Towards The Problem Of Depersonalization Disorders Psychotherapy (A Pilot Study Findings Discussion)
Abstract
The study addresses the problem of search for psychosocial factors associated with depersonalization-derealization disorders (DDD). Research design consists of two stages: 1. A nonclinical sample study using four questionnaires (N=101). 2. Between-group comparison of patients diagnosed with depression and DDD (N=15) and patients diagnosed with depression without DDD (N=15). For the second stage a battery of 8 questionnaires and the Rorschach test has been used. On a high level of significance general intensity of DDD phenomena experience (according to Cambridge Depersonalization Scale) positively correlates with reflection and cognitive flexibility (Beck Cognitive Insight Scale); usage of certain coping mechanisms: mental disengagement, denial, focus on and venting of emotions, behavioral disengagement, substance use, acceptance (COPE); alienation from other people, from the family, from oneself, vegetativeness, helplessness and nihilism (Alienation Questionnaire). DDD intensity negatively correlates with self-certainty, active coping and planning (COPE). Patients with DDD have lower self-reflection (The Self-Reflection and Insight Scale), lower planning index (Self-Regulation Profile Questionnaire), prefer using composing drugs and planning as the means of coping (COPE), score higher on impulsiveness in the attention sphere (The Barratt Impulsiveness Scale, Version 11), they are less likely to have meaninglessness in personal relationships (AQ). The Rorschach test revealed that patients with DDD score significantly lower on Perceptual-Thinking Index, associated with reality testing. Study limitations are evaluated. Several psychological explanations are discussed and possible psychotherapeutic strategies for treating DDD are suggested.
Keywords: Depersonalizationderealizationreflectionalienationrorschqch testpsychotherapy
Introduction
Depersonalization-derealization disorders (DDD) appear in literature from the second half of XIX century (Sierra & Berrios, 1997). Summing up the descriptions, five principal dimensions of the disorder symptoms and complaints can be defined (Sierra, 2009, Simeon, 2006; Michal et al., 2016):
complaints about feeling changes in bodily experiences;
feeling of action automation (lack of feeling in control of self);
emotional numbing;
changes in subjective experiences, imagination, autobiographical recalling;
complaints about feeling alienated from the outside world (derealization).
Along with these come commonly known phenomena of déjà vu (seen for the first time is experienced as familiar) and jamais vu (familiar is experienced as seen for the first time). It is also typical for the patients with DDD while complaining about not feeling anything, at the same time to feel high levels of anxiety.
Epidemiologically, these disorders usually appear among youth; equal between men and women; more common for the West than the East; usually appear in a chronic form with no remission not as a specific syndrome, but among other psychiatric disorders, especially affective disorders. The commonly found triggers are stress, episodes of other psychopathological disorders and drug abuse. (Hunter, Sierra, & David, 2004).
It has been proven only recently through a sizeable statistical data gathering, that it not only appears to be an independent disorder but that it is as common, as some other major disorders – carried by 0.8-2% of the population (Sierra, 2009). DDD phenomena seem to be universal outside of clinic, appearing in 26-74% of the non-patient population during lifetime (Hunter et al, 2004). It might appear when a person is experiencing worry, burnout, fatigue, sleep deprivation (Simeon, 2006). When it appears within some other forms of mental disorders (i.e. schizophrenia, depression, anxiety disorder), it seems to be a valuable diagnostic and therapeutic marker, signaling that the major disorder appears in its heaviest form and that it will be resistant to pharmacological treatment (Mula, Pini, & Cassano, 2007).
Despite the fact that in the historical context DDD drew much interest due to potential insight in psychological and philosophical questions about the nature of consciousness, subjectivity and self-experience (works of K. Jaspers, L. Dugas, F. Moutier and many others), during the last decades there is a significant overweight of searching for neurobiological basis and pharmacological treatment for DDD. This path has not yet led to any established treatment plan, and the disorder still stays resistant to pharmacotherapy. To find ways and strategies for treating it with psychotherapy, we need to take further steps in finding out more about the role of psychological factors and possible psychological mechanisms.
Problem Statement
Due to a fundamental lack of psychological studies of DDD, current research aims at taking few steps toward testing the waters in this field and at finding possible psychotherapeutic strategies for treating these disorders. It is now widely considered to have a biopsychosocial approach in psychiatry (Engel, 1980), although, such a model is absent for treating DDD.
