Abstract
This topic was approached based on the conviction that action can be taken to improve the quality of life in children with cerebral motor deficit by both their families and by specialized healthcare staff. Considering the benefits which would be achieved, implementation of combination therapy in these children is desirable. It should become a day-to-day ritual for children with Cerebral Motor Deficit, as it is the only way helping us to achieve the goal proposed, which is to improve the quality of life of both the impaired child and their family. This research is intended to promote adoption of this combination therapy, via awareness of long-term benefits over the children’s quality of life, both for families with children with cerebral motor deficit, and among specialized healthcare staff. By definition, the quality of life is subjective, albeit for the most part, specialty literature, when it comes to the quality of life in children with cerebral motor deficit, used data from the parents rather than from the children themselves. Studies tend to focus on functional skills and their role in the quality of life and only little attention was paid to other important contextual factors, such as the environment and ambiance in families, their status, which are deemed as significant factors in the quality of life. The use of combination therapy for children with cerebral motor deficit favours the improvement of the quality of life from all points of view, not just in terms of physical evolution, but also cognitive, social etc.
Keywords: Cerebral palsy, combination therapy, quality of life, rehabilitation
Introduction
Quality of life refers to individual perception on own experience, perception developed depending on social context, cultural norms imposed and, at the same time, conditional upon personal goals, standards and needs. Where there is an early lesion on the encephalon, children will suffer permanent, irreversible and non-progressive damages, a pathology called Cerebral Motor Deficit. Subsequent symptoms materialize into movement and postural disorders, most often affecting cognitive functions as well. Disease status and its consequences affect children’ lives and their quality of life, implicitly. In order to improve the quality of life in children with Cerebral Motor Deficit and of their families too, a multidisciplinary approach must be taken as early on as possible with a joint mission, purposes and goals. This can be done by implementing certain types of combination therapy in the child’s daily routine, referring here to kinesiotherapy and occupational therapy, psychotherapy, speech therapy, medication therapy, orthopaedic- surgical treatment and various alternate therapies. Given that we have noticed, over time, how important early and correct application of this combination therapy is, we wanted to be able to emphasize the close connection between its implementation and the quality of life in children with Cerebral Motor Deficit in this article.
Problem Statement
Over time, the specialized literature, be it national or international, used a number of terms when referring to cerebral impairments. For the avoidance of any confusion as to the use of such terms, we believe it is necessary to have a brief terminological introduction from a historical point of view. The first specifications about this type of affliction were made by Mr. William John Little in 1860. He described spastic diplegia, also known for a long period of time as “Little disease”. As years passed by, the term of “cerebral palsy” is noticed in the Anglo-Saxon literature, translated as “paralizie cerebrală” in Romanian, term we use to this day. However, there is a counterargument brought by Bobath (1966), who asserted that “there is no actual cerebral palsy in this kind of conditions, a lack of a neuromuscular activity’s functioning, but rather the expression of abnormal ways of posture and movement” (p. 55). In 1953, the term of Infirmité Motrice Cérébrale was introduced by Guy Tardieu, romanian authors used various denominations over time as well for this condition, depending on the particularities noticed. Thus, Vereanu (1963) believed this pathology to be:
A persistent impairment, without being fixed, of movement and posture, arisen since birth or during the first years of life, connected to a non-tumour and non-degenerative damage of the brain, occurring during its normal development, before, during or after birth. (p. 34)
Robănescu (1983), uses the term of sequelae of chronic infantile encephalopathies, referring to “lesional damages of a child’s brain with repercussions on brain functions, especially motricity and mental development” (p. 76). Some authors believe Cerebral Motor Deficit to be a “disorder largely caused by sequalae of chronic infantile encephalopathies whose common trait is motricity impairments, mandatorily mental alterations and sometimes, epileptic fits” (Le Metayer, 1999, p. 55).
Nowadays, motor deficit is streamlined into three key groups, corresponding to physiopathological disorders:
a) spasticity- pyramid syndrome featuring an exaggeration of the stretch (myotatic) reflex in the muscle; b) dyskinesia – extrapyramidal syndrome manifested in various forms: athetosis, tremor, dystonia, rigidity etc.; c) ataxia- cerebellar syndrome produced by damage to the cerebellum or its connections and characterized by disorders of coordination and posture (Albu et al., 2007, p. 96).
There are authors who define cerebral palsy as a:
Chronic postural and movement-related disorder caused by injury to the central nervous system; it combines a group of chronic neurological disorders, non-progressive, influenced by the growth and development process characterized by inadequate control of motility and posture, due to lesions of the central nervous system, which occur during prenatal period, during birth or in the perinatal period (Alexander & Matthews, 2010, p. 77).
This brief history having been presented, we can see there are multiple differences in terms of concept and approach with obvious implications on evolution and prognosis, be it long or short-term. The attempt to reach general consensus on how to define and approach this condition was done repeatedly. The thing that can lead to a common vision with regard to the manner of approach should start with finding and using common terminologies, general clinical evaluations valid worldwide. Irrespective of the term used, the fact is confirmed that the disease arises at birth or during the first 2-3 years of life. It is a non-tumour and non-degenerative damage of the immature brain, which can occur during the intrauterine period, during birth or post-partum. Whether or not lesions can be reversible has not been proven, but various adaptive processes can take place, over time, through different treatment methods Yamada (1994, p. 66). Believes that the percentage of encephalon damage’s aetiology in children would be as follows: prenatal causes: 20,5% perinatal causes: 22,7% post-partum: 4,5% and unknown causes: 34,1%. Also, Hagberg and Hagberg ,state that the most significant importance in Infantile Cerebral Palsy-ICP/ Cerebral Motor Deficit CMD- aetiology are causes acting on intrauterine development (44% of cases), and key factors coming into play during labour and expulsion amount to 19%. Cerebral palsy’s aetiology is often not fully understood. In most cases, children with cerebral motor deficit do not have an identifiable aetiology (Hagberg & Hagberg, 1984, pp. 433-440). Among the factors which can contribute to brain damage and the development of cerebral palsy are included: prematurity, infections, inflammations and coagulopathy. A significant interest also consists in the role/ contribution of the numerous biomolecules and cytokines accompanying the infectious or inflammatory processes (Menkes, 1995, p. 177).
Quality of life is a highly controversial concept, multidisciplinary and multidimensional. According to the WHO, quality of life is: “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” (World Health Organization, 1998, p. 46). Quality of life is an amorphous concept. While the term “quality” implies the degree of a characteristic that implies excellence, different individuals may value different areas of life distinctly and, as a result, quality of life implies different things to different people. A variety of definitions can be found in the literature, elaborated by different authors, which highlight distinct meanings of quality of life, such as importance attached to life, conditions necessary for happiness, satisfaction from a personal, subjective view and so on (Carr et al., 2003, p. 133).
Revicki and Kaplan (1993), come with a different utilitarian definition: ”quality of life reflects preferences for certain states of health that allow improvements of morbidity and mortality and which are expressed by a single weighted index- standardized years of life, depending on the quality of life” (p. 88). Carr and Higginson (2001) tried to uncover what determines the quality of life through the following 4 aspects degree to which own hopes and ambitions are realised in everyday life; person’s perception of their standing in life, in the cultural and axiological background in which they are living and in relation to their goals, expectations, standards and concerns; evaluation of own health status, by reference to an ideal model; things considered important in people’s lives (pp. 1357-1360). Another key requirement needed to ensure the quality of life in a person’s life is the pursuit of both subjective and objective wellbeing (Kahneman et al., 1999, p. 98).
Research Questions
A multidisciplinary approach is required in order to treat a child who has cerebral motor deficit. Once the diagnosis is established, the infant/child should be assessed by a multidisciplinary rehabilitation team, comprehensively. These team members vary, depending on their availability as well. Among potential members of this team are included: a psychiatrist, a paediatrician specializing in development, orthopaedist, neurologist, physiotherapist, occupational therapist, speech therapist, therapeutic recreation specialist, orthotics specialist, psychologist, social worker and nutritionist. They should collaborate, exchange ideas, and constantly improve their working methods with other specialists, communication and understanding being the strength of most interdisciplinary teams. At the same time, they must be committed to a common mission, with common goals and objectives. They need to be competent, with appropriate experience and training, sufficient resources and organisational support. In addition to these, a specialist can also be appreciated for their high standards, always evaluating their individual and group performances.
Purpose of the Study
The primary goal is to promote an increased quality of life for these children using combination therapies. The aim was thus to apply early and correct therapeutic intervention to children with disabilities, including children with Cerebral Motor Deficit, and to promote good collaboration between the various specialised professionals.
