, 14, 56.
- Semple, S.J., Hotham, E., Rao, D., Martin, K., Smith, C.A. & Bloustien, G.F. (2006). Community pharmacists in Australia: barriers to information provision on complementary and alternative medicines. Pharmacy World and Science, 28(6), 366-373.
- Tiralongo, E. (2013). Inclusion of complementary and alternative medicine (CAM) teaching into pharmacy curricula – a crosssectional survey of Australian and New Zealand Schools/Department of pharmacy. 7th International Technology, Education and Development Conference. Griffith University, Australia, 4586-4595.
- Tiralongo, E. & Wallis, M. (2008a). Attitudes and perceptions of Australian pharmacy students towards Complementary and Alternative Medicine - a pilot study. BMC Complementary and Alternative Medicine, 8(1), 2.
- Tiralongo, E. & Wallis, M. (2008b). Integrating complementary and alternative medicine education into the pharmacy curriculum. American journal of pharmaceutical education, 72(4), 74.
- Wahab, M. S. A., Ali, A. A., Zulkifly, H. H., & Aziz, N. A. (2014). The need for evidence-based complementary and alternative medicine (CAM) information in Malaysian pharmacy curricula based on pharmacy students’ attitudes and perceptions towards CAM. Currents in Pharmacy Teaching and Learning, 6(1), 114-121.
- World Health Organization (2013). WHO traditional medicine strategy: 2014-2023. World Health Organization. Retrieved from http://www.who.int/iris/handle/10665/92455 accessed 27 May 201.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
14 January 2019
Article Doi
eBook ISBN
978-1-80296-052-5
Publisher
Future Academy
Volume
53
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-812
Subjects
Education, educational psychology, counselling psychology
Cite this article as:
Aziz, Z., Hisham, M. D. B., & Yi, L. H. (2019). Incorporation Of Complementary And Alternative Medicine In An Undergraduate Pharmacy Curriculum. In Z. Bekirogullari, M. Y. Minas, & R. X. Thambusamy (Eds.), ICEEPSY 2018: Education and Educational Psychology, vol 53. European Proceedings of Social and Behavioural Sciences (pp. 565-574). Future Academy. https://doi.org/10.15405/epsbs.2019.01.54

