Abstract
One of the factors that define the level of health care is provision with professional medical staff. The aim of the present investigation is to analyze the current situation with human resources of the health care system in Karaganda region of Kazakhstan and the main trends of its dynamics in future. This investigation is based on the statistical data of WHO and Statistical composite materials “Health of the people of Kazakhstan and the activity of the health care organizations” from 2000 to 2014. During this period it has indicated the number of doctors and nurses per capita that was bigger than in the countries of the EU and CIS. The changes in the provision with physicians are related to the number of population. It is positive if the population and life expectancy increase, and negative if the level of mortality goes up. The proportion of physicians in different fields has its own peculiarities. In the structure of the health care system in Kazakhstan, there are differences from western countries. Karaganda region has a problem of unequal provision with physicians between town and village and a problem of medical staff ageing. In general, the staffing level for 2014 in the region amounted to 97% and the nationwide indicator was 93.7%.
Keywords: Human resourceshealth carelife expectancymedical staff
Introduction
One of the factors that define the level of health care is provision with professional medical staff. The aim of the present investigation is to analyse the current situation with human resources of the health care system in Karaganda region of Kazakhstan and the main trends of its dynamics in future.
Now the shortage of health workers admits as one of the leading factors interfering development of a health care system, especially in the countries with low and average income (World Health Organization WHO, 2010).
In the report of the World Health Organization "A Universal Truth: No health without a workforce", made at the third global forum on human resources of health care in November 2013, is noted that in 2035 there won't be enough 12,9 million workers of health care in the world; today shortage is estimated in 7,2 million people (WHO, 2013).
According to WHO experts, for ensuring basic level of medical care it requires 23 experts of health care on 10 thousand of the population. In 83 countries this level is still not reached.
According to the analysis which is carried out by WHO (2006) in the system of global health care work more than 43 million people, including 20,7 million nurses/midwifes, 9,8 million physicians and about 13 million other experts.
At the global level, many countries are facing critical health-care human resources (HRH) challenges including worker shortage, skill-mix imbalance, maldistribution, poor work environment, and weak knowledge base (Chen et al., 2004; Dussault & Dubois, 2003; Wyss, 2004). In several low and low-middle income countries, the supply of health professionals is being challenged by demographic trends; an aging population; growing shortages; limited education and training capacities; poor recruitment and retention strategies including out-migration of health professionals; skill-mix imbalance; maldistribution; poor HRH planning; absence of a reliable database; poorly informed policy decisions (Chen et al., 2004, Wang, Collins, Tang, & Martineau, 2002); and slow health system reform (Wang, Collins, Tang, & Martineau, 2002).
The African region and the region of Southeast Asia having the biggest population density which bears the greatest burdens of limitation of medical services and at the same time have the lowest density of health workers in comparison with richer countries of Europe and America (Table
Problem Statement
Health-care human resources planning has been identified as the most critical constraint in achieving the well-being targets set forth in the United Nations’ Millennium Development Goals (Dreesch, 2005). Moreover, the effective use and deployment of personnel is paramount to ensure an efficient service delivery in terms of cost, quality and quantity (Ozcan, Taranto, & Hornby 1995). Failure to do so may result in an oversupply or shortage of clinical staff. While the former may lead to economic inefficiencies and misallocated resources under the guise of unemployment (Roberfroid, Leonard, & Stordeur, 2009) or inflated costs through supplier-induced demand (Birch, 1993), the latter is linked to a more extensive list of negative effects, including but not limited to the following: lower quantity and quality of medical care as few resources exist to provide the necessary services and the visits are shorter (WHO, 2006); work overload of the available physicians and nurses, resulting in sleep deprivation, ultimately compromising patient safety (Williamson & Fejer, 2000); and queues and waiting lists resulting from insufficient medical staff, causing avoidable patient deaths (Steinbrook, 2014).
A key element of system transformation is an educated and skilled workforce (Health Council of Canada, 2005), with appropriate skill mix, that is utilized in an effective and efficient way (Baranek, 2012). Changing the way healthcare providers work together to deliver care may address potential HHR shortages, healthcare provider misdistribution, and help achieve high quality, efficient, and cost-effective care. Furthermore, workforce modification is expected to increase productivity, job satisfaction, recruitment, and retention (Alberta Health Services, 2012), leading to a sustainable health workforce (Australian Capital Territory, 2012) and more effective and accessible service delivery (Health Workforce Australia, 2011).
