Abstract
This study aims to highlight the close relationship between movement games and respiratory function in students with hearing impairments. Particularly, the paper draws attention to the lack of specific syllabus and informative material on how to carry out the physical education lesson in special schools. Addressing this topic has involved conducting a pedagogical experiment based on the hypothesis that the substantial use of movement games for students with hearing impairments will result in the optimisation of their respiratory function. The methods used to achieve the study were: documentation, pedagogical observation, experiment, test method (tests, controls and measurements), statistical and mathematical methods for data processing and interpretation, comparative method and graphical method. The experiment was conducted over a 7-month period and involved students with hearing impairments in two 5th grades (11-13 years old). After the initial testing, the experiment classroom worked according to a programme including several movement and sports games, and the control classroom worked according to the adapted school syllabus. Final testing was based on identical controls for both groups. The respiratory function of the participating students was tested with the spirometer at the Interdisciplinary Research Centre of UNEFS Bucharest and was interpreted by a specialist physician from the Pneumophthisiology Ambulatory Care. The conclusions largely confirm the research hypothesis. Thus, the use of movement games in the physical education lesson for students with hearing impairments clearly improves their respiratory capacity, forced vital capacity and the degree of airflow limitation.
Keywords: Hearing impairmentsschool physical educationmovement gamesrespiratory function
Introduction
Pulmonary tests are valuable tools for detecting and investigating respiratory pathologies. Although they do not establish a diagnosis, they can serve to indicate one, being relevant for various types of abnormalities. The general rules for conducting and interpreting these tests have been published and are identical for the European Respiratory Society and the American Thoracic Society.
Such a test with special valences is spirometry, which helps to determine, in a relatively simple way, the parameters of lung capacity, lung volume and respiratory flow (inhalation, exhalation), either to diagnose respiratory pathologies (such as asthma, chronic obstructive pulmonary disease - COPD) or to monitor their progression.
For deaf students, the physical education lesson is the school subject allowing them to be equal to those with normal hearing and, at the same time, is a source of externalisation. The idea of this study has emerged from a simple remark, according to which children who use their lungs to shout, sing or just ‘argue’ during the physical education lesson seem to have better pulmonary capacity than the other deaf, who are ‘good’ children.
General considerations about students with hearing impairments
At an official level, in order to diminish the incidence of their impairment, the deaf accept the status of ‘disabled’, although they are actually part of a special world.
In psycho-pedagogical terms, the child with hearing impairments is in a special situation, because they cannot perceive a certain category of physical stimuli, therefore their sensory experience related to the object world will be poorer by far. Moreover, deafness restricts not only the child’s auditory field, but also their early social interrelation that underlies the communication process (Stanojevic, Quanjer, Miller, & Stocks, 2013)
The physical development of people with hearing impairments is close to that of the normal-hearing people of the same age, but there are noted slight coordination deficiencies, less developed static balance, low indices of resistance to long-term efforts etc., disorders which are partially corrected (for a high percentage of children) by the education system (Arunovic & Pantelic, 1997).
Motor, postural and even emotional delays result from the non-stimulation and non-practice of the act of speech. The fact that they do not talk (muteness), along with the lack of movement, lead to low indices of their lung capacity. Consequently, deaf children will hardly cope with long-term efforts and therefore their effort resistance will be diminished. (Wang et al., 1993)
All this explains the magnitude of the inventory of specific objectives pursued through physical education, of which the primordial ones are: developing the chest muscles and their elasticity, educating breathing and increasing vital capacity, starting/continuing the ‘de-muting’ and the social integration process (Beaussant, 2003).
On the mental plane, the deaf child’s courage, even boldness, must be emphasised; they never refuse a new activity, and their desire to know and learn is much more obvious than in those with normal hearing. Emotionally, the deaf child is certainly much closer to the adult: the demonstrations of joy and affection, as well as sincerity are common among them. (Craft, 2000)
Problem Statement
Children with hearing impairments are not encouraged to speak and therefore are unaware of the normal changes caused by air pressure on the respiratory tract. The impact of factors such as speech and shout on the development of respiratory function has not been sufficiently investigated. This experimental study starts from the hypothesis that the substantial use of movement games for students with hearing impairments will result in the optimisation of their respiratory function, with its many positive effects.
In this regard, standard spirometry was used to analyse forced vital capacity (FVC) and the amount of air exhaled in the first second (FEV1). The spirometry equipment was calibrated every time, this action being performed by two people with experience in the field, and the instruction of deaf children was provided by their physical education teacher.
