Abstract
Background: Schizophrenia is a complex chronic disease that turns the affected person into a dependent and disorganized patient. This pathology is responsible for a major burden on the family members who are in charge of taking care of that person. Objectives: to analyze to what extant can socio-demographic, clinical and environmental variables interfere with the burden felt by family members who live with someone suffering from schizophrenia; to analyze the relationship between a depressive mood state and the burden on the family members who live with a person suffering from schizophrenia. Material and methodology: quantitative and non-experimental, cross-sectional, descriptive and correlational study. The data collection was done through socio-demographic questionnaires; Vaz Serra and Pio Abreu’s Portuguese version of Beck Depression Inventory (1973); Zarit Burden Interview adapted by Sequeira (2007). 95 informal caregivers taking care of schizophrenic patients were assessed. Results: the participants are mainly female (66%), aged 40 or over (79%) and 36 % are the patients’ mothers. Gender, age and existing family ties variables interfered significantly with the impact caused on the caregiver’s burden. There was a statistically significant correlation between the depressive symptomatology and the burden experienced by the family caregivers. Conclusion: the family/ informal caregiver experience several difficulties when they have to go through a daily process of taking care of a family member suffering from schizophrenia. This situation may cause exhaustion, conflicts, emotional suffering and even depressive symptomatology. This burden of care grows stronger as the patients are older, when they are male and when there are no families ties binding patient and caregiver. These variables must be taken into account in these caregivers’ service plans.
Keywords: Schizophrenia, family, informal caregiver
Introduction
The disease and the social pressure turn a schizophrenic patient into a significantly dependent person. The loss of some basic skills, the neurocognitive deficit and disorders, the therapy and its collateral effects, the symptomatology, the social significance associated with such a disease (feeling of stigmatization), among other factors, make these patients more dependent on their informal caregivers. This role is mostly played by relatives (Carvalho, 2011).
Schizophrenia, an emblematic entity in the field of Psychiatry and Mental health care, is among the top ten causes of long-term social burden, showing significant prevalence rates among world population.
Schizophrenia is responsible for the increase in the average number of days a patient will need to spend in the psychiatric services in order to be treated (35,4 days when 20 is the average number of days a patient suffering from other mental illnesses will be spending during his hospitalization in the general psychiatric services). Schizophrenia was the main cause that led patients to look for health care.
In times of crisis, family members have to learn again how to deal with a series of problems like the patient’s decrease in self-care, his aggressiveness, odd behaviours, refusal to follow the treatment, social isolation, mood changes, anxiety, substance abuse, bizarre behaviours and even the risk of suicide (Yacubian & Neto, 2008). According to the same authors the schizophrenic patient’s behaviours associated with the lack of information about the disease are frequent causes of stress-related problems and make the family more likely to develop situations of anxiety, rage and depression which will certainly increase the caregivers’ burden. Rudge and Morse (2007) also refer to the emotional disturbance experienced by the caregiver, his worries, his negative feelings and the discomfort that comes from the fact that he has to take care of a schizophrenic family member. Generally speaking, caregivers look at the action of taking care of someone as something they are forced to do. This perspective increases the feeling of burden and of constant concern that the people they are taking care of might have to be institutionalized (Rudge & Morse, 2007; Teixeira, 2005).
When a caregiver is a member of the patient’s family, it usually reduces the possibility of a psychotic relapse during treatments.
McFarlane et al. (2003) show that the use of additional interventions from the patient’s family in a period of nine to twelve months may reduce relapse rates by four during a one year period and reduce by 20% to 50 % the risk of readmission to a hospital during a two year period.
The family psycho-educational interventions are seen as the most effective. Results show that these interventions meet families’ needs and expectations and improve the patient’s situation and the family’s well-being as a whole (Gonçalves-Pereira et al., 2006). These interventions reduce the level of caregiver’s stress and provide information about the illness and about possible types of treatment, improving the communication patterns with the informal caregiver and the coping strategies, as well as the caregiver’s abilities and skills he will use to solve possible problems (World Health Organization, 2002, quoted by Gomes, 2008).