Research Methods
Over the course of this research, a series of methods was used to ensure the theoretical foundation of the theme, but also to obtain potential suggestions that represent the ways to solve the proposed objectives. The research methods used for this paper were the following: literature and interdisciplinary literature review; questionnaire survey method; statistical-mathematical method; graphical method.
Findings
The research was conducted over 12 months’ time, on a number of 30 families with children who had been diagnosed with Cerebral motor deficit and related conditions.
Research hypothesis
When combination therapy is implemented, the quality of life in children with Cerebral Motor Deficit can be positively impacted; these therapies, harmoniously combined in a personalized treatment, have a major contribution to the smooth recovery of these beneficiaries.
Techniques to measure quality of life
In this research, we used the questionnaire called Family Quality of Life Survey: Main caregivers of people with intellectual or developmental disabilities (Brown et al., 2006, p. 173). By this questionnaire we were able to record the perception on the quality of life seen from within, precisely by the ones directly affected, which as a matter of fact, is most pertinent to this research. The Family Quality of Life Survey is a method of focusing attention on the quality of life for families with one or more members with intellectual or developmental disabilities. Moreover, it is also a way of investigating the difficulties faced by families and the degree to which they perceive their own quality of family life as enjoyable, valuable and supported by the kinds of resources that are important to family members. We used this questionnaire as a tool to describe and measure the quality of family life for strictly evaluation and research purposes. All personal information of family members was protected, making public only statistical data. Family quality of life can be approached from several perspectives. The questionnaire includes aspects of family life considered as essential, based on previous research and practice. The Quality of Family Life Assessment Questionnaire was, in each case, completed by the main carer of the family member with an intellectual or developmental disability, which generally took about one hour.
Research results
As this was a large-scale questionnaire, aiming to review quality of life from all standpoints, we chose to detail the results we obtained in the second section, first part, i.e. “Family health , referring to this research’s topic specifically. Also, the satisfaction degree of the respondents’ family with regard to all the other sections featured by the questionnaire shall be presented as well, in order to have a wider view of these families’ quality of life, as seen from within. Names and surnames of respondents have not been disclosed in this paper for confidentiality reasons. The introductory questions of the questionnaire administered, found in the first section: “About your family” allow for details of particular relevance.
Two important aspects have to be underlined:
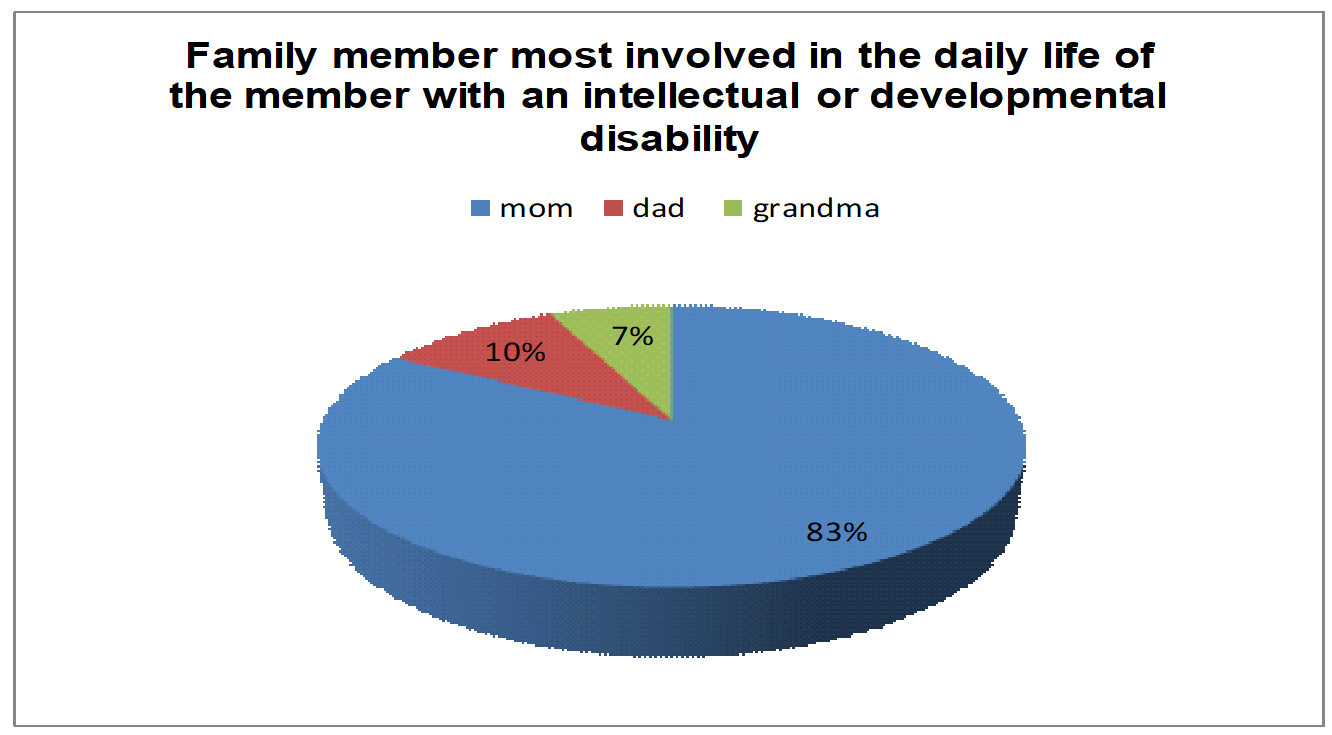
In 25 of the 30 families subject to the study (figure 1), Mother’s predominant involvement in everyday life of the member with intellectual or developmental disability was noted, the mother being the one to complete the questionnaire. For the remainder of 5 cases, the most involved family member in everyday life of the member with intellectual or developmental disability was the father in 3 cases, and the grandmother in 2 cases.
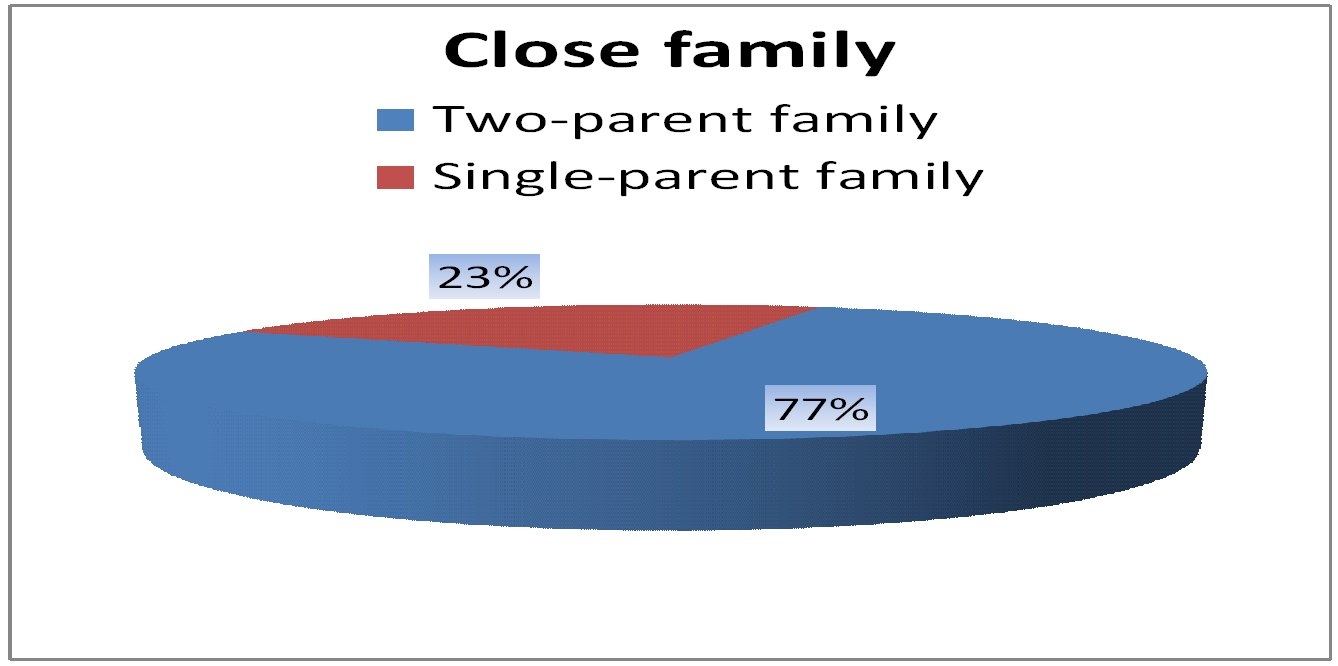
In 23 of the respondents (figure 2), the close family consisted of two-parent family, and the remaining 7 were found to be single-parent families.