Research Questions
We want to check whether the respiratory function of students with hearing impairments can be improved by the intensive use of movement games in the physical education lesson.
Purpose of the Study
The research aims to improve the instructive-educational process for the training of students with hearing impairments by focusing on the use of movement games, while taking into account their age particularities and the specific working conditions.
Research Methods
Study design and subjects
The pedagogical experiment was conducted between October 2015 and May 2016 at the Special Middle School for Deaf no. 1 in Bucharest and involved a number of 18 students in two 5th grades. This category included girls and boys of different chronological ages (11 to 13 years), forming a single group based on the main criterion, puberty, with the major changes produced in the child’s body. There were no significant differences between morphological characteristics, intellectual development and socio-economic factors. Therefore, the results of this research most likely reflect the effects of physical activity on respiratory function.
The 9 students (2 girls and 7 boys) in the control group worked according to the school syllabus, with standard exercises: sprints for the ‘speed’ quality, jumping for vertical jump, flexions and extensions for abdominal and back muscles, and long run for aerobic endurance. With the same objective (the development of motor qualities), the other 9 students (5 girls and 4 boys) experienced a programme with several movement and sports games that were adapted (in terms of rules and way of performing them), in the sense of their simplification, and were given funny names. This urged to the vocal externalisation of feelings and encouraging classmates. The amount of games within the lessons was about 35 minutes (75-80%) of the time allotted to the lesson, as much as the activity of the control group.
In order to make sports classes and sports games as attractive as possible for these students with special needs, it is vital to take into account the affinities of each one, which is why the lesson planning included games preferred by each child.
The functional testing of students took place at the “Dr Alexandru Partheniu” Interdisciplinary Research Centre of UNEFS Bucharest, at the beginning and the end of the school year, using the spirometry method.
Spirometry
Spirometry is a very simple painless examination, which remains the main test for respiratory function due to its parameters that are more objective than pulmonary auscultation or symptom description. In medical terms, it represents a highly accurate paraclinical investigation with a predictive value, used to diagnose and classify the condition that causes the pulmonary function alteration. The main benefit of spirometric testing is the detection of abnormalities in the respiratory system, even when there are no obvious signs or symptoms of a disease.
The spirometer measures the volume of air that fills, goes into and out of the lungs. When connected to a computer, the results are also displayed in graphical form, representing the volume as a function of time and the flow volume (spirogram).
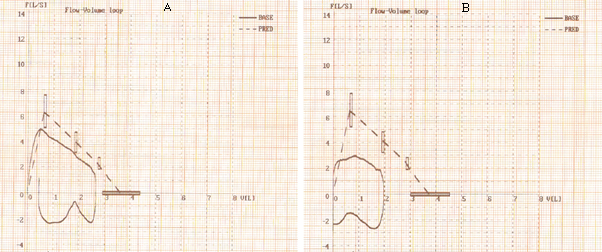
The spirogram is used by the physician to compare the values between them, on the one hand, and with the ideal figures (for age, height, gender, race), on the other hand. The flow-volume curve, the graphical representation of the degree of airflow limitation - the FEV1/FVC ratio (Figures
Findings
The two groups were tested at the beginning and the end of the experiment, and the results are found in Tables
the total volume of air a patient is able to exhale for the total duration of the test during maximal effort: FVC (forced vital capacity) (Johnson & Theurer, 2014);
the total volume of air a patient is able to exhale in the first second during maximal effort (FEV1 - forced expiratory volume in one second) (Johnson & Theurer, 2014);
the degree of airflow limitation: the FEV1/FVC ratio, according to the Morris/Polgar equation. A low FEV1/FVC ratio shows that, because of airway narrowing, the affected person needs more time to achieve full exhalation.
Forced vital capacity (FVC) and FEV1 are influenced by age, height, gender and ethnicity. In our study, the index scores for the spirometry test indicate a reduction in the overall lung dysfunction for both groups. However, the mean difference between the final and initial testing, with higher values for the experimental group (23.72% versus 18.36%), and the fact that 77.7% of the experiment group students versus 66.6% of the control group students have increased their FVC are additional arguments to support the research hypothesis.