Also, there are some notions of DDD phenomena occurring differently in non-patient population and in patients differs not only quantitatively, but also qualitatively (Hunter et al., 2009), the difference has been annotated based more on observable data. It is essential to compare the results of two conditions with same experiences looking into similar psychological parameters. This could help to find out whether the mechanism for the disorder is a chronification: phenomena occurs in personal experience and so some stay with it, some experience it briefly - why? Are there any predispositional and buffering psychosocial factors associated with DDD?
Literature review reveals that there is an exceptional role of reflective processes as markers of DDD (Sierra, 2009). Probably something associated with them might serve as predispositional or chronificational factors (Torch, 1987; Sacco, 2010).
From the other side, in general psychology reflection as a psychological process is often seen as being a form of “normal” alienation (Leontiev, & Salikhova, 2010). However, what particular kind of reflection do these who experience DDD phenomena perform?
These are some of many questions that are still being unanswered in this field of research, which we are only starting to plow.
Research Questions
Following research tasks were suggested:
Using several batteries to find out how reflection, coping and meaning alienation associated with the occurrence of DDD phenomena in a nonclinical population.
Using expanded battery of methods to find out particularities in self-regulation, reflection, coping and meaning alienation in patients with DDD.
To find any significant markers for personal, interpersonal, perceptional particularities in patients with DDD by using the Rorschach test.
Purpose of the Study
The study aims at the multidimensional research of DDD phenomena and psychological factors associated with it, mainly reflection and perception.
Research Methods
Research design
To conduct the pilot study according to the research questions, we proposed following research design:
Research of the appearance of DDD phenomena in a nonclinical sample and its correlation with several other questionnaires (CDS, BCIS, COPE, AQ – see the list below).
Between-group comparison of patients with depression and with or without DDD using an expanded battery of questionnaires and the Rorschach test.
Methods used
List of methods used:
Cambridge Depersonalization Scale (CDS) (Sierra, & Berrios, 2000)
Beck Cognitive Insight Scale (BCIS) (Beck, 2004)
The Self-Reflection and Insight Scale (SRIS) (Grant et al., 2002)
Self-Regulation Profile Questionnaire (SRQM) (Morosanova, 2017)
The Barratt Impulsiveness Scale, Version 11 (BIS-11) (Patton et al., 1995)
Behavior Rating Inventory of Executive Functions – Adult Version (BRIEF-A) (Roth et al., 2005)
Cognitive Emotion Regulation Questionnaire (CERQ) (Garnefski, & Kraaij, 2007)
COPE (Carver et al., 1989)
Alienation Questionnaire (AQ) (Osin, 2009)
(all questionnaires have and approved Russian version)
The Rorschach test (Exner, 2003; Mihura, Meyer, Dumitrascu, & Bombel, 2013).
We chose the Rorschach test as our core method for several reasons. First, it is different from other methods; it can be sensible to a large number of personal traits, can reveal particularities of perception, personality characteristics, relationship patterns, cognitive and emotional functioning and other spheres. Second, it has recently been thoroughly analysed according to contemporary scientific standards (Mihura, 2013) and also can be representative in clinical conditions. Third, although the test is commonly used as a reliable diagnostical tool, we have not found any scales that might help to reveal DDD.
The Data was analysed using Microsoft Excel 2007 and StatSoft STATISTICA 8.0 for Windows 7 (Mann-Whitney U-test, Spearman’s rank correlation coefficient).
Characteristics of the Sample.
The study has been conducted in Russian with Russian sample. The nonclinical sample has been gathered using internet forms and filtering data from participants who took less than 15 minutes for filling all four questionnaires.
The clinical group with DDD alone (as it is described by Sierra (2009)) has been hard to find. To gain some insight into DDD phenomenology alone, we decided to compare a group of patients with depression and comorbid DDD, and a group of patients with depression without any DDD in anamnesis. Patients were diagnosed by psychiatric expertise in Mental Health Research Center.
Findings
Study 1. Non-patient sample DDD phenomena correlations.
Nonpatient sample revealed following correlations of DDD phenomena general intensity (CDS) with several psychological parameters:
Positive correlation with reflection and cognitive flexibility (BCIS – p<0,001), and negative correlation with self-certainty (p<0,02).
Correlation with coping strategies questionnaire (COPE) was positive with usage of following coping strategies (p<0,01): mental disengagement, denial, focus on and venting of emotions, behavioral disengagement, substance use, acceptance. Negative correlation with active coping (p<0,0002) and planning (p<0,03).
As on the level of meaning and values (AQ), higher DDD intensity index correlates with higher levels of alienation from other people (p<0,01), alienation from the family (p<0,02), alienation from oneself (p<0,0001), vegetativeness (p<0,004), helplessness (p<0,005), nihilism (p<0,02). Here we find it important to note that these are purely psychological not clinical scales of alienation and meaninglessness (Osin, 2009).