Methodology
We choose to use a quantitative, analytical descriptive and correlational methodology to explore the relationships between variables which will allow a better understanding of such a phenomenon. The data collection was performed between June and December 2014 and our intention was to analyse to what extent the socio-demographic, clinical and environmental variables can interfere with the burden experienced by the family members who live with a person suffering from schizophrenia and to analyse the relationship between depression and the burden experienced by the family members who live with a person suffering from schizophrenia.
According to the objectives we had outlined, the following research design was created:
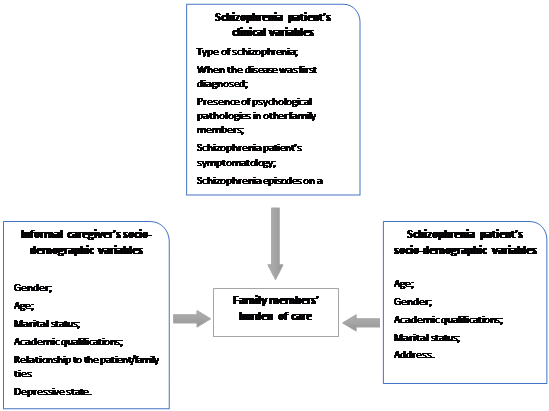
95 family members who live with a person suffering from schizophrenia were interviewed. The data collection instrument was a socio-demographic questionnaire that allowed the collection of relevant data about the socio-demographic profile of the family members who live with someone suffering from schizophrenia.
Clinical variables which make it possible to create the patient’s clinical portrait: when the disease was first diagnosed; the kind of medication the patient takes; other psychiatric diseases diagnosed before schizophrenia; psychiatric pathologies diagnosed in other family members; schizophrenia patient’s symptomatology; how often do episodes of schizophrenia occur on a monthly basis…
Environmental variables, five questions through which one can gather enough information to establish the profile of the person who suffers from schizophrenia: age, gender, academic qualifications, marital status and address.
1961 Mendelson, Mock e Erbaugh’s Beck Depression Inventory- BDI ( 1973 Vaz Serra & Pio Abreu’s Portuguese version), a 21 question self-report inventory which main goal is to measure the severity of depression symptoms. The depressive symptomatology is organized into six different types of symptoms: affective, cognitive, motivational, delirious, physical and functional (sleep pattern, appetite, weight and libido).
Caregiver’s Burden Interview: this document was translated and adapted to the Portuguese population by Sequeira (2007). It allows to assess the informal caregivers’ objective and subjective burden of care and helps explore the negative effects that such situation has on those caregivers’ lives: on a social, personal, financial, and emotional planes as well as the way relationships will be affected by this burden.
Research Questions
Based on the above, there were the following initial questions:
What factors influence the burden of family members cohabiting with the person schizophrenia?
That sociodemographic, clinical and contextual caregiver to interfere with overload of family cohabiting with the person with schizophrenia.
Purpose of the study
In order to answer the research questions, the following objectives were defined:To analyze to what extant can socio-demographic, clinical and environmental variables interfere with the burden felt by family members who live with someone suffering from schizophrenia; to analyze the relationship between a depressive mood state and the burden on the family members who live with a person suffering from schizophrenia.
Results
32 of the caregivers we interviewed are male (34%) and 63 are female (66%). The majority of the participants are 40 or over (n=75; 79%), while the other participants are 39 or younger (21%). As far as their marital status is concerned we could witness that, whether they were male (62,5%) or female (61,9%), participants were mostly married couples or unmarried partners who didn’t graduate from high school. When it came to the kind of relationship which exists between the caregiver and the schizophrenic patient, the highest percentage went to the role played by the mother (55, 6%) and by the father (50%). Brothers (25%) were next in the group of male participants and wives (14,3 %) in the female group.
We got statistically significant differences (p=,000) ( Table 1).
People’s relatives were diagnosed with schizophrenia 21 years ago or before and 66,3 % of the cases studied suffer from paranoid schizophrenia.
The majority of the male patients (68,6%) and of the female patients (64,5 %) diagnosed with schizophrenia are 40 or over. The majority lives with close relatives.
From the data collected, we saw that, whether they’re male or female, caregivers show signs of moderate depression (37,5 % and 63,5 % respectively). The cases in which depression does not exist are less representative showing statistically significant differences (p=0,032) to X2=6,868. This shows that depression is more likely to affect female and older people (p=0,002 and X2=12,5889).