The results of the second section, first part, i.e. “Family health” are shown below.
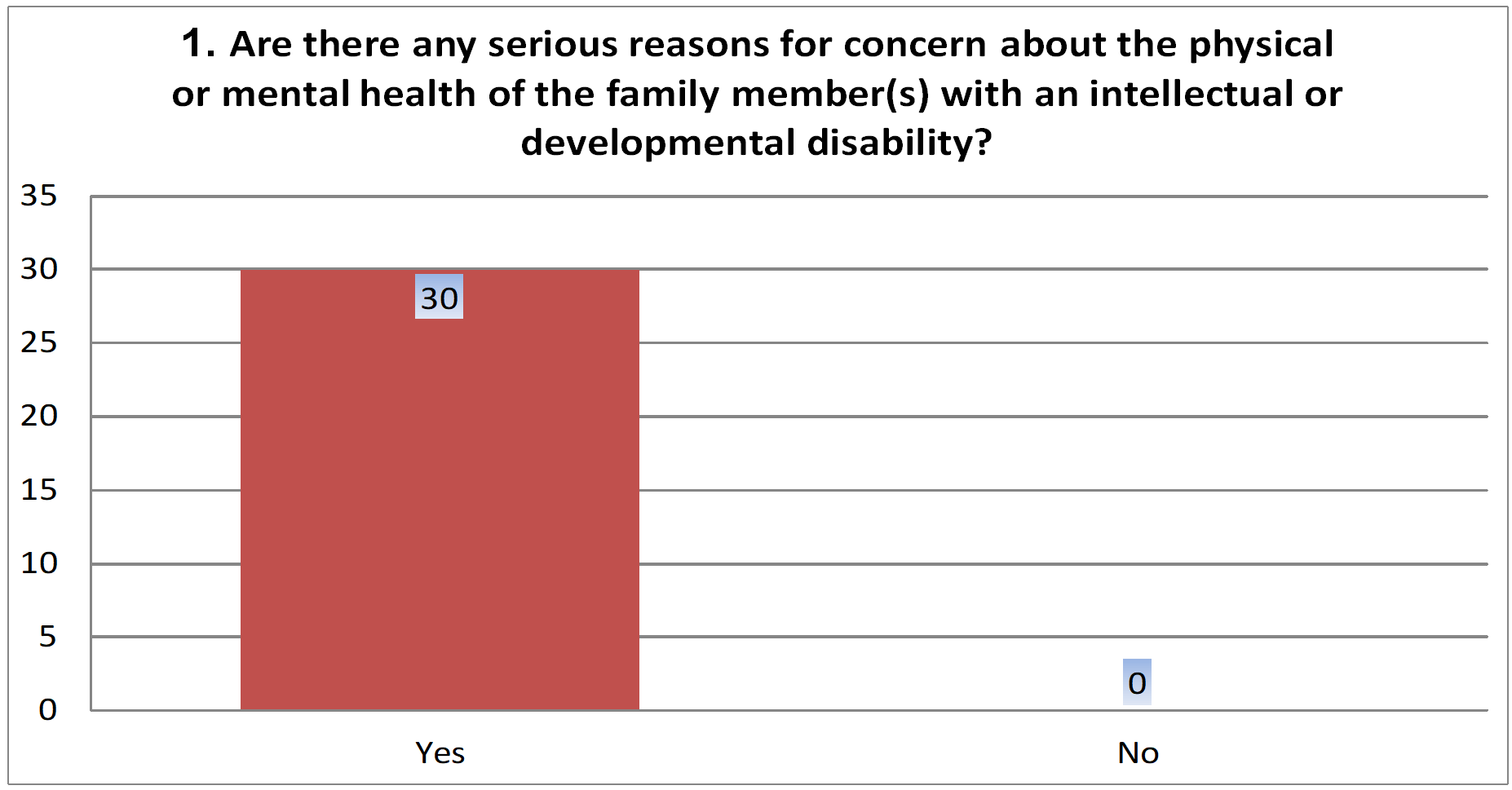
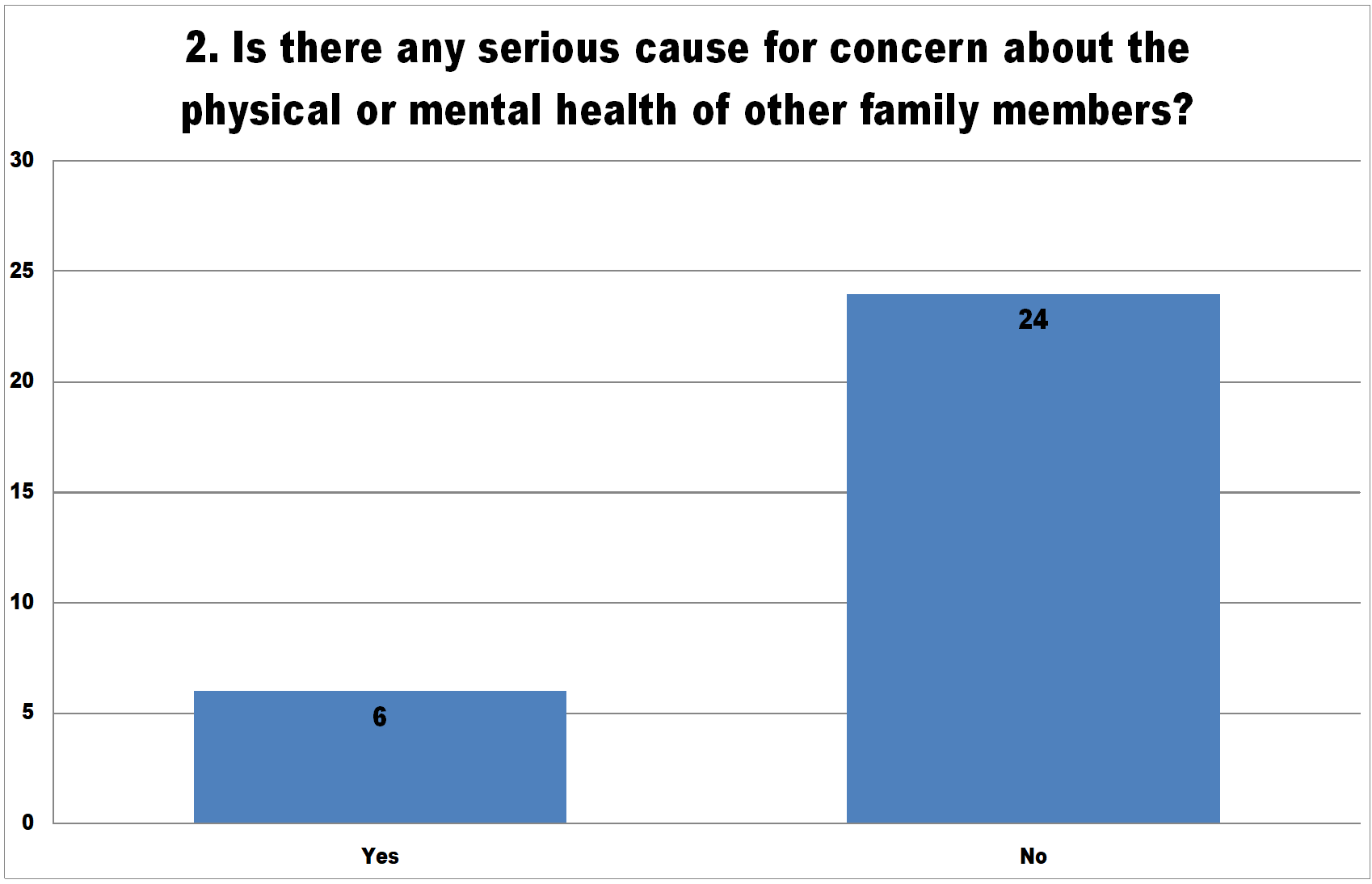
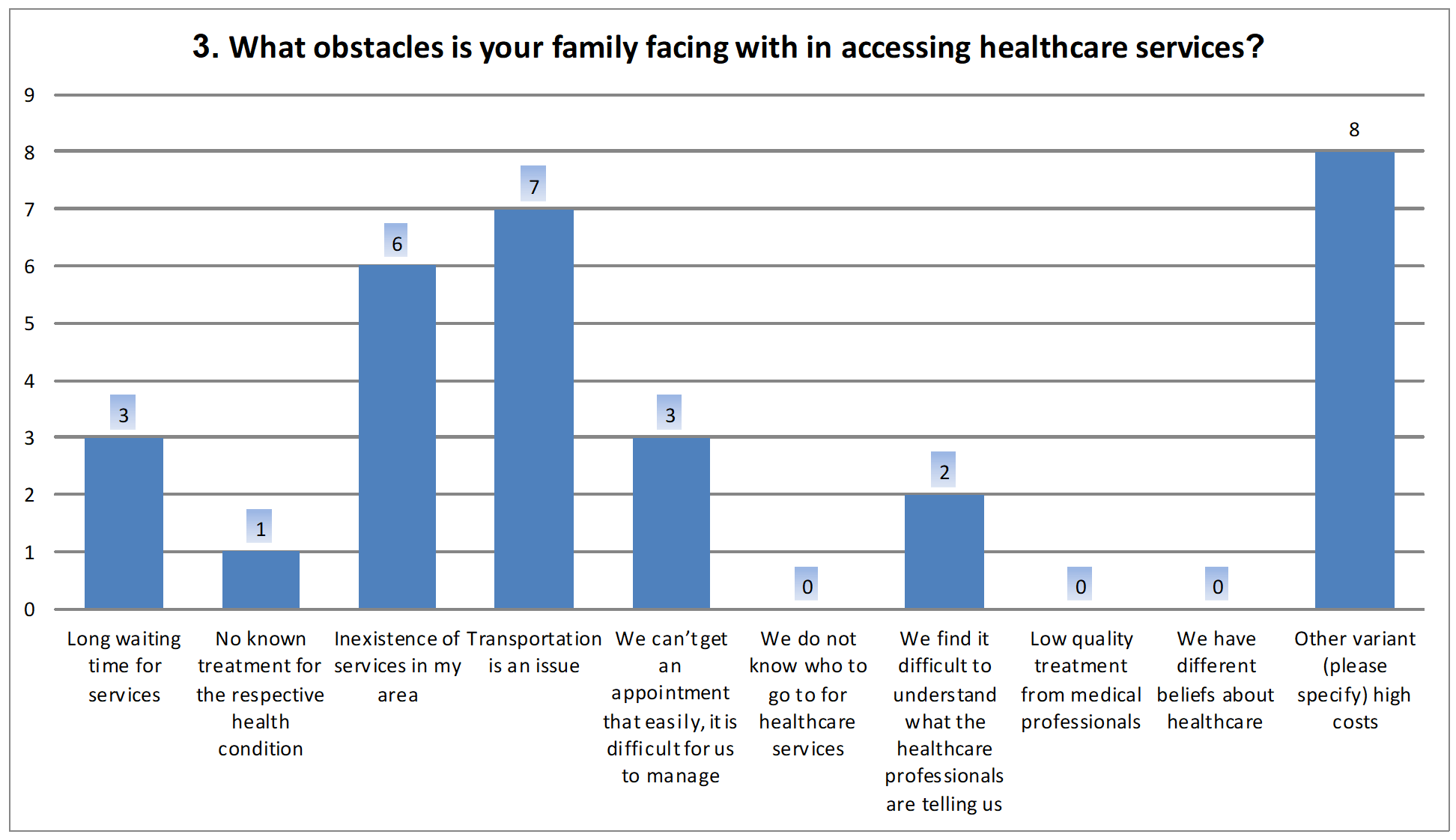
Section A revealed that all respondents believe they have serious reasons for concern about the physical or mental health of the member (s) with intellectual or developmental disability: 6 out of them were concerned for the physical or mental health of other family members as well and each