Forced expiratory volume in one second (FEV1) is used as a percentage of the value found. Based on this parameter, the physician can determine the degree of reduction in the rate at which the air passes through the bronchi, assessing the severity of each abnormality (Table
Physicians often analyse FVC and FEV1 separately and then calculate the FEV1/FVC ratio. The higher the FEV1/FVC ratio (in the absence of pulmonary disease), the healthier the lungs are. A low ratio suggests the airway obstruction. (Table
The degree of airflow limitation (FEV1/FVC), also called BRI (Bronchial Reactivity Index) is comprised between 70-80% in the normal adult, with the specification that a score below 70% indicates a restriction of airflow and possibly COPD (chronic obstructive pulmonary disease).
In the final testing, the FEV1/FVC ratio has very good and good scores (the mean is 98.81% for the experimental group and 77.65% for the control group), and the decrease in the BRI scores for 27.7% of the total number of subjects, analysed in the context, can only be due to wrong spirometry manipulation.
Figure
The subject’s data (FVC, FEV1 and FEV1/FVC) were compared to reference values and interpreted
by the specialist physician, who correlated them with the clinical examination and formulated the initial and final diagnoses (Tables
Because deaf children have communication difficulties, they are faced with the refusal of their entourage that they do no not understand; they can neither receive nor provide explanations, and the non-acceptance of their desires seems brutal, unmotivated, and gives them the impression of hostility. According to specialists, deaf people are more frustrated than people with normal hearing, and hence their slightly aggressive nature (Virole, 2005).
The influence of environmental factors and infections on lung development was investigated in many studies (Barker et al., 1991; Finkelstein & Johnston, 2004), but the impact of movement games has not been closely assessed, and therefore this hypothesis has not yet been checked.
In this study, we used spirometry to assess the lung function in deaf children and analysed two parameters, FVC and FEV1; the former reflects pulmonary capacity, and the latter, airway obstruction.
The children in both investigated groups have improved their lung function, those in the experiment group recording a rather large increase in their vital capacity (23.72% within 7 months). This may be due to better pulmonary function, but also to their appropriate participation in the spirometry test.
As regards the obstruction level, both groups show considerably improved values. A significant aspect is that the degree of airflow limitation has decreased in 72.2% of children, which demonstrates once again the importance of physical exercise for this category of special children. (Figure
But we believe that, although the differences between the two groups are due to the sports activities organised during the lesson, they partially result from the subjects’ appropriate participation in the spirometric assessment. The misunderstanding of indications has led to the erroneous labelling of some children with delays in the respiratory system function.
When deaf children perform simple sports acts (they throw/catch a ball or jump), they are pleased and proud of their performance. At the same time, when running over the 50-m distance, the indication “You need to be fast” is not understood, while “You have to win” is intellectually perceived and immediately achieved (Colin, 2012).
Thus, the teacher is in a challenging situation: in order to fulfil the objectives of the school subject, they must develop, but also temper the desire for winning expressed at a purely individual level. How can we overcome this communication difficulty? By stimulating the hearing-impaired children to practice movement and team games, during which they can benefit from special educational tools: a soundproof room equipped with audio induction loop systems, outdoor lessons at the stadium, swimming classes.
If adapted, the teaching of physical education to the deaf student and implicitly the optimisation of lung function do not involve real difficulties, although the results can be seen after a long period of time (also because much time is wasted on explanations). Deaf students are eager to know and, paradoxically, the emotional bond created between teacher and student actually translates into more communication.
Limitations of the research
In our research, we can identify three categories of limitations, which are related to: the difficulty of making conversation; the organisation of the research; the size of the investigated sample.
The experimental procedures were explained in detail to each subject through the sign language and in writing, but despite this, some children failed to understand the concept of forced exhalation; consequently, the tables also contain erroneous values, which are poorer than in reality.
Organisational difficulties only allowed double testing by spirometry, but the literature suggests that three tests are needed to make sure that the results are reproducible and accurate.
Regarding the investigated sample, the small number of participants leads us to state that the results cannot be generalised, so they have significance only for the research subjects.
Conclusion
Pulmonary tests are an important tool in assessing patients with known or suspected respiratory disease. Their interpretation requires knowing normal values and the flow-volume graph, as well as clinical history.
Our study shows how some children with hearing impairments are disadvantaged by the spirometry test, highlighting the (erroneous) possibility of a malfunctioning respiratory system. In this context, a first conclusion of the study would be the need to improve the testing instructions for deaf children. Our observations are in line with other studies that have reported increased aerobic efficacy in children with normal hearing, just due to a better understanding of these indications.