Study 2. Patient between-group comparison.
Between-group comparison of patients with depression and with/without DDD revealed following significant results (p<0.05):
Patients with depression and DDD are more likely to have lower self-reflection (SRIS), they tend to have lower planning index (SRQM); as the means of coping they are more likely to use composing drugs and planning (COPE), also they score significantly higher on impulsiveness in the attention sphere (BIS). Patients with depression and DDD are less likely to have meaninglessness in personal relationship (AQ). We need to note that we didn’t get any significant results using CERQ.
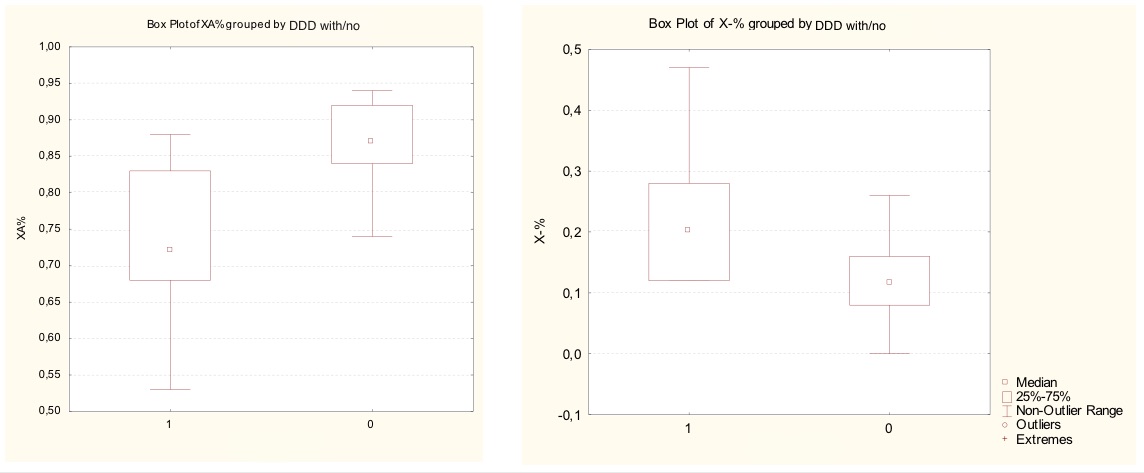
Between-group comparison of the Rorschach test results revealed only a difference in 6 out 65 variables: increase in Distorted Form (X-%), and less likely to give answers with Unusual Form (Xu%); all in all they score lower on Form Appropriate Extended (XA%), Form Appropriated Common Areas (WDA%), Conventional Form Use (Xu%) (see Table
Interestingly, in Exner’s Comprehensive System (2003) all 3 are a part of 1 out of 8 spheres in Exner’s Comprehensive System interpretation, which is Cognitive Mediation. Also, they all together form a Perceptual-Thinking Index, which determines perceptual and thinking disturbances common for psychosis associated with mood, schizotypical, borderline personality disorders (Mihura et al., 2013). Behind these variables are the measures of how inaccurate perception is depending on the form qualities of the blots; lack of giving popular and ordinary answers; numerous no-form responses.
Study limitations.
This study is defined as pilot due to obvious reasons (i.e. small samples sizes, simple statistics used). Besides this we need to note that the results of the clinical groups have following limitations: not all questionnaires were approbated in clinical settings; some patients were diagnosed with schizophrenia (7 patients in each group), which can in part explain the Rorschach test results; some patients experienced drugs side effects and needed additional support (i.e. reading aloud) to fill the questionnaires. Also it is notable that similar to several questionnaires psychological parameters (like planning and reflection) appeared to show significant results in one method but not the other despite their similarity.
Conclusion
Discussion of findings
To sum up, it has been found that in the nonclinical conditions occurrence of DDD phenomena are associated with reflection level and cognitive flexibility, more likely to use ineffective coping mechanisms (i.e. denial, substance use, mental disengagement and other) and not using effective ones (like planning, active coping), and meaninglessness in a range of personal life spheres (others, family, self).
Clinical sample, on the other hand, has shown that patients with DDD show lower results of self-reflection and lower results in planning abilities, but prefer to use composing drugs and planning as the means of coping. Unlike patients with depression without DDD, they tend to have less meaninglessness in personal relationships. The Rorschach test revealed that patients with DDD score significantly lower on Perceptual-Thinking Index, which is associated with psychosis and refer to lower levels of reality testing.
The results gathered leave an ample space for psychological interpretation and assumptions, while keeping in mind their limitations. We would like to focus on several findings relevant to the initial research tasks.