separate family was facing with various obstacles in accessing healthcare services, as shown by the following figure 3, 4 and 5.
Section B contains questions about 6 basic concepts for the instrument’s theoretical construction: importance, opportunities, initiative, accomplishment/ current status, stability and satisfaction.
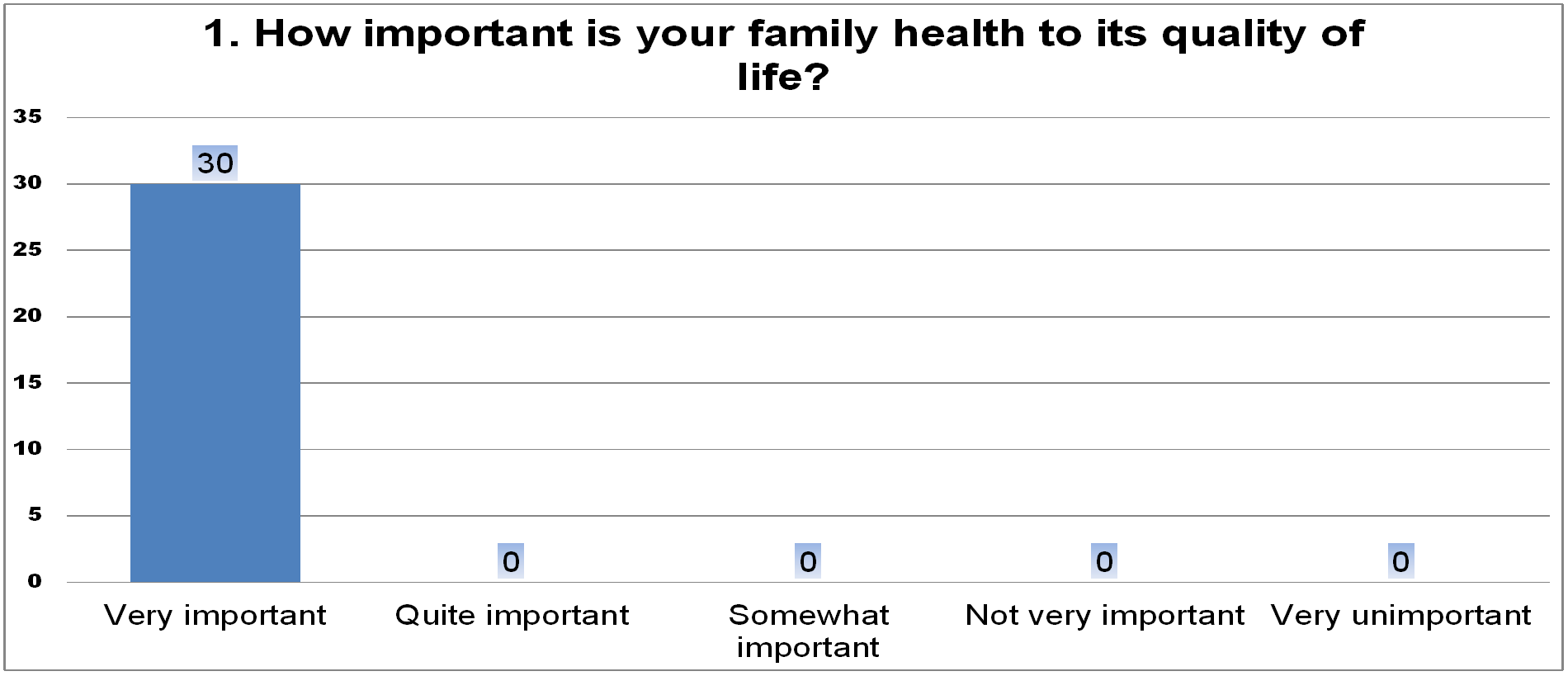
Not surprisingly, 100% of respondents replied that health was very important to their quality of life, figure 6, 7, 8, 9, 10, 11.