The results of our study reveal that the participating students have different levels of airway obstruction, as a consequence of their reduced thoracic elasticity, and identify a possible cause for the changed values of the spirometric parameters, namely the lack of verbal language development. Thus, they confirm that using the lungs to speak and shout (inherent actions in the movement games) has a positive effect on pulmonary development, which validates our hypothesis that the substantial use of movement games for students with hearing impairments will result in the optimisation of their respiratory function.
Our data prove that sensory deprivation (deafness) in children aged 12 to 13 years affects the functional capacity of the respiratory system. Therefore, they should be encouraged to participate systematically in sports and physical exercise programmes.
Based on their own experience, special school teachers support the idea that practicing physical exercise over a much longer period of time, uninterrupted by the summer holidays, will substantially improve the respiratory capacity of children with hearing impairments.
The only school subject where they do not feel inferior, physical education, offers the deaf children many advantages from the social point of view (because they forget about the complex caused by their impairment), but also in physical and moral terms. The direct observation of students during the lessons has revealed their increased interest in movement games, which are numerous, varied and can be combined differently and harmoniously with exercises for the learning/improvement of certain technical elements and procedures or with exercises for the development of motor qualities.
We conclude by saying that, because the current scientific-methodological literature provides little informative material, one cannot talk about a specific pedagogical method for the teaching of physical education to deaf children, but rather about a pedagogical adaptation of the learning process to these special people.
References
- Arunovic, D., & Pantelic, Z. (1997). Comparative analysis of the physical development and abilities of pupils with damaged and pupils with normal sense of hearing. Facta Univesitatis, 1(4), 29-36.
- Barker, D. J., Godfrey, K. M., Fall, C., Osmond, C., Winter, P. D., & Shaheen, S. O. (1991). Relation of birth weight and childhood respiratory infection to adult lung function and death from chronic obstructive airways disease. BMJ, 303(6804), 671-675.
- Beaussant, M. (2003). La scolarité d’un enfant sourd. Paris: Harmattan.
- Cirino, E. (2017). Spirometry: What to expect and how to interpret your results. Retrieved from https://www.healthline.com/health/spirometry
- Colin, D. (2012). Psychologie de l’enfant sourd. Paris: Masson.
- Craft, D. H. (2000). Visual impairments and deafness. In J. P. Winnick (Ed.), Adapted physical education and sport (3rd ed.) (pp. 159-180). Champaign, IL: Human Kinetics.
- Finkelstein, J. N., & Johnston, C. J. (2004). Enhanced sensitivity of the postnatal lung to the environmental insults and oxidative stress. Pediatrics, 113(4 Suppl.), 1092-1096.
- Johnson, J. D., & Theurer, W. M. (2014). A stepwise approach to the interpretation of pulmonary function tests. American Family Physician, 89(5), 359-366.
- Jonsson, Ö., & Gustafsson, D. (2005). Spirometry and lung function in children with congenital deafness. Acta Paediatrica, 94(6), 723-725.
- Stanojevic, S., Quanjer, P., Miller, M. R., & Stocks, J. (2013). The global lung function initiative: Dispelling some myths of lung function test interpretation. Breathe, 9(6), 462-474.
- Virole, B. (2005). Psychologie de la surdité (3e éd. revue et augmentée). Louvain-la-Neuve: De Boeck.
- Wang, X., Dockery, D. W., Wypij, D., Gold, D. R., Speizer, F. E., Ware, J. H., & Ferris, B. G. Jr. (1993). Pulmonary function growth velocity in children 6 to 18 years of age. American Review of Respiratory Disease, 148(6), 1502-1508.
- WHPP (Worker Health Protection Program). (2013). Understanding your breathing test results. Retrieved from http://www.worker-health.org/breathingtestresults.html
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
16 February 2019
Article Doi
eBook ISBN
978-1-80296-054-9
Publisher
Future Academy
Volume
55
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-752
Subjects
Sports, sport science, physical education
Cite this article as:
Ivan, C. (2019). Influence Of Movement Games On Respiratory Function In Students With Hearing Impairments. In V. Grigore, M. Stănescu, M. Stoicescu, & L. Popescu (Eds.), Education and Sports Science in the 21st Century, vol 55. European Proceedings of Social and Behavioural Sciences (pp. 16-25). Future Academy. https://doi.org/10.15405/epsbs.2019.02.3
