Abstract
The research deals with practical aspects of measuring the integral performance of the Russian health system and the role of public and private funding sources in contributing and facilitating the health growth. We introduce life expectation as an integral indicator of health and derive multiple regression models that quantitate contribution of the public and private sectors to the increase of health. It is determined that the decreasing proportion of the public sector health expenditure and the growth of the private sector share is not a positive outcome of institutional development, because the majority of private sector funding is represented by out-of-pocket expenditure which is proved to be akin to income tax, but with a selective scope of imposition. We provide the methodology for evaluating the healthcare burden on individuals and derive regression models that undermine the concept of the “pay as you go” method that is being widely discussed concerning the future reforms of the Russian healthcare system.
Keywords: Healthhealth expenditureout-of-pocket paymentspublic-private partnershiphealth sector performance
Introduction
Following the discussion on the matters of health sector performance and efficiency evaluation, we conclude that the proper indicator could be the one that measures the integral change of health and its infrastructure in some numeric form, which would be comparable and allow for dynamic specification. The problem itself is not a brand new one, due to the fact that several attempts have been made recently to design and implement comprehensive health system performance scorecard that would entail and consider the data from several “domains of health outcomes, quality, access, equity, and efficiency” (Schoen et al., 2006).
Not arguing with the multitude of researchers, we introduce an indicator which meets the most of the requirements for performance measurements – the expectation of life at a given age, and we intend to give an appropriate rationale in several forthcoming papers. This indicator is very instrumental because it is almost free from inertial development effects, generally due to its multidimensional interrelation tohealth system and infrastructure development, or economic development as well. According to Shaytura et al., (2016) integrating the multiverse factors contributes to the increase of social and economic systems manageability (Shaytura et al., 2016). Thus such an approach is worth implementing.
The expectation of life in different age cohorts tends to increase, thus making it reasonable to determine and evaluate factors that facilitate or, in contrast, inhibit the trend. All the manifold of the factors can be brought to several generalized categories that are measured by monetary units and are related to expenditure of funds. Given this, the “carrier” of the expenses can differ within two large groups: a public sector – general government budget (including federal budget and the budgets of public social security funds) on the one hand, and a private sector on the other hand, represented by insurance companies and funds, corporations, and by individuals as well. For this case, it is interesting to determine which of the two sources of health expenditure funding has a greater influence on the integral health system performance indicator – expectation of life at different ages.
It is true to some extent that sharing the healthcare expenditure burden between public and private sectors stands inline with the concept of Public-private partnership (cooperation), but such a cooperation can be both voluntary and compelled, and it also requires verification in this research. Moreover, comparing the per capita total healthcare expenditure to the government expenditure and its revenue, one can derive an answer to another important question: the role of public-private partnerships in healthcare development and its contribution to health.
Methods
We employ several techniques of multiple regression analysis which is instrumental in obtaining quantitative measures of interdependency between several arguments and a function. Several assumptions were made prior to model identification:
1) functions – life expectation and out-of-pocket health expenditure – demonstrated causality towards the arguments;
2) the functions were assumed to have linear nature, according to their dynamics pattern and essential characteristics of the phenomena in focus: both life expectation and health expenditure in the long-run tend to linearization, while in short time frames they might look exponentially growing or declining. Moreover, current macroeconomic situation and the foreseen prospects show no signs of probable further increase of the functions growth rate.
Analysis in terms of modelling the relations between the functions and arguments was held according to the algorithm described in (Kolmakov et al., 2015). We introduced two representations of the models: “Executive” – with time series taken in levels, and “Authentic” – with the data in stationary representation (first-order differences). The “Executive” model, being more practice-oriented due to its greater explanatory power, is verified by the “Authentic” model which is correct in terms of spurious regression results elimination.
Regression models were characterized by R-squared and F-statistics, regression coefficients were cross-checked with their betas and appropriate p-level evaluation.
Data sources and manipulations
In order to verify the latter hypothesis, we are to run the survey using the following data.
1) Expectation of life at ages of 30-34; 35-40; 60-64, both females and males.The source of data is the World Health Organization.