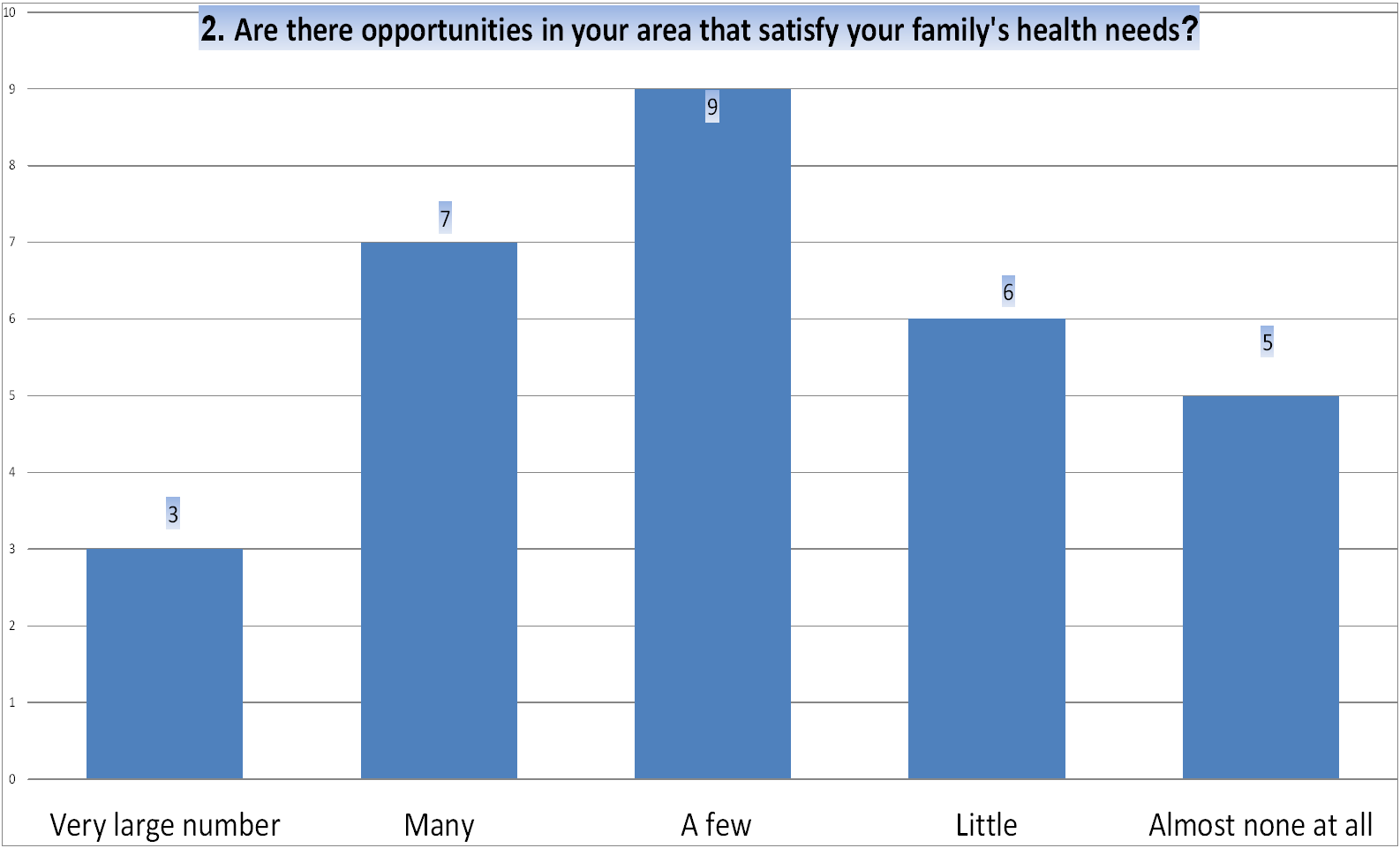
When asked to right down whether or not there are opportunities satisfying their family health’s needs in their area, replies were very different, as follows:
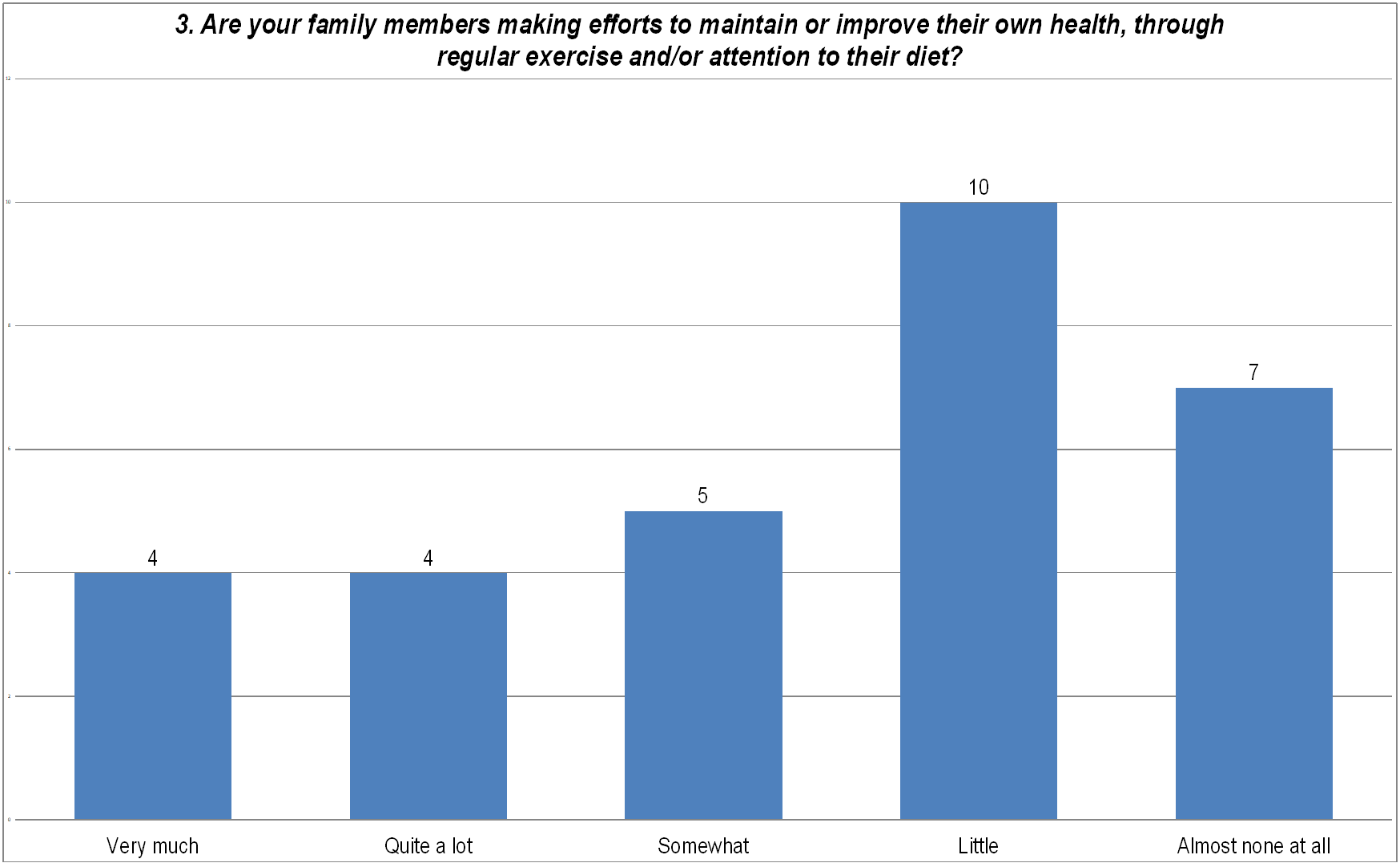
In terms of the other family members’ involvement in the support or improving their own health, by regular exercise and/or attention to diet, all with a view to optimizing quality of life, the finding is that the vast majority of people surveyed replied that they were doing little effort to the respective direction.
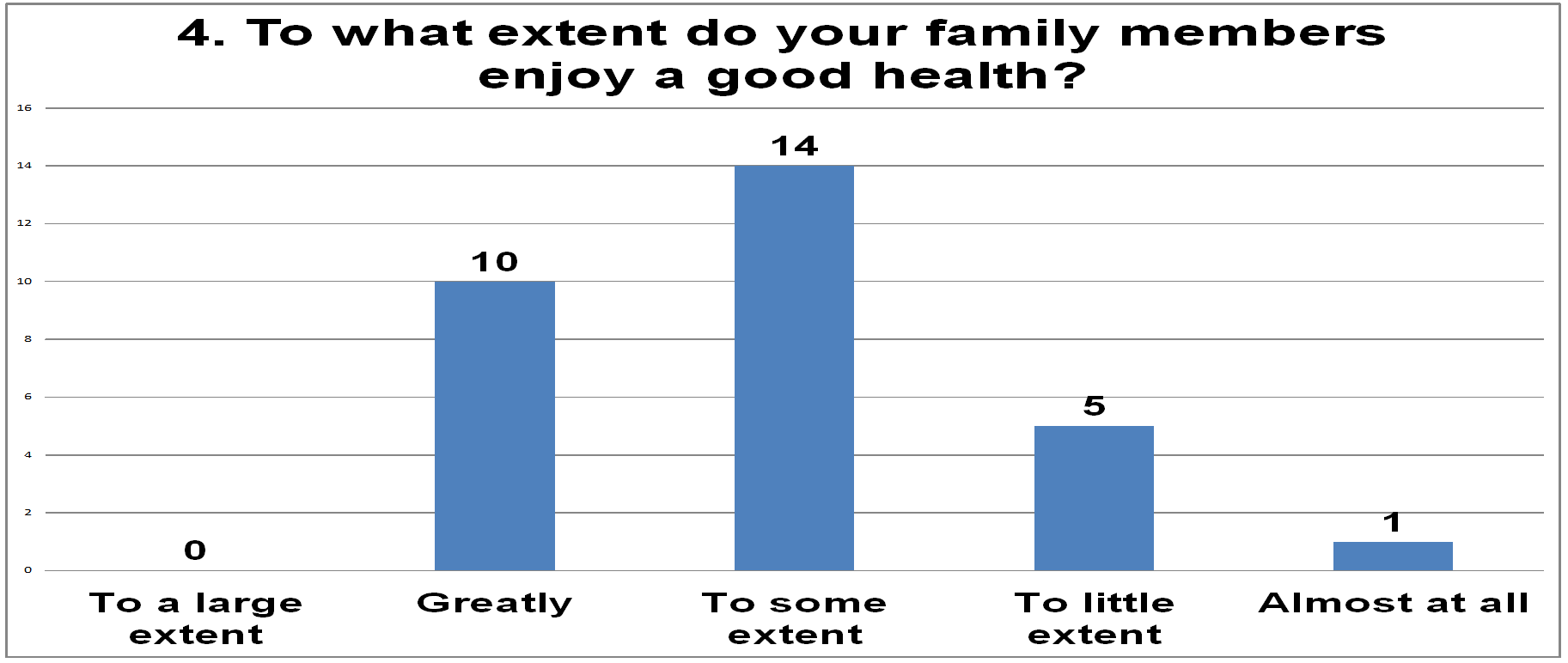
The current health status of the other family members, judging by the replies given, seems to be somewhere in the middle, enjoying health to some extent. The encouraging thing is that the next highest response was that they enjoyed their current health “to a large extent”.