As far as academic qualifications are concerned, we can conclude that participants with the lowest qualifications are more likely to suffer from depressive illnesses (p=0,027 to X2=7,202).
We can stress out that, according to our analysis, 100% of the people we interviewed and who have experienced light burden don’t show any depressive symptoms, while 85, 90 % of the sample who have experienced intense burden show signs of depressive symptomatology. This variable shows highly significant statistical differences (p=0,000) to X2=15,296.
Female caregivers got higher rates in all the burden factors when they are compared to male caregivers; however the differences are only statistically significant when it comes to – (p=0,030).
Single participants aged 40 or over were those who showed higher rates in all the burden factors, but factor 4-. Participants aged 39 or under were those who showed a higher rate in this burden factor.
The participants who have relatives suffering from a mental illness were those who show stronger burden in all factors but factor 3- and Factor 4-. For those factors the highest average went to the participants who don’t have any relatives diagnosed with schizophrenia. However there was no statistical significance in the results displayed.
Participants who take care of a 39 years old or younger schizophrenic patient were those who showed higher burden in all the assessed factors, but factor 3-We could see that the statistical differences are very significant for factor 1-(p=0,001) and significant for Global Burden (p=0,010).
As far as the schizophrenic patient’s gender was concerned, we witnessed higher burden in female caregivers in all burden factors but statistical significance was found only in factor 1-(p=0,030).
Through Mann- Whitney – U Test, we discovered that higher burden is found in caregivers whose schizophrenic relative is not married. This is evident for all the factors, although we don’t find any statistically significant differences.
As far as the schizophrenia patient’s address is concerned, we can see that the highest average results belong to participants whose schizophrenic relative lives in an urban surrounding. This is evident for all factors although there’s no statistical significance.
We tried to investigate the way the burden of care and its dimensions were influenced by the depressive symptomatology global score. We found the existence of positive correlations for all factors. This conclusion suggests that the increase in the depressive symptomatilogy scale score leads to an increase in the scores of the burden factors and global burden. As far as the global burden is concerned, we got a positive correlation (general r=0,498 – moderate positive association) which reveals that burden feelings decrease as depressive symptomatology increases. These associations show significant statistical differences (p<0,01) and highly significant ones (p<0,001).
These results suggest that there is a correlation between depressive symptomatology and the burden experienced by informal caregivers who deal with schizophrenic patients.
Discussion/conclusion
Several Studies have showed that the presence of a mental patient in the family is an important burden for the family members (Jungbauer et al., 2003).
This burden may, eventually, cause psychological disorders like anxiety and depression. These disorders affect more often women who take care of their mentally ill children or husbands. Because of the chronic nature of such illness, these family members are more likely to suffer from the stress that comes from the daily experience of looking after someone affected by a terrible disease. This may, in the end, affect their own mental health (Martens and Addington, 2001; Rammohan et al., 2002).
Figueiredo (2007) defined the caregiver’s profile: his gender and age (usually a female between 45 and 60); the kind of family ties he has with the patient (husband/wife, son or daughter, friends or neighbours when there’s no next of kin); his marital status (married) and the geographic vicinity (living in the same house or close to the patient). Despite this fact, reality shows that male participation in this kind of tasks is more and more frequent. Sequeira (2007) identifies four informal caregiver’s characteristics: the family ties that bind caregiver and patient, the fact that both caregiver and patient live together, their gender and the conditions caused by the kind of relationships that exist between parents and children. Dias (2011) in his study proved that the majority of caregivers were female (78,40 %). Most of them were the patients’ mothers (62,20%) and they show an average age of 59,14. Those facts confirm what this study has showed so far.
As far as informal schizophrenic caregivers’ burden of care is concerned, it’s a fact that the female participants got higher rates in all burden factors, when they are compared to male elements. Those results are in agreement with those found when the issue of depressive symptomatology was studied. In both cases female participants showed a deeper depressive symptomatology and experienced deeper burden. Other studies (Frias, Tuokko & Rosenberg, 2005; Giacomin et al., 2005; Mehta, 2005) also show that women present a lower self-esteem and higher levels of anxiety and depressive symptomatology. All these factors have a strong impact on their quality of life. Female caregivers who deal with schizophrenia patients show deep weariness (physical but mainly psychological weariness) which is deeper and more consuming when the patients are their children or husbands. This deep fatigue is more than understandable since this task has a deep impact on the different dimensions of their lives (physical, psychological, social, professional and economic) that will lead to deeper burden. To them, there is a moral obligation that leads to a higher commitment to the sick person which will increase the levels of stress, namely during any psychotic crisis. The burden, in all its different dimensions, is also influenced by the amount of medical consultations and psychiatric hospitalizations.