Comparison of human resources for health in different countries represents a certain difficulty associated with varying the role of doctors and nurses, which they perform in the hospital, clinic, or in the provision of emergency medical assistance (Rechel, Dubois, & McKee, 2006).
By the assessment of international experts, the main part of the zones of inefficiency is "at the junction" between different parts of the health care industry of Kazakhstan - increase the load on the narrow specialists, a high proportion of unnecessary hospitalizations, duplication of diagnostic studies in polyclinics and hospitals because of the low performance of the primary health care (The state program of development of health care of the Republic of Kazakhstan "Densaulik", 2015). Primary health (PHC) and social care has not yet become the central link in the health care system, which would provide a rational distribution of phases of treatment in outpatient and inpatient levels. The presence of a strong PHC allows developed countries to hold up to 80% of patients at its level, becoming thus the main coordinator system, whereas in Kazakhstan as the main serving structure remains stationary sector.
Research Questions
The changes in the provision with physicians are related to the number of population. It is positive if the population and life expectancy increase, and negative if the level of mortality goes up. The proportion of physicians in different fields has its own peculiarities. In the framework of this study, it is proposed to answer the following questions: whether the structure of human resources in Kazakhstan (Karaganda region) have specific features that distinguish it differs from European countries, what steps appropriate taken to adopt contemporary planning methods.
Purpose of the Study
The purpose of this study was to analyse the current situation of human resources in health care in Karaganda region of Kazakhstan and the main trends of its dynamics in the coming years.
Research Methods
We used the method of comparative analysis in the work. This investigation is based on the statistical data posted on the website of the World Health Organization and the statistical compendium "Health of the population of the Republic of Kazakhstan and the activities of health organizations for 2000 – 2014”, posted on the website of the Ministry of Labor and Social Protection of Population of the Republic of Kazakhstan. We analyzed indicators such as the number of physicians and nurses per 10 000 population, the population in the region, life expectancy, morbidity and mortality rates. To determine the correlation, the authors used the nonparametric Spearman correlation coefficient. The number of physicians per 10,000 populations in countries with developed economies over the past 15 years had a tendency to growth (Figure
![Physicians density in different countries]](https://www.europeanproceedings.com/files/data/article/81/3843/icRPTSS2018FA065.fig.001.jpg)
Findings
According to WHO information in the European Union, the growth rate of number of physicians had amounted to an average of 1.3%, in the Nordic countries - 1.9%, in the CIS countries - 1.2%. In Kazakhstan, the figure was 1.3% and in Central Kazakhstan, there was a small dynamics at an average of 0.8%. It should be noted that in the period from 2000 to 2014 in Kazakhstan the number of doctors per capita was more than in the countries of the European Union and the CIS. Thus, in 2000, in the EU and the Scandinavian countries were 29 and 30 physicians per 10,000 of the population, and in Karaganda region were almost 42 that exceed even the overall republican level of 33. And if in the European countries this figure rises to 2014 up to 35 and 38, respectively, in Kazakhstan as a whole - up to 39.2, and in Karaganda region - reached the value of 46.2.
The correlation analysis showed that changes in the availability of physicians have a significant positive relationship with population growth in the area (r=0.77, p<0.05), the increase in life expectancy (r=0.65, p<0.05) and a negative relationship with mortality (r=-0.71, p<0.05). However, an increase in the number of physicians very weak correlated with morbidity (r=-0.27, p<0.05), which in those years was the downward trend.
Indicators of availability of middle medical staff per capita in Karaganda region are higher than in the EU and CIS, but much less than in the Scandinavian countries (Table
An important indicator of the health care system is the ratio of physicians and paramedical staff. On average in the EU countries it is 1:2.5, while in Germany and France on the one physician has 3 nurses, USA - 3.2, Great Britain - 3.5, Canada, Switzerland and Finland - 4, and in Belgium - 5. In Karaganda region in recent years, this ratio is 1:2.1, and in 1991 in the Republic there was one physician per 3 secondary medical workers.