2) Expenditure on health, in current prices (RUB) and in International USD (parity amended):
3) General Government revenue.
Data from sections “2” and “3” are retrieved from the “World Economic Outlook Database”.
Prior to any analysis, all the data series were checked for stationarity and multicollinearity. The data in levels representation indicate that the values are strongly biased, thus cross-correlated (correlation ratios exceed 0.93). The reason for such a result is rather obvious: most of the macroeconomic data are nonstationary due to the presence of autoregressive components combined with a trend or a seasonal pattern. Thus, the series had to be tested for the presence of a unit root and were modified according to the results. Otherwise, two constraints arise: a multicollinearity problem and spurious regression results.
Problem statement
We assume that there is a distinct interrelation between expectation of life at different ages and the expenditure on health from different sources, i.e. public and private, including out-of-pocket payments.We also have reasons to assume that a further change in the heath expenditure structure will result in roles redistribution within the partnership between the public and private sectors.
The hypothesis of this paper goes as the following: private healthcare expenditure is more efficient then the public expenditure, that is why the policy of social sector funding needs to be revised in order to give the population several incentives in exchange for the growing healthcare expenditure burden on individuals.
The roots of the hypothesis are found in several current processes that can be treated as non-characteristic for a social type of market economy. Thelatterprocessesinclude:
1. Life expectation in different age cohorts that had been decreasing till the end of 2003 is now constantly growing since 2004. The factors of the growth are quite numerous and include the increase of availability and quality of medical services, prosperity growth, positive change in labor conditions and contents.Life expectation during 2000-2014 increased annually by 0,48-0,9%, and in the period of permanent growth (2004-2014) it varied within 0,82% per annum (for females, 35-39 y.o.) and 1,47% per annum (males, 35-39 y.o.). The profiles of average life expectation can be extrapolated, but one should not expect for the prolonged linear growth of it due to some natural constraints.
It is clear that the quality of life is increasing synchronously. But to determine the true reasons for it, one needs to take a look at exogenous growth factors that include healthcare expenditure in its different interpretations.
2. Health expenditure is increasing, but its structure is changing permanently. i.e., starting from 1995, total health expenditure according to international comparisons methodology (using purchasing power parities) increased from 74,4 billion USD to 270,4 billion USD, which is 8,5% of the annual growth in average relative terms (fig. 1).
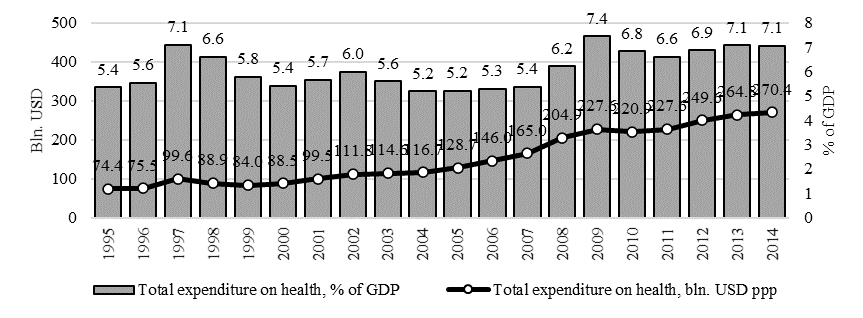
Notably, the relative amount (in terms of GDP proportion) was much more stable within the corridor between 5,2% and 7,4% (the average of 6,1%). Still, there is one peculiar fact that starting from 2004, there was a strong correlation between the growth of life expectation and out-of-pocket payments: the latter in 2001-2014 grew up from 30,34 billion of International USD (73,7% of total private health expenditure) to 124,0 billion international USD (95,92% of total private health expenditure – see fig. 2a). Along with that, per capita average private expenditure (fig. 2b) increased 10 times compared to its amountin 1996 (from 87,5 to 877,4 international USD per annum).
