Abstract
Constraint-induced movement therapy (CIMT) stimulates neuroplasticity through exercises that are intended to use deficient functions. To make the process more efficient, these exercises must be integrated into intensive training. In the functional gait recovery process, the therapy uses Taub’s method. In accordance with this, the healthy lower limb is immobilised in proportion of 90% of total walking time and, concomitantly, the affected lower limb is intensively trained for 6 hours per day. Unlike the upper limb, for the lower limb, it is recommended to practice this method 5 days per week, for 3 consecutive weeks. This is the minimum standard to achieve visible progress. This study was conducted between 05- 24.06.2017 in Rosana Medical Clinic, on a group of 4 subjects diagnosed with ischemic stroke (3 female patients and 1 male patient, aged 65-72 years), and the therapy effectiveness was statistically interpreted starting from the initial and final assessments of the group. In this regard, we applied the timed “Up and Go” test. The research hypothesis is: the constrained use of the affected lower limb by immobilisation of the unaffected lower limb, in the patient with ischemic stroke, leads to improved dynamic balance and decreases the risk of falling, ensuring fast functional recovery. The research findings demonstrate the beneficial effect of the CIMT on dynamic balance, by its influence on the peripheral somatosensory system.
Keywords: Ischemic strokeconstraint-induced movement therapydynamic balance
Introduction
Constraint-induced movement therapy applied to the lower limb is based on cerebral neuroplasticity. Studies conducted by various authors, but especially those of Mark, Taub, and Morris (2006), claim, supported by clear evidence (such as transcranial stimulation, nuclear magnetic resonance etc.), the effectiveness of this therapy in rehabilitating walking in neurological patients after ischemic stroke. Thus, as regards the association of the reorganization process of cortical neural networks with constraint-induced movement therapy, the above-mentioned authors have demonstrated, in the laboratory, that repetitive action with the impaired limb leads to increased function in the motor area of the cerebral cortex.
The purpose of the method is to improve walking in a quicker time, so that the patient can become autonomous in terms of locomotion, in order to be able to fulfil the activities of daily life, involving medium- and long-distance travel, with a level of motor accuracy as close as possible to the one prior to its loss. To achieve this goal, the objectives subordinated to the method consist in:
the successive improvement of lower-limb motor control (the active flexion-extension range of motion in the coxofemoral, knee and ankle joints);
the improvement of the relationship between coordination and movement execution speed;
the improvement of quantitative walking parameters: the pace and length of steps, then transposed into the length of the walking perimeter.
Problem Statement
The scope of this method is extensive in that it can be applied not only in neurological pathologies that affect walking – stroke, multiple sclerosis (Mark et al., 2011), Parkinson (Lee, Lee, & Hwang, 2011), Guillain-Barré syndrome etc., but also in post-traumatic osteoarticular sequelae (ankle/knee sprain). Within the method, the therapeutic program involves restraining the degree of mobility of the healthy lower limb while thoroughly practicing through intense strain of the impaired lower limb, by performing functional therapeutic tasks relevant to everyday life. At the same time, compensatory movements are discouraged, aiming to shape motor behaviour and ensure the transfer of functional gains within the clinical setting into that of everyday life.
Research Questions
Given the importance of reducing the costs that the State has to bear with the functional recovery and reintegration into society of patients with ischemic stroke, this research is shaped by two fundamental questions, namely: Does constraint-induced movement therapy manage to bring this type of patients back to the level of a dynamic balance closest to the one prior to the ischemic episode? Does this therapy manage to accomplish this in the shortest time possible?
Purpose of the Study
If patients with ischemic stroke, with severe disturbances of dynamic balance are subjected to constraint therapy induced to the healthy lower limb, for 3 weeks, daily, for 90% of the day, their dynamic balance improves and the risk of falling decreases significantly.
Research Methods
The research was conducted between June 5 and 24, 2017, in Rosana Medical Clinic and targeted a group of 4 subjects (3 females and 1 male) aged 65 to 72 years, having the diagnosis of ischemic stroke. The subjects were evaluated both initially and at the end of therapy by the timed “Up and Go” test (Cordun, 2009). To include them in the study, we considered the following inclusion and exclusion criteria:
Inclusion criteria
clinical diagnosis of hemiparesis after ischemic stroke, whose duration until the study did not exceed six months;
no recurrence of ischemic stroke until the study;
the absence of pain of any kind in the lower limbs;
the absence of any medical problems (bedsores, arthrosis etc.), which could make it impossible to practice walking under constraint-induced conditions;
the possibility to cover a walking perimeter of at least 200 m, without the aid of a device or another person;
aged between 65 and 72 years.