Keeping this in mind, one can say that the family member who assumes the role of caregiver will have to develop several tasks that will be closely influenced by the receiver’s needs (Martins, 2006). New, unknown and unpredictable tasks that will add more efforts and more worries to those which already exist in his daily life and that will trigger a multitude of feelings like fear, guilt, uncertainty about what the future will bring, responsibility to the patient, feelings of emotional discomfort, distress and sadness that threatens his well-being (Fernandes & Garcia, 2009; Pinquart & Sorensen, 2006; Silveira, Caldas & Carneiro, 2006).
This role as caregiver will bring important changes into individual and family life. Taking care of someone who suffers from schizophrenia forces a person to spend a lot of time and a lot of energy, to have to go through new tasks that can sometimes be unpleasant and uncomfortable during periods of time which length is usually unpredictable (Pinquart & Sorensen, 2006). The consequences that come from this caregiver’s role can be felt at a physical, emotional and social levels and can manifest themselves in changes felt by the caregivers. These changes have to do with the difficulty in achieving complex tasks, changes in their self-care, changes in their sleeping patterns, insomnia and constant weariness, irritability, depression, emotional stress, lower social life, frustration, fear, lack of interest in living, discouragement and a poor quality of life (Fernandes & Garcia, 2009a; Sena & Gonçalves, 2008).
We have to point out that the participants who take care of younger schizophrenic patients (≤ 39) obtained the highest rates in all burden factors, but factor 3-In this factor, the higher rates were associated with users aged 40 or over, although the only factor statistically significant is factor 1- (p=0,001)
Martins (2006) found out that older caregivers feel less satisfied with this role and with their sick family member and that they feel that this task has dire consequences in their personal life. This conclusion is in agreement with the data collected in this investigation. Taking this information into account, and according to Sousa et al. (2006), caregivers who take care of mentally ill people suffer from structural, procedural, cognitive and emotional discomfort, which will increase the burden they experience. When the time comes to assume the role of caregiver, no one knows exactly what to expect and what will be expected of them. Taking care of a schizophrenic person involves spending a lot of one’s personal time and energy and often performing new tasks that are, most of the time, unpleasant and uncomfortable.
Physical, emotional and social burden is directly associated with some of the caregiver’s characteristics: his/her age, gender, his family ties with the patient, the lack of support from Healthcare services and the importance this person gives to his/her role as caregiver, his/her commitment with his/her role (Fernandes & Garcia, 2009b; Giacomin, Uchoa & Lima Costa, 2005; Martins, 2006).
We witnessed that female and older caregivers are more likely to feel a stronger sense of depression. These results are in agreement with those presented by Basheer et al (2005), Guedes (2008) e Maurin e Boyd (1990). In both cases, the conclusion was that older informal caregivers who take care of schizophrenic patients present higher levels of burden and higher levels of depressive symptomatology.
We could also witness that participants with lower academic qualifications were more likely to experience depressive symptomatology. These results may have to do with the fact that people with lower academic qualifications have little access to information and therefore fewer opportunities to gather a vaster knowledge concerning their relative’s disease and the way they should deal with that condition and with the person who suffers from it.
Our professional experience has showed us that society in general has quite a negative opinion about schizophrenia. People usually feel afraid or even threatened and some of them think that people who suffer from that disease should be locked away in psychiatric hospitals, kept in their homes or under the influence of sedatives.
We could see that all the participants who have experienced moderate burden of care don’t show any depressive symptoms, while 85, 90 % of the participants in our survey who have experienced intense burden of care show depressive symptomatology. There are highly significant statistical differences (p=0,000) to X2=15,296 which suggests that the subjects who have experienced intense burden are more likely to manifest a depressive symptomatology. These results are in agreement with those found by Train et al. (2005) and Dias (2011). In their opinion there is a strong relationship between high levels of burden and depressive symptomatology in caregivers who deal with mentally ill patients.