First of all, we are now able to see a part of the inner structure of differences in DDD phenomena occurring in nonclinical population and patients, and it is of not only quantitative but qualitative as it has been suggested based on observational data before (Hunter et al., 2004): in nonclinical sample DDD phenomena appears to be associated with higher level of reflection, lower on planning, while in clinical sample we see a quite opposite picture. We can assume that the difference is in the part reflection plays in coping and self-regulation processes. Particularly, in the nonclinical sample, we find a high correlation with several effective coping mechanisms (with a notable exception of active coping and planning), which might support the idea of some form of alienation being normal in the process of coping with critical situations and anxiety (Nuller, 1982). Reflection in general psychology is commonly seen as a major ability for self-regulation and planning. DDD might be the case of appealing to reflection by itself, using it as a separate activity (objectifying self-observation), that is not playing function in self-regulation and planning processes, which in some cases leads to frequent and prolonged DDD phenomena developing a sort of vicious circle. This conclusion supports theoretical models of psychotherapeutic treatment for DDD by Sacco (2010) and Torch (1987). Also, it is consistent with a hypothesis by a well-known founder of Russian abnormal psychology Bluma Zeigarnik (Zeigarnik, 2012). She suggests that in DDD occurs as a shift in motivational hierarchy (basing on theoretical viewpoints of L. Vygotsky and A.A. Leontiev). She suggests that depersonalization becomes abnormal when on the place of the leading motive comes self-observation along with a lack of other motives realisation activity.
It is hard to speculate on causality relationship between reflection and DDD based on our data. We can assume both: nonpatients with higher reflection capability are more likely to spot DDD phenomena; or reflection as a psychological process being a form of “normal” alienation somehow becomes fixed leading to clinical forms of DDD (which supports the idea of its close nature with OCD (Sierra, 2009)). The last assumption opens up an interesting direction for thought and research both in finding out about the nature and treatment of DDD and the nature and role of reflection processes.
Our core finding in Rorschach test results was that the primary disturbance in patients with DDD appears in Perceptual-Thinking Index, which is associated with schizophrenia spectrum disorders. Might it suggest that DDD is a halfway state between normal functioning and schizophrenic delusions, where the feeling of alienation develops into even worse reality testing? This and other findings need to receive verification and further research.
Suggestions on psychotherapeutic interventions for DDD
Based on our findings, the first target for psychotherapeutic addressing of nonclinical DDD phenomena is to avoid discussing vague experiences in separated from life context alienating reflection, but on to preferably establish the following goals: developing planning and active coping skills and realistic future-perspective, bridging reflective processes to their original effective role in playing a part in activity regulation. For example, experiential approaches (focus on direct experiencing) and approaches of the third-wave CBT (development of self-regulation, reality testing with mindfulness techniques) might appear as more effective than nondirectional approaches.
Based on the Rorschach test results, it seems that tactics of avoiding more in-depth research of DDD and other «vague» feelings and states are advisable in therapy with clinical forms of DDD (since a tendency to discuss them might come from a psychosis-like or obsessive-compulsive urge for perceiving not standard, but unusual, not formed aspects of reality). Instead, a psychotherapeutic vector needs to be switched from intrapersonal reality to interpersonal (i.e. appreciation for everyday things, commonsense understanding and interpretation of reality, relationships). Following this logic, despite these patients are not being in schizophrenia spectrum, CBT protocols for schizophrenia might appear more effective when addressing clients with complaints on DDD phenomena.
Acknowledgments
We would like to thank for making arrangements necessary for conducting the research, supervision and invaluable critical insights professor of Lomonosov Moscow State University, doctor of psychology, Alexander Tkhostov. Also, Elena Rasskazova, Associate Professor in Lomonosov Moscow State University and Evgeniy Osin, Associate Professor in National Research University Higher School of Economics, for providing important theoretical and methodological remarks. And finally, psychiatrists in the Mental Health Research Center, especially Sergey Sorokin, Katerina Gedevani, Olga Schelokova..
References
- Beck, A. T., Baruch, E., Balter, J. M., Steer, R. A., & Warman, D. M. (2004). A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophrenia research, 68(2), 319-329. doi: 10.1016/S0920-9964(03)00189-0
- Engel G. L. (1980). The clinical application of the biopsychosocial model. American Journal of Psychiatry. 137(5), 535–544. doi: 10.1176/ajp.137.5.535
- Exner, J. E., Jr. (2003). The Rorschach: A comprehensive system: Vol 1. Basic foundations and principles of interpretation (4th ed.). New York: Wiley.