Exclusion criteria
age under 65 and over 72 years;
the time elapsed from the occurrence of the stroke until the study, more than 6 months;
haemorrhagic stroke;
patients who were having pains in the lumbar spine and lower limbs;
subjects who had not given their consent;
the presence of other disorders overlapping with the neurological syndrome.
Implementation of therapeutic design
The subjects were tested for the level of dynamic balance both before and after therapy. The test used was the timed “Up and Go”. Between the two assessment moments, the subjects were applied constraint-induced movement therapy for the lower limb, which consisted in mounting a fixed knee orthosis on the healthy lower limb, so that the knee joint was blocked in maximum extension. With this orthosis, they were subjected to a program of performing motor tasks, cumulated in a set of 12, which were performed every day, for 3 weeks, from 08:00 AM to 08:30 PM. Between the sets of tasks, they were given 90-minute breaks. The 12 tasks consisted in:
walking on a horizontal plane facing the direction of travel;
walking on a horizontal plane with the back towards the direction of travel; side walking with added step;
walking by avoiding some obstacles (located at a distance of 1 meter one to the other); walking on an inclined plane over a distance of 6 m;
walking on a horizontal plane over a distance of 6 m, with an emphasis on the heel attack phase, followed by rolling of the foot on the ground, with self-imposed speed;
walking on a horizontal plane over a distance of 6 m, by stepping over obstacles located at a height of about 3 cm, with self-imposed speed;
walking on a horizontal plane by changing the direction upon verbal command, over a distance of 6 m;
walking on a horizontal plane over a distance of 6 m, by performing a task: while walking, he/she picks up stakes from the ground;
walking on a horizontal plane over a distance of 6 m, by performing a task: while walking, the patient catches with both hands a ball thrown by the physical therapist (he/she is in front of the patient at a distance of about 2 m), and then throws it to the physical therapist, with both hands, from the chest;
walking up the steps of a staircase (5 steps);
walking down the steps of a staircase (5 steps); the initiation was done with the disease-free lower limb (the one with the orthosis), because we wanted to get the best control of the unipodal support (in particular, controlled braking capacity) on the impaired limb.
The process of recording and interpreting the results, based on the timed “Up and Go” test, was performed disjointedly, in the sense that, in a first stage, the results were recorded by assigning scalar scores, and then interpreted according to these scores, and in the second stage, it was taken into account the test performance time, and the results were interpreted according to time points imposed by the test.
The results presented in the research were recorded and interpreted at group level.
Findings
In order to highlight the progress made, the results obtained from the two tests were transposed in the form of tables and diagrams. Progress was also quantified in percent, being distributed inversely proportional to the scale values – from both the point of view of the mobility deficit and the performance time of test tasks (e.g.: if the deficit decreases from score 3 to score 2, or the time drops from 30 seconds to 19 seconds, then progress increases in percent).