In conclusion, when we have to deal with a relative’s disease, like schizophrenia for instance, the caregiver must face multiple challenges that require a strong adaptability, the capacity to mobilize certain resources (coping) and the capacity to take care of ourselves, which means that we must have the capacity to manage the different aspects of our own life. This is why the role of healthcare professionals is so important: important to promote or protect people’s health and to help reduce those people’s physical and psychological burden. In this context, the therapeutic relationship becomes the nurse’s most powerful tool and can be used to work with the schizophrenic patient, as well as with his caregivers: helping solve the conflicts that come from living with a schizophrenic member of our family, helping members of the family fight and reduce their anxiety, giving them all the conditions they need to fight against the destructive social forces that can interfere directly with their quality of life, promoting cohesion and the feeling of family identity in order to develop a sense of sharing that will reduce the burden experienced by a single caregiver.
Those healthcare professionals must precociously identify signs that can predict the caregiver’s weariness so that they can act and give information to any healthcare support network thus preventing more serious consequences.
References
Basheer, R., Brown, R., Ramesh, V., Begum, S., & McCarley, R. W. (2005). Sleep deprivation-induced protein changes in basal forebrain: implications for synaptic plasticity. Journal of Neuroscience Research, 82(5), 650-658. doi:
Carvalho, J. C. M. (2011). Esquizofrenia e família: repercussões nos e filhos e cônjuge (Tese de doutoramento, Universidade do Porto). Acedido em https://repositorio-aberto.up.pt/bitstream/10216/63724/2/Esquizofrenia%20e%20Famlia%20repercusses%20nos%20filhos%20e%20conjuge.pdf
Dias, E. A. (2011). Sobrecarga vivenciada por familiares cuidadores de pacientes esquizofrénicos e sua relação com a depressão (Dissertação de mestrado, Universidade Nova de Lisboa). Acedido em https://run.unl.pt/handle/10362/5932
Fernandes, M. G. M., & Garcia, T. R. (2009). Atributos da tensão do cuidador familiar de idosos dependentes. Revista da Escola de Enfermagem da USP, 43(4), 818-824. Acedido em http://www.scielo.br/pdf/reeusp/v43n4/a12v43n4.pdf
Fernandes, M. G. M., & Garcia, T. R. (2009). Determinantes da tensão do cuidador familiar de idosos dependentes. Revista Brasileira de Enfermagem, 62(1), 57-63. Acedido em http://www.scielo.br/pdf/reben/v62n1/09.pdf
Figueiredo, D. (2007). Prestação familiar de cuidados a idosos dependentes com e sem dependência. Dissertação de Doutoramento em Ciências da Saúde, Secção Autónoma de Ciências da Saúde, Universidade de Aveiro.
Frias, C. M., Tuokko, H., & Rosenberg, T. (2005). Caregiver physical and mental health predicts reactions to caregiving. Aging Mental Health, 9(4), 331-336. doiI:
Giacomin, K. C., Uchoa, E., & Lima-Costa, M. F. (2005). Projeto Bambuí: A experiência do cuidado domiciliário por esposas de idosos dependentes. Cadernos de Saúde Pública, 21(5), 1509-1518. Acedido em http://www.scielo.br/pdf/csp/v21n5/24.pdf
Giacomin, P. R., Wang, H., Gordon, D. L., Botto, M., & Dent, L. A. (2005). Loss of complement activation and leukocyte adherence as Nippostrongylus brasiliensis develops within the murine host. Infection and Immunity, 73(11), 7442-7449. doi:
Guedes, A. S. M. (2008). Avaliação do impacto da perturbação mental na família, e implementação de um programa psicoeducacional (Dissertação de mestrado, Universidade do Porto). Acedido em http://repositorioaberto.up.pt/bitstream/10216/23753/2/Avaliao%20do%20impacto%20da%20perturbao%20mental%20na%20familia%20e%20implementao%20de%20um%20programa%20psicoeducacional.pdf
Jungbauer, J., Wittmund, B., Dietrich, S., & Angermeyer, M. C. (2003). Subjective burden over 12 months in parents of patients with schizophrenia. Archives of Psychiatric Nursing, 17(3), 126-134. doi:
Martens, L., & Addington, J. (2001). The psychological well-being of family members of individuals with schizophrenia. Social Psychiatry and Psychiatric Epidemiology, 36(3), 128-133. doi:
Martins, I. (2006). AVC – Qualidade de vida e bem-estar dos doentes e familiares cuidadores. Loures : Framausau.