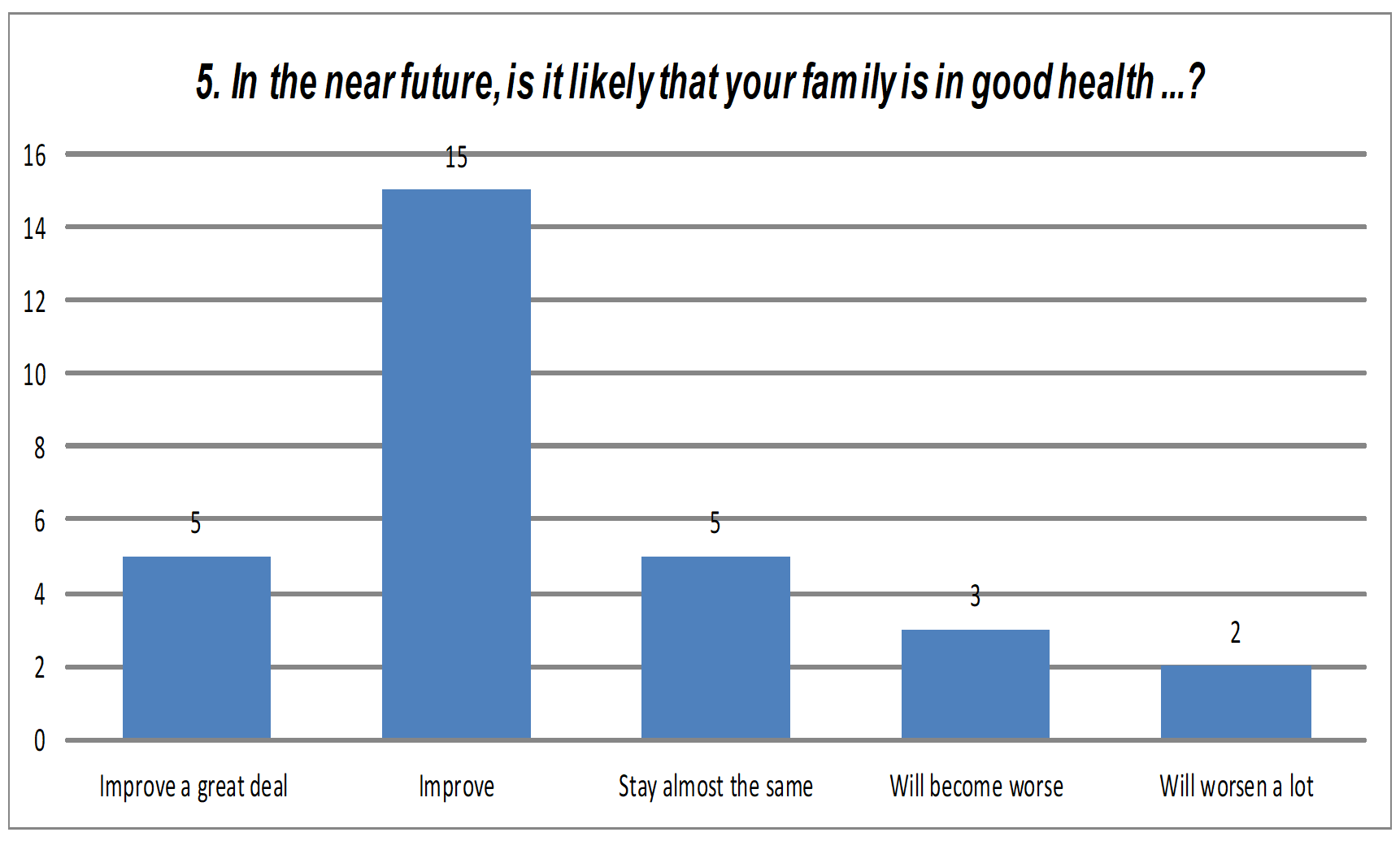
Family predictions on how the family’s health status will develop were favourable, families being largely convinced that health will improve in the future.
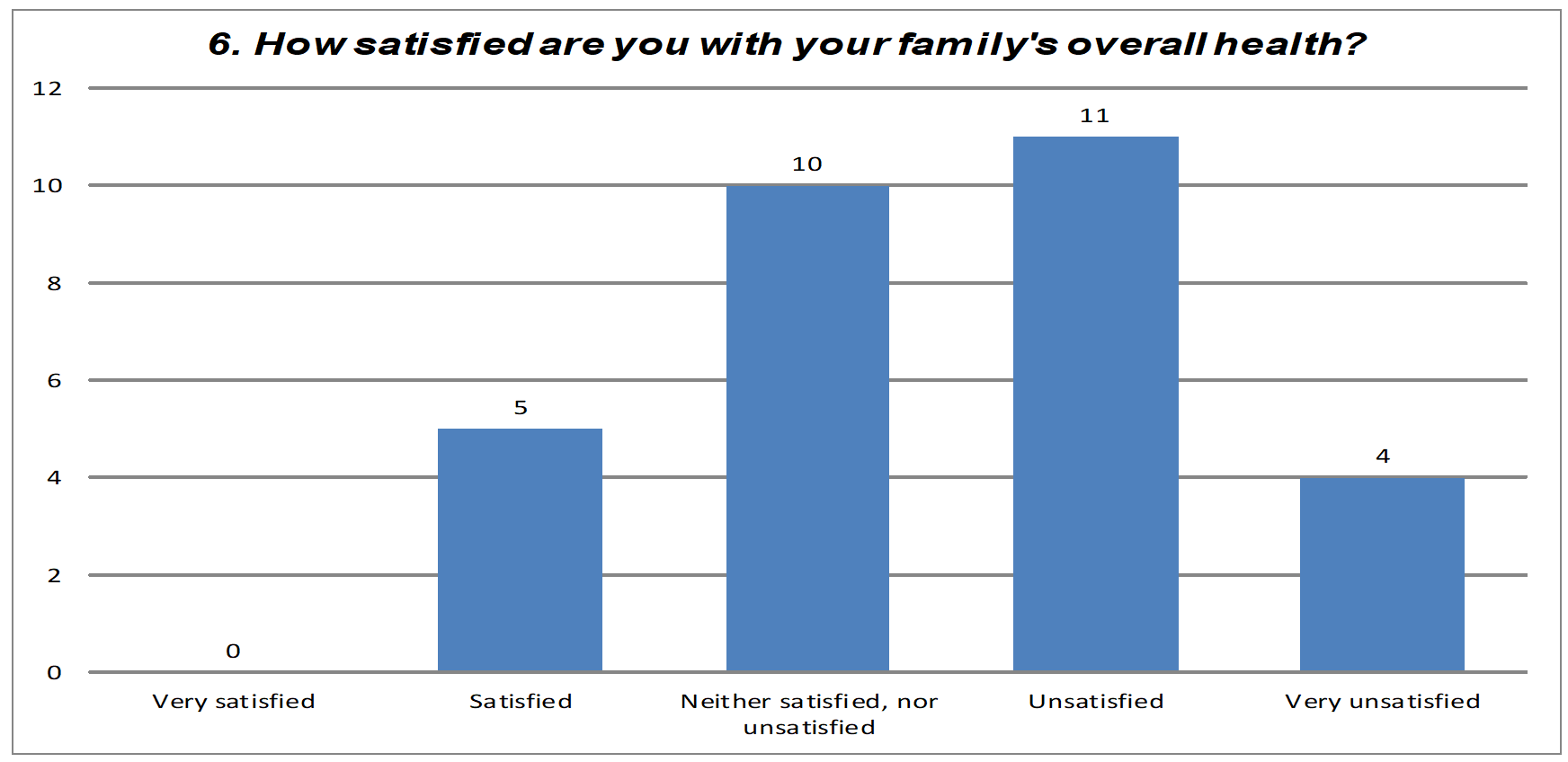
The final and most important question in this section refers to the satisfaction degree on family health, as a whole. Thus, in terms of health, it can be seen that the majority of respondents consider the quality of their family life to be unsatisfactory.