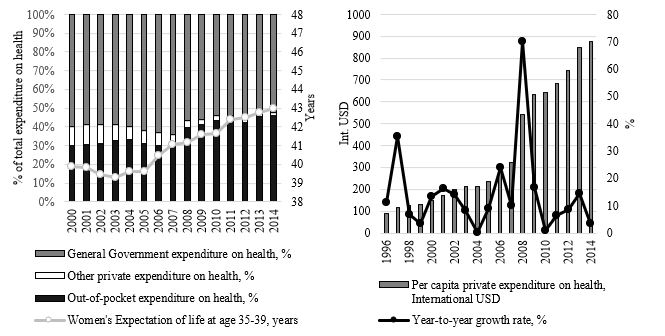
Obviously, the individuals pay more while the government’s proportion is constantly decreasing. The greatest matter of concern is the share of individuals’ expenditure within the whole private sector spending on health. It demonstrates the failure of private institutions of social security and insurance. The reasons for that include – as it is clear from fig. 2b – crises, during which the private share of health expenditure increased dramatically in response to the government slowdown. To tell more, the study of Murthy and Okunade indicates that per capita health expenditure in the USA depends strongly on per capita real income, the population percent above 65 years and the level of health care technology, measured as the level of Research & Development expenditure in health care (Murthy, & Okunade, 2016).
3. The general government revenue increases as health expenditure goes up that allows for the conclusion concerning some causality between social policy and economic development. Technically, during 2004-2014, the total government expenditure on health increased annually by 18,4% in current prices, while the revenue at the same time increased by 17,8% a year. Taken as the proportion of revenue, health expenditure sums up to the average of 10,2% between 8,7% in 2005 and 12,7% in 2009. In other words, the government does not cut the funding for its social obligations, but the growth rate of the demand for healthcare determines the gap between the demand and possibilities to finance it at the budget expense. People’s healthcare demand increases due to the changes in the socioeconomic life and improvement in the health technology (Yahaya et al., 2016). This is why, we face the coverage of current funding deficits by private sources, represented dominantly by individuals’ money. This situation is not unique since it is replicated in other sectors like agriculture, housing and utilities, etc.
In order to make a quality assessment of the present institutional disproportion effects, it is required to estimate the relative burden of out-of-pocket healthcare expenses by representing them as the percentage of the average monthly wage (table
Despite the relative stability of public healthcare expenditure, private spending is growing both in absolute and relative figures. As a result, the working people face growing pressure of healthcare payments as if it was an additional income tax rated in 2014 at 10,14% of an average wage after tax (individual income tax, 13%). This “quasi-tax” rate keeps growing since 2007 when it was minimal during the period of observation (5,75%).
It is clear that any further promotion of the Russian healthcare system efficiency and performance depends on individual income dynamics. But its growth can be useful only if the government, which is cutting down the budgets and has no potential to grow, introduces some incentives to the individuals. Actually Russia is no longer a country with no compulsory payments for medical insurance by individuals – those payments are in fact substituted by almost 100-percent out-of-pocket healthcare expenditure in the private sector.
Results and discussion
The modelling allowed one to derive the linear regression model showing that even in rescaled representation out-of-pocket healthcare expenditure does not provide any appreciable contribution to the quality of life andhealthsectorperformanceandefficiency. The “Executive” model indicated that the general government and individuals’ expenditure on health are statistically determined to make a contribution of no more than 19% to total variance of life expectation of males aged 35-39, as long as other factors, not included to the model, deliver 81,5% of the function variance (see table
The comparative performance of public and private health expenditure is in favor of the former. The standardized regression coefficients (Betas) indicate that public funds are 15,9 times more efficient in terms of contributing to healthcare system performance then out-of-pocket payments.
It is plausible, given the fact that individual spending cannot be considered equally distributed, especially considering healthcare financial burden shift to older cohorts. It is also obvious that individual expenditure averaging is not reliable in terms of unequal distribution of wealth. There is also a problem of spatial inequalities, which is discussed and revealed in.
One of the Authentic model results is the negative interrelation between healthcare efficiency and performance integral indicator and out-of-pocket expenditure growth. In its strength but no in the vector, it is equal to public expenditure. The interpretation is rather rational: for the most of the individuals, out-of-pocket healthcare expenditure is the barrier for development, or some kind of a social tax with selective scope.