- Garnefski, N., & Kraaij, V. (2007). The cognitive emotion regulation questionnaire. European Journal of Psychological Assessment, 23(3), 141-149. doi: 10.1027/1015-5759.23.3.141
- Grant, A. M., Franklin, J., & Langford, P. (2002). The self-reflection and insight scale: A new measure of private self-consciousness. Social Behavior and Personality: an international journal, 30(8), 821-835. doi: 10.2224/sbp.2002.30.8.821
- Hunter ECM, Sierra M, David AS (2004) The epidemiology of depersonalization and derealisation: a systematic review. Social Psychiatry & Psychiatric Epidemiology, 39(1), 9-18. doi: 10.1007/s00127-004-0701-4
- Leontiev, D., & Salikhova, A. (2010). Looking at oneself as inner dialogue. International Journal for Dialogical Science, 4(2), 95-104.
- Michal, M., Adler, J., Wiltink, J., Reiner, I., Tschan, R., Wölfling, K., ... & Zwerenz, R. (2016). A case series of 223 patients with depersonalization-derealization syndrome. BMC psychiatry, 16(1), 203. doi: 10.1186/s12888-016-0908-4
- Mihura, J. L., Meyer, G. J., Dumitrascu, N., & Bombel, G. (2013). The validity of individual Rorschach variables: Systematic reviews and meta-analyses of the comprehensive system. Psychological bulletin, 139(3), 548. doi: 10.1037/a0029406
- Mula, M., Pini, S., & Cassano, G. B. (2007). The neurobiology and clinical significance of depersonalization in mood and anxiety disorders: a critical reappraisal. Journal of Affective Disorders, 99(1), 91-99. doi: 10.1016/j.jad.2006.08.025
- Morosanova, V. I., & Fomina, T. G. (2017). Self-regulation as a Mediator in the Relationship Between Anxiety and Academic Examination Performance. Procedia-Social and Behavioral Sciences, 237, 1066-1070.
- Nuller, Y. L. (1982). Depersonalisation‐symptoms, meaning, therapy. Acta Psychiatrica Scandinavica, 66(6), 451-458. doi: 10.1111/j.1600-0447.1982.tb04502.x
- Osin, E. (2009). Subjective experience of alienation: Measurement and correlates. Gesellschaft fur Logotherapie und Existenzanalyse, 1(26), 16-23.
- Patton, J. H., Stanford, M. S., & Barratt, E. S. (1995). Factor structure of the Barratt impulsiveness scale. Journal of clinical psychology, 51(6), 768-774. doi: 10.1002/1097-4679(199511)51:6<768::AID-JCLP2270510607>3.0.CO;2-1
- Roth, R. M., & Gioia, G. A. (2005). Behavior rating inventory of executive function--adult version. Lutz, FL: Psychological Assessment Resources.
- Sacco, R. (2010). The circumplex structure of depersonalization/derealization. International Journal of Psychological Studies, 2(2), 26. doi: 10.5539/ijps.v2n2p26
- Sierra, M., & Berrios, G. E. (1997). Depersonalization: a conceptual history. History of psychiatry, 8(30), 213-229. doi: 10.1177/0957154X9700803002
- Sierra, M., & Berrios, G. E. (2000). The Cambridge Depersonalisation Scale: a new instrument for the measurement of depersonalisation. Psychiatry research, 93(2), 153-164. doi: 10.1016/S0165-1781(00)00100-1
- Sierra, M. (2009). Depersonalization: A new look at a neglected syndrome. Cambridge University Press. doi: 10.1017/CBO9780511730023
- Simeon, D., & Abugel, J. (2006) Feeling Unreal: Depersonalization Disorder and the Loss of the Self. Oxford University Press.
- Torch, E. M. (1987). The psychotherapeutic treatment of depersonalization disorder. Hillside Journal of Clinical Psychiatry.
- Zeigarnik, B. (2012). Experimental abnormal psychology. Springer Science & Business Media.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
23 November 2018
Article Doi
eBook ISBN
978-1-80296-048-8
Publisher
Future Academy
Volume
49
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-840
Subjects
Educational psychology, child psychology, developmental psychology, cognitive psychology
Cite this article as:
Shankov, F., & Pluzhnikov, I. (2018). Towards The Problem Of Depersonalization Disorders Psychotherapy (A Pilot Study Findings Discussion). In S. Malykh, & E. Nikulchev (Eds.), Psychology and Education - ICPE 2018, vol 49. European Proceedings of Social and Behavioural Sciences (pp. 606-614). Future Academy. https://doi.org/10.15405/epsbs.2018.11.02.69