The next sections deal with specific fields of family life: financial well-being, family relationships, support from others, and support from services, and influence of values, career, leisure and recreational activities, integration into community life. The focus will be on the last question in section B within each aspect separately.
Next, the vision of families surveyed on their satisfaction degree with regard to all these sections, presented in the survey, will be discussed.
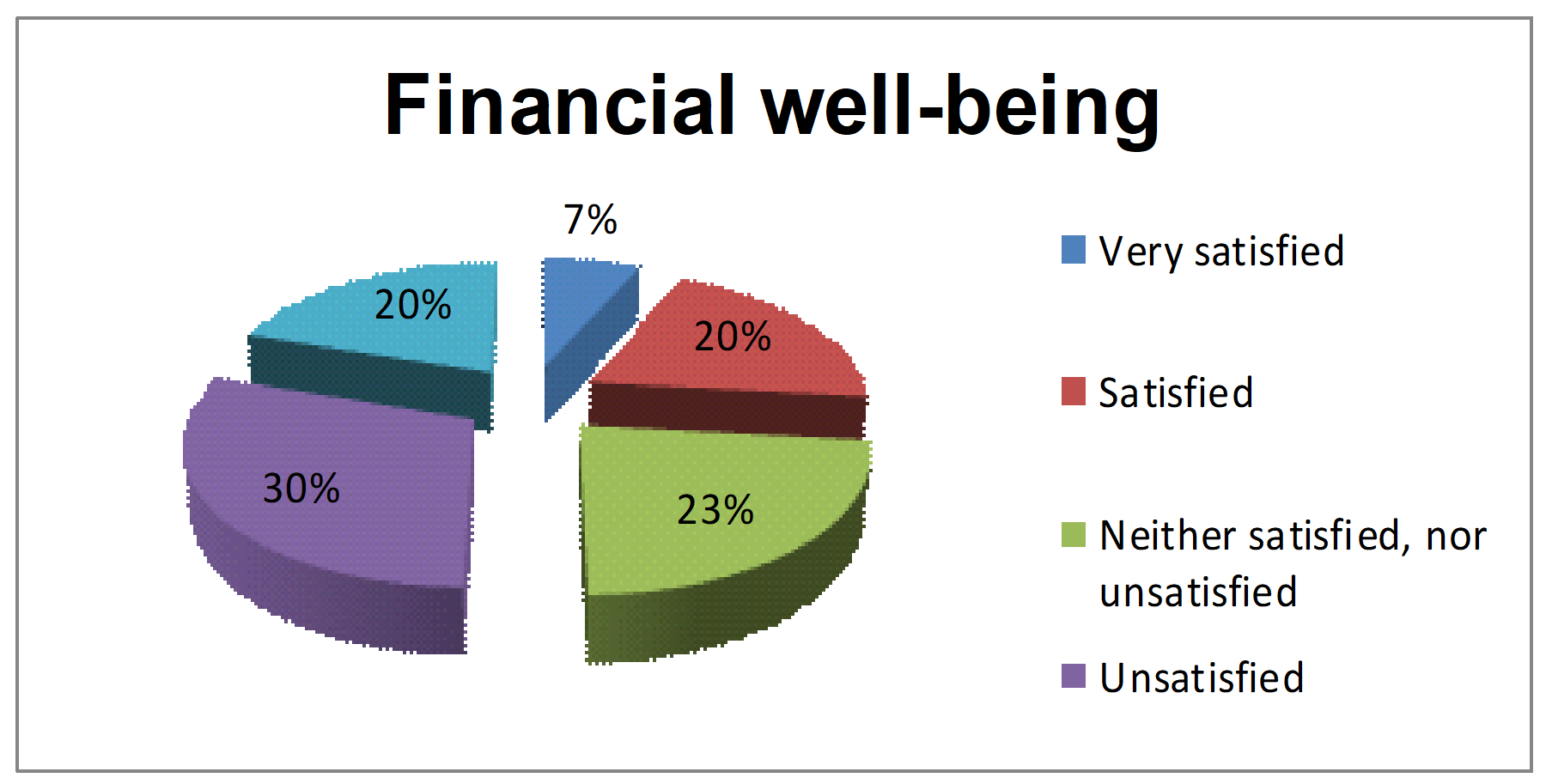
With regard to the satisfaction about financial situation of families with a child suffering from CP, the 30 respondents replied as follows, to figure 12:
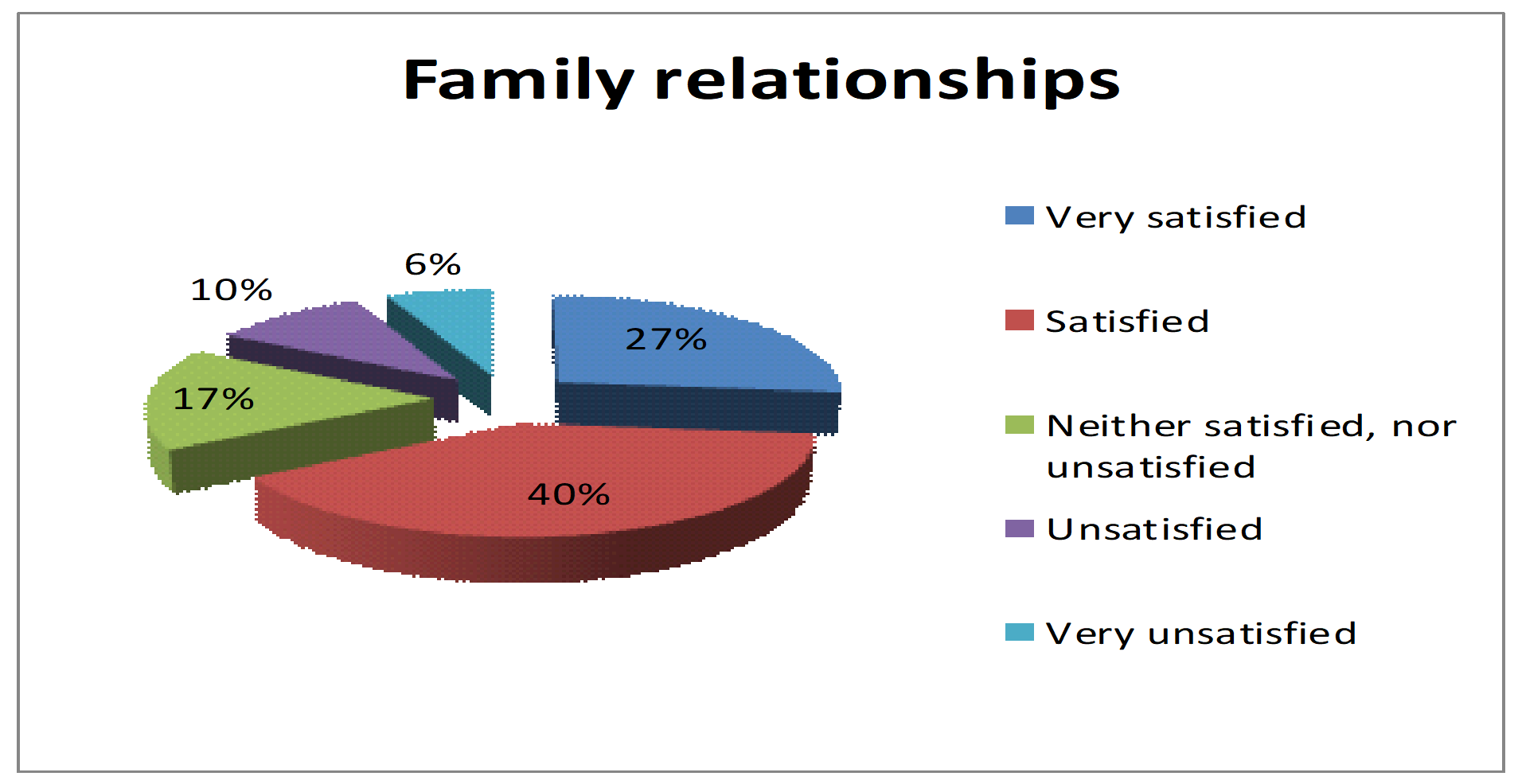
Results show that Family relationships (figure 13) are deemed as satisfactory by 40% of respondents to this questionnaire, standing for a majority, followed by those to have replied by “Very satisfied” (27%). The number of people to have identified with the less optimistic options to this question about family relationships was lower, but it would be inappropriate to dismiss them.