In terms of dynamic balance and risk of falling, at the time of the initial assessment, the following results were recorded: initial average score was 3.5, the worst rated score being 4 and the best rated score being 3 (Table
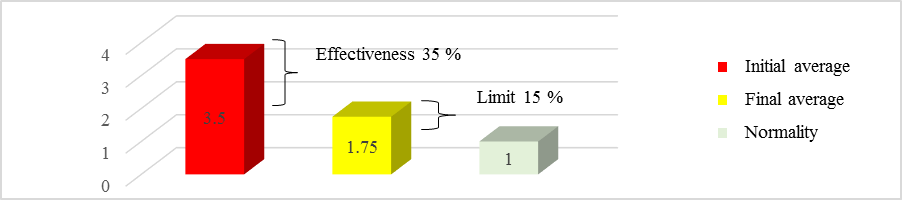
By analysing the initial and final averages of the group, there was a difference of 1.75. It follows that therapy achieved an average efficiency of 35% (Figure
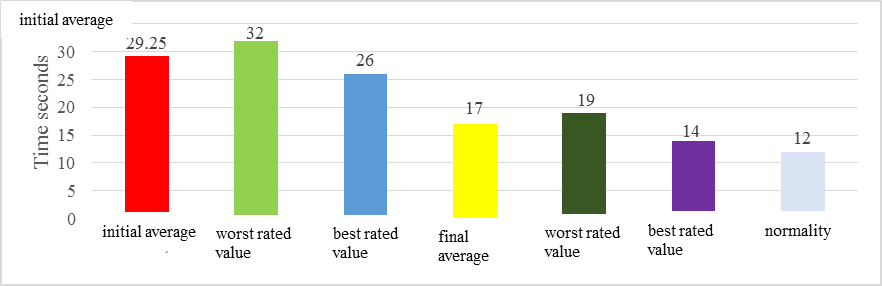
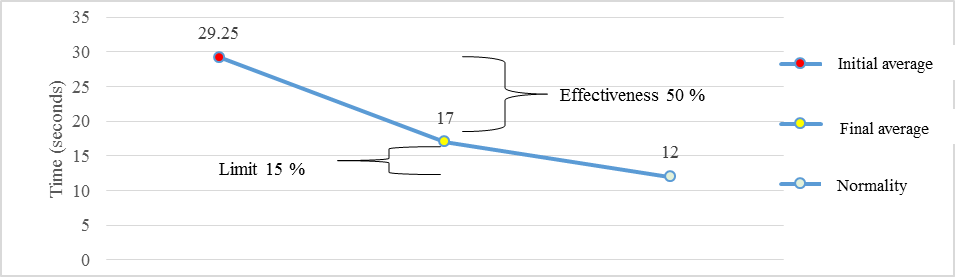
Regarding the performance time of the test, the initial average of the group was 29.25 seconds, the worst rated value being 32 seconds and the best rated value being 26 seconds (Figure
Conclusion
During the performance of motor tasks, the subjects were determined – by the positive support response, movement reflex, cross extension reflex, reflex locomotion – to predominantly use the impaired lower limb, which automatically led to intense brain information about the impaired part (Robănescu, Marcu, Mertoiu, Robănescu, & Stanciu, 2001). Through repetition, the development of the motor program was “enriched” with information from the periphery, and consequently, there was a decrease in hemispatial neglect syndrome, the brain beginning to progressively “rely” on the impaired limb, which resulted in the optimal adjustment of the support base during walking.
We consider that the mechanism by which induced constraint improves dynamic balance is in close correlation with the set of proprioceptive structures. This is represented by the multitude of receptors in the joints, muscles, tendons and ligaments, which inform the central nervous system about muscle length, contraction state and muscle tension, segment position and pressure.
References
- Cordun, M. (2009). Kinantropometrie. București: CD Press.
- Lee, K. S., Lee, W. H., & Hwang, S. (2011). Modified constraint-induced movement therapy improves fine and gross motor performance of the upper limb in Parkinson disease. American Journal of Physical Medicine and Rehabilitation, 90(5), 380-386.
- Mark, V. W., Taub, E., & Morris, D. M. (2006). Neuroplasticity and constraint-induced movement therapy. Europa Medicophysica, 42(3), 269-284.
- Mark, V. W., Uswatte, G., Bashir, K., Cutter, G. R., Bryson, C. C., Taub, E., … Bowman, H. (2011). Constraint-induced movement therapy for the lower extremities in multiple sclerosis: Case series with 4-year follow-up. Archives of Physical Medicine and Rehabilitation, 94(4), 753-760.
- Robănescu, N., Marcu, V., Mertoiu, M., Robănescu, L., & Stanciu, M. (2001). Reeducarea neuromotorie: Recuperare funcțională și readaptare. București: Editura Medicală.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
16 February 2019
Article Doi
eBook ISBN
978-1-80296-054-9
Publisher
Future Academy
Volume
55
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-752
Subjects
Sports, sport science, physical education
Cite this article as:
Mitroi, S., & Cordun, M. (2019). Improving The Dynamic Balance In Patients With Stroke By Constraint-Induced Movement Therapy. In V. Grigore, M. Stănescu, M. Stoicescu, & L. Popescu (Eds.), Education and Sports Science in the 21st Century, vol 55. European Proceedings of Social and Behavioural Sciences (pp. 209-214). Future Academy. https://doi.org/10.15405/epsbs.2019.02.26