Maurin, J. T., & Boyd, C. B. (1990). Burden of mental illness on the family: A critical review. Psychiatric Nursing, 4(2), 99-107. doi:
Mehta, S. R., Cannon, C. P., Fox, K. A., Wallentin, L., Boden, W. E., Spacek, R., … Yusuf, S. (2005).
Mueser, K. T., & McGurk, S. R. (2004). Schizophrenia. Lancet, 363(9426), 2063-2072. doi:
Pinquart, M., & Sörensen, S. (2006). Helping caregivers of persons with dementia: which interventions work and how large are their effects? International Psychogeriatrics, 18(4), 577-595. doi: DOI:
Portugal, Ministério da Saúde, Alto Comissariado da Saúde, Coordenação Nacional para a Saúde Mental. (2008). Plano Nacional de Saúde Mental 2007-2016. Lisboa: CNSM.
Portugal, Ministério da Saúde, Direcção Geral de Saúde. (2007). Reestruturação e Desenvolvimento dos Serviços de Saúde Mental em Portugal: Plano de Acção 2007-2016. Lisboa: CNRSSM. Acedido em http://www.hmlemos.min-saude.pt/docs/PNacSM2007.pdf
Rammohan, K. W., Rosenberg, J. H., Lynn, D. J., Blumenfeld, A. M., Pollak, C. P., & Nagaraja, H. N. (2002). Efficacy and safety of modafinil (Provigil®) for the treatment of fatigue in multiple sclerosis: A two centre phase 2 study. Journal of Neurology, Neurosurgery & Psychiatry, 72(2), 179-183. doi:
Routine vs selective invasive strategies in patients with acute coronary syndromes: A collaborative meta-analysis of randomized trials. JAMA, 293(23), 2908-2917. doi:
Sena, E. L. S., & Gonçalves, L. H. T. (2008). Vivências de familiares cuidadores de pessoas idosas com doença de Alzheimer: Perspectiva da filosofia de Merleau-Ponty. Texto Contexto Enfermagem, 17(2), 232-240. Acedido em http://www.scielo.br/pdf/tce/v17n2/03.pdf
Silveira, T. M., Caldas, C. P., & Carneiro, T. F. (2006). Cuidando de idosos altamente dependentes na comunidade: Um estudo sobre cuidadores familiares principais. Cadernos de Saúde Pública, 22(8), 1629-1638. Acedido em http://www.scielo.br/pdf/csp/v22n8/11.pdf
Sousa L. Figueiredo, D. & Cerqueira, M. (2006). Envelhecer em família – Os cuidados familiares na velhice. Porto.
Train, G. H., Nurock, S. A., Manela, M., Kitchen, G., & Livingston, G. A. (2005). A qualitative studt of the experiences of long-term care for residents with dementia, their relatives and staff. Aging and Mental Health, 9(2), 119-128. doi:
Vaz Serra, A., & Pio Abreu, J. L. (1973). Aferição dos quadros clínicos depressivos. I: Ensaio de aplicação do "Inventário Depressivo de Beck" a uma amostra portuguesa de doentes deprimidos. Coimbra Médica, 20, 623-644.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
31 July 2016
Article Doi
eBook ISBN
978-1-80296-012-9
Publisher
Future Academy
Volume
13
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-462
Subjects
Health psychology, psychology, health systems, health services, ocial issues, teenager, children's health, teenager health
Cite this article as:
Cabral, L., Almeida, M. J., Ferreira, M., Gonçalves, A., & Duarte, J. (2016). Caregivers’ burden experienced by relatives living with a person suffering from schizophrenia. In S. Cruz (Ed.), Health & Health Psychology - icH&Hpsy 2016, vol 13. European Proceedings of Social and Behavioural Sciences (pp. 128-138). Future Academy. https://doi.org/10.15405/epsbs.2016.07.02.11