In previous years the most significant growth occurred in the availability of physicians-cardiologists, the average annual growth rate of 3.8% (Figure
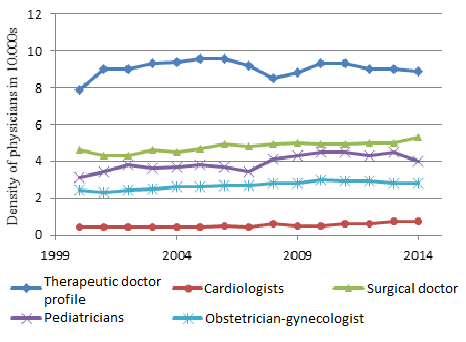
In various states, the ratios between physicians of different specialties have their own peculiarities. In the structure of the health care system in Kazakhstan, there are differences from western countries.
Thus, as of 2014, more specialists in the therapeutic and surgical profile were in the European Union, while in the EU and in the Nordic countries there were fewer obstetricians of gynecologists and pediatricians (Table
The provision of medical personnel in the city and in the countryside is uneven. In 2014, in the urban area of Karaganda region, there were 53.7 physicians per 10,000 populations, while in rural areas - 17.7. A similar picture is in the provision of average medical personnel: 99.3 and 71.9, respectively.
The problem of the "aging" of medical personnel remains one of the most important problems. In 2013, the proportion of persons of pre-retirement age in the Republic was 30.7%, and in the region 36.7%.In general, in 2014, the staffing in the field amounted to 97%, while the Republican average is 93.7%.
Conclusion
According to the estimates of the American Association of Medical Colleges, the problem of the shortage of physicians in the most developed countries will become extremely acute in the very near future. So in the US, despite the growth in the number of physicians, by 2025 the growth in the need for medical care will lead to a deficit of more than 20% (160,000) of physicians (Dill & Salsberg, 2008). These calculations are based on the assumption that the current trends in the number of graduates of medical schools are maintained, taking into account the aging of the population and the increase in the prevalence of chronic diseases, changes in the gender and age composition of medical personnel, and the increasing availability of medical care for people with low and middle incomes (Cooper, Getzen, McKee, & Laud, 2002).
In the public health development program of the Republic of Kazakhstan "Densaulyk" for 2016-2020б it was noted that "in Kazakhstan there is an imbalance in the staffing between levels of medical care (deficit at the PHC level and village, surplus - at the hospital level). On average, one PHC physician serves about 2,200 attached populations, whereas in OECD countries the burden is significantly lower - less than 1,500. There is a shortage of middle medical workers at the primary health care level (1.1 nurses per 1 local physician with the optimal ratio of 2-3). There are problems associated with uneven geographical and territorial distribution, as well as structural staff imbalances. In this regard, "further improvement of the normative regulation of personnel security, planning and forecasting is necessary" (The state program of development of health care of the Republic of Kazakhstan "Densaulik", 2015).
Human resources planning is a complex process, including political, economic, technical aspects, the level of qualifications of personnel, priorities of the health care system, etc. Currently, the following methods of forecasting are recommended in the Republic: a population-based method, a method based on targeted indicators of care, a method based on the needs for medical care and services. There are other methods, including those developed by WHO. No country has a definite forecasting model, which could be called the best. There is an understanding that an integrated approach is required to plan medical personnel resources and its main goal is to improve access and improve the effectiveness of medical care.
References
- Alberta Health Services. (2012). Clinical workforce strategic plan 2011-2016. Ver 4.6. Retrieved from http://insite.albertahealthservices.ca/hpsp/tms-hpsp-cwsp-appendices.pdf
- Australian Capital Territory. (2012). Health workforce plan for 2013-2018. Retrieved from http://www.health.act.gov.au/c/health? a = sendfile & ft = p & fid = 1907982279 & sid =.
- Baranek, P. (2012). Review of the areas of practice of medical professions in Canada: Balancing act. Retrieved from http://www.healthcouncilcanada.ca/rpt_det.php?id=133.