Study of interrelation between individual and public healthcare spending, and general government revenue allowed one to determine the fact that according to Executive and Authentic models, government revenue and individual spending are counter-phase to each other (see table
The explanation is rather traditional for the social state situation: growing public revenue is the reason for easing-off individual spending, due to the ratios between public healthcare expenditure and revenues are relatively permanent. In contrast, decreasing revenue is usually not correlated with healthcare services demand, and in terms of crisis, for example, it acts as a driver for the demand growth, thus stimulating individuals to spend more (Dmitriev, & Drobyshevsky, 2015).
Conclusion
The analysis allowed us to reject the hypothesis of the research. Private healthcare expenditure in terms of contribution to the life expectation growth is much less efficient compared to public expenditure. The verification can also be found in (Bustamante, 2010), showing that regressive out-of-pockethealth care expenditures stimulate quality and availability development in originally centralized health infrastructures, like the one we have in Russia.
The obtained result allows us to conclude that Russia’s current situation of a gradual decrease of the share of public-funded health expenditure can hardly be the success story of public-private partnership.Instead of efficient private institutions, the burden of funding is held by individuals who have to pay more. Therefore, out-of-pocket health expenditure can be treated as “quasi-tax”, rated at 10,14% of the average after tax income. The good way to go in such a realm, according to Luck et al., (2014), is to improve the quality of healthcare by implementing pay-for-performance principles of funding both in private and public sectors.
References
- Dmitriev, M., & Drobyshevsky, S. (2015). Russian economy as the hostage of high oil prices. In The international monetary system, energy and sustainable development pp. 191-252.
- Kolmakov, V. V., Polyakova, A. G., & Shalaev, V. S. (2015). An analysis of the impact of venture capital investment on economic growth and innovation: evidence from the USA and Russia. Economic Annals, Volume LX(207), 7-37.
- Kookueva, V. V. (2014). Trends of financing sustainable development of rural areas in Russia. Life Science Journal11(6 SPEC. ISSUE), 310-314.
- Luck, J., Peabody, J. W., DeMaria, L. M., Alvarado, C. S., & Menon, R. (2014). Patient and provider perspectives on quality and health system effectiveness in a transition economy: Evidence from Ukraine. Social Science and Medicine114, 57-65.
- Murthy, V. R., & Okunade, A. A. (2016). Determinants of U.S. health expenditure: Evidence from autoregressive distributed lag (ARDL) approach to cointegration. Economic Modelling59, 67-73.
- Polyakova, A. G., & Simarova, I. S. (2014). The conceptual model of a region development administration considering the level of spatial relatedness. Economy of Region2, 32-42.
- Schoen, C., Davis, K., How, S., & Schoenbaum, S. C. (2006). U.S. health system performance: A national scorecard. Health Affairs26(6), 457-475.
- Shaytura, S. V., Stepanova, M. G., Shaytura, A. S., Ordov, K. V., & Galkin, N. A. (2016). Application of information-analytical systems in management. Journal of Theoretical and Applied Information Technology, 90(2), 10-22.
- Vargas Bustamante, A. (2010). The tradeoff between centralized and decentralized health services: Evidence from rural areas in Mexico. Social Science and Medicine71(5), 925-934.
- Yahaya, A., Nor, N. M., Habibullah, M. S., Ghani, J. A., & Noor, Z. M. (2016). How relevant is environmental quality to per capita health expenditures? Empirical evidence from panel of developing countries. SpringerPlus5(1).
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
20 July 2017
Article Doi
eBook ISBN
978-1-80296-025-9
Publisher
Future Academy
Volume
26
Print ISBN (optional)
Edition Number
1st Edition
Pages
1-1055
Subjects
Business, public relations, innovation, competition
Cite this article as:
Kolmakov, V. V., & Polyakova, A. G. (2017). Health Sector Performance Under Public-Private Partnership. In K. Anna Yurevna, A. Igor Borisovich, W. Martin de Jong, & M. Nikita Vladimirovich (Eds.), Responsible Research and Innovation, vol 26. European Proceedings of Social and Behavioural Sciences (pp. 436-443). Future Academy. https://doi.org/10.15405/epsbs.2017.07.02.56