- Birch, S. (1993). A re-examination of the meaning and importance of supplier-induced demand. J Health Econ, 2, 1–22.
- Chen, L., Evans, T., Anand, S., Buffoff, D.I., Brown, X., Chowdhury, M., . . . Eltsinga, G. (2004). Human resources for health: overcoming the crisis. Lancet, 364, 1984-1990.
- Cooper, R. A., Getzen, T. E., McKee, H. J., & Laud, P. (2002). Economic and demographic trends are signaling the imminent shortage of a doctor. Health issues, 21 (1), 140-154.
- Dill, M.J. & Salsberg, E.S. (2008). The Complexities of Physician Supply and Demand: Projections through 2025. Washington, DC: Association of American Medical Colleges
- Drishev, N., (2005). Approach to assessing the human resource needs for achieving the Millennium Development Goals. Health policy and planning, 20 (5), 267-76.
- Dussault, G, & Dubois, C.A. (2003). Human resources for health policy: an essential component of health policy. Hum Resour Health, 1, 1-15.
- Health Council of Canada. (2005). An Environmental Scan of Current Views on Health Human Resources in Canada: Identified Problems, Proposed Solutions and Gap Analysis. Retrieved from https://healthcouncilcanada.ca/files/2.13-EnvironScanENG.pdf
- Health Workforce Australia. (2011). National health workforce innovation and reform strategic framework for action – background paper. Retrieved from http://www.hwa.gov. au/sites/uploads/wir-strategic-framework-background-paper-FinalFinal.pdf.
- Ozcan, S., Taranto, Y. & Hornby, P. (1995). Forming future health in Turkey: a new role in human resources planning. International Journal of Planning and Health Management, 10 (4), 305-19.
- Rechel, B., Dubois, C.-A. & McKee, M. (2006). Health personnel in Europe. Learning from personal experience. WHO Regional Office for Europe (Copenhagen).
- Roberfroid, D., Leonard, C. & Stordeur, S. (2009). Prognosis of the doctor's proposal: better than a glimpse into the crystal ball? Human resources for health. 2009; 7 (1), 1-13.
- Steinbrook, R. (2014). Private Health Care in Canada. N Engl J Med, 354 (16), 1661-4
- The State Health Development Program of the Republic of Kazakhstan "Densaulik" for 2016-2019: Resolution of the President of the Republic of Kazakhstan of January 15, 2016 No. 176 Retrieved from http://www.npzdravrk.kz/index. PHP / Health-with / 112-2
- Wang, Y., Collins, C., Tang, S., & Martineau, T. (2002). Health systems decentralization and human resources management in low and middle income countries. Public Administration and Development, 22(5), 439-453
- WHO (2006). World health report 2006: working together for health. Geneva: WHO press.
- WHO (2010). Models and tools for planning and forecasting human resources for health. Human Resources for Health Observer. Retrieved from http://www.who.int/hrh/resources/observer3/en/
- WHO (2013) Universal Truth: No Health without a Workforce. Third Global Forum on Human Resources for Health Report, WHO press.
- Williamson, A.M., Fejer, A.M. (2000). Moderate sleep deprivation leads to a deterioration in cognitive and motor performance, equivalent to the legal levels of alcohol intoxication. Busy Environ Med, 57 (10), 649-55.
- Wyss, K. (2004). Approach to the classification of human resource constraints to achieve the health-related Millennium Development Goals. Hum Resour Health, 2, 1-8.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
17 December 2018
Article Doi
eBook ISBN
978-1-80296-049-5
Publisher
Future Academy
Volume
50
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-1464
Subjects
Social sciences, modern society,innovation, social science and technology, organizational behaviour, organizational theory
Cite this article as:
Kharin, A., Koichubekov, B., & Omarkulov, B. (2018). Condition Of Human Resources Of Health Care System In Karaganda Region. In I. B. Ardashkin, B. Vladimir Iosifovich, & N. V. Martyushev (Eds.), Research Paradigms Transformation in Social Sciences, vol 50. European Proceedings of Social and Behavioural Sciences (pp. 544-551). Future Academy. https://doi.org/10.15405/epsbs.2018.12.65