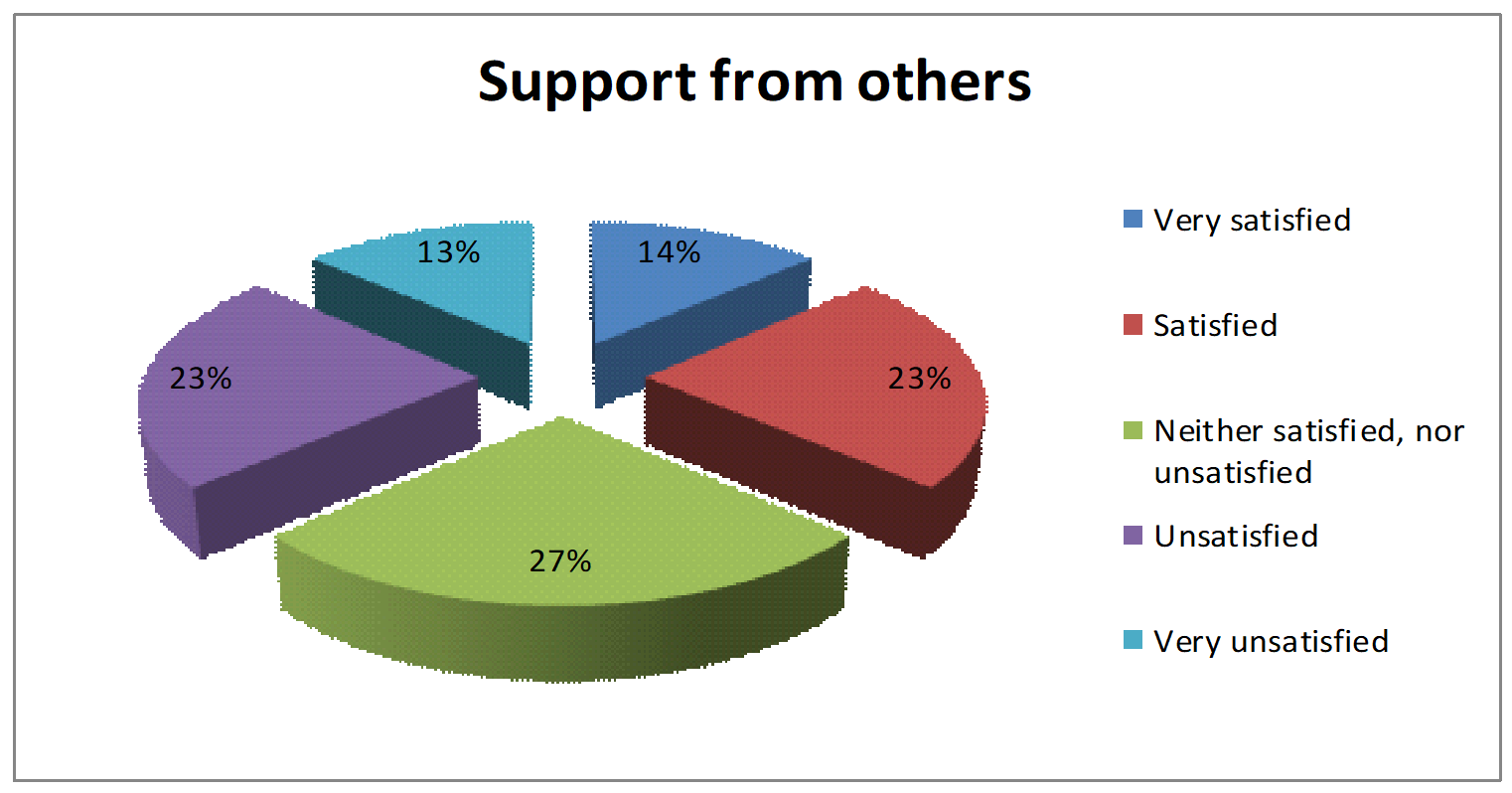
Things seem to be somewhere in the middle in terms of support given by other people (figure 14) to families with children suffering from CMD. The vast majority of replies were:” Neither satisfied, nor unsatisfied” , the rest being similar in percentage: “ Satisfied/ Unsatisfied summing up 23% of replies and “Very satisfied/ Very unsatisfied reported 13%, 14% respectively.
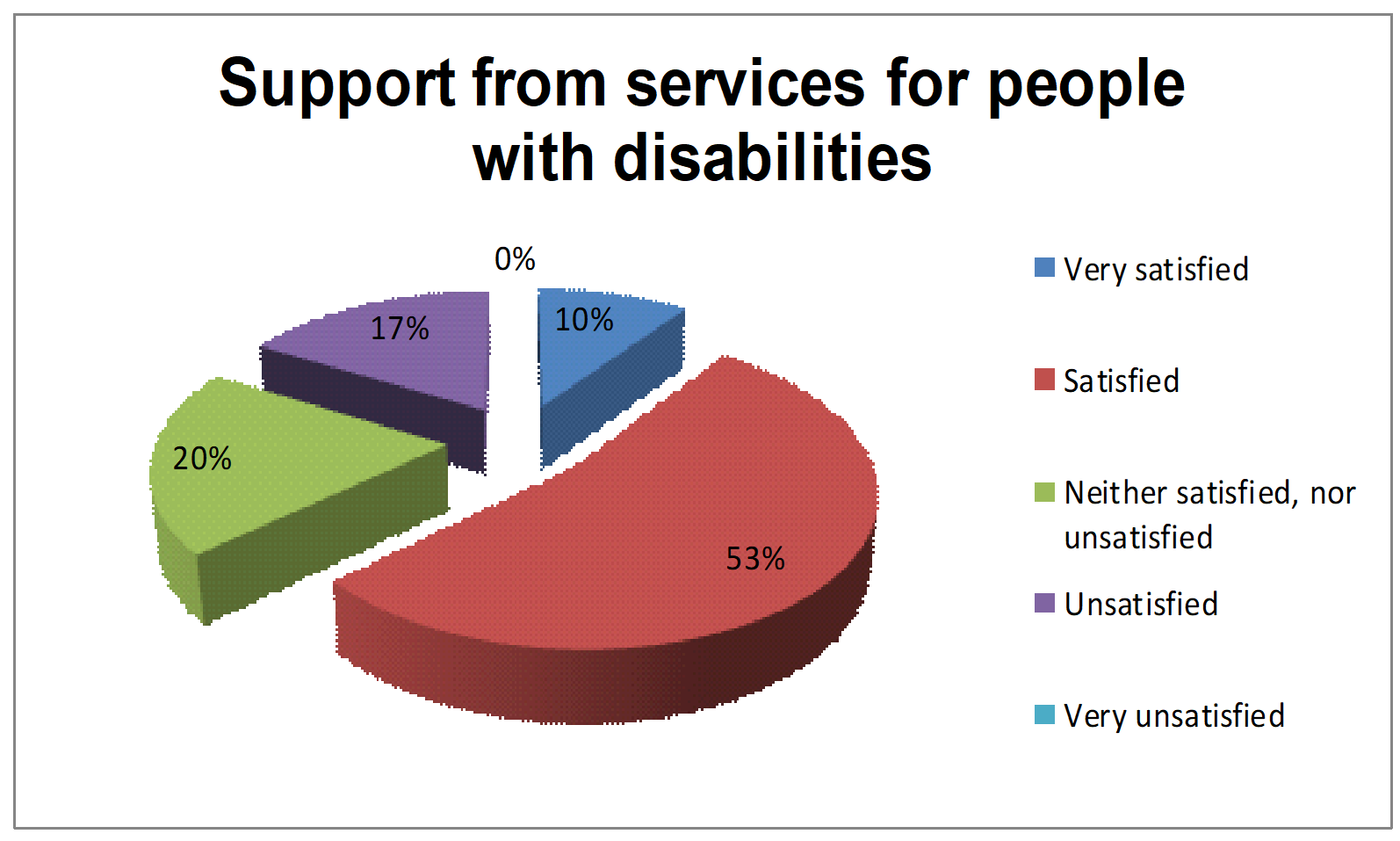
Support from services granted to people with disabilities (figure 15) was evaluated as “Satisfactory” by more than half of the respondents.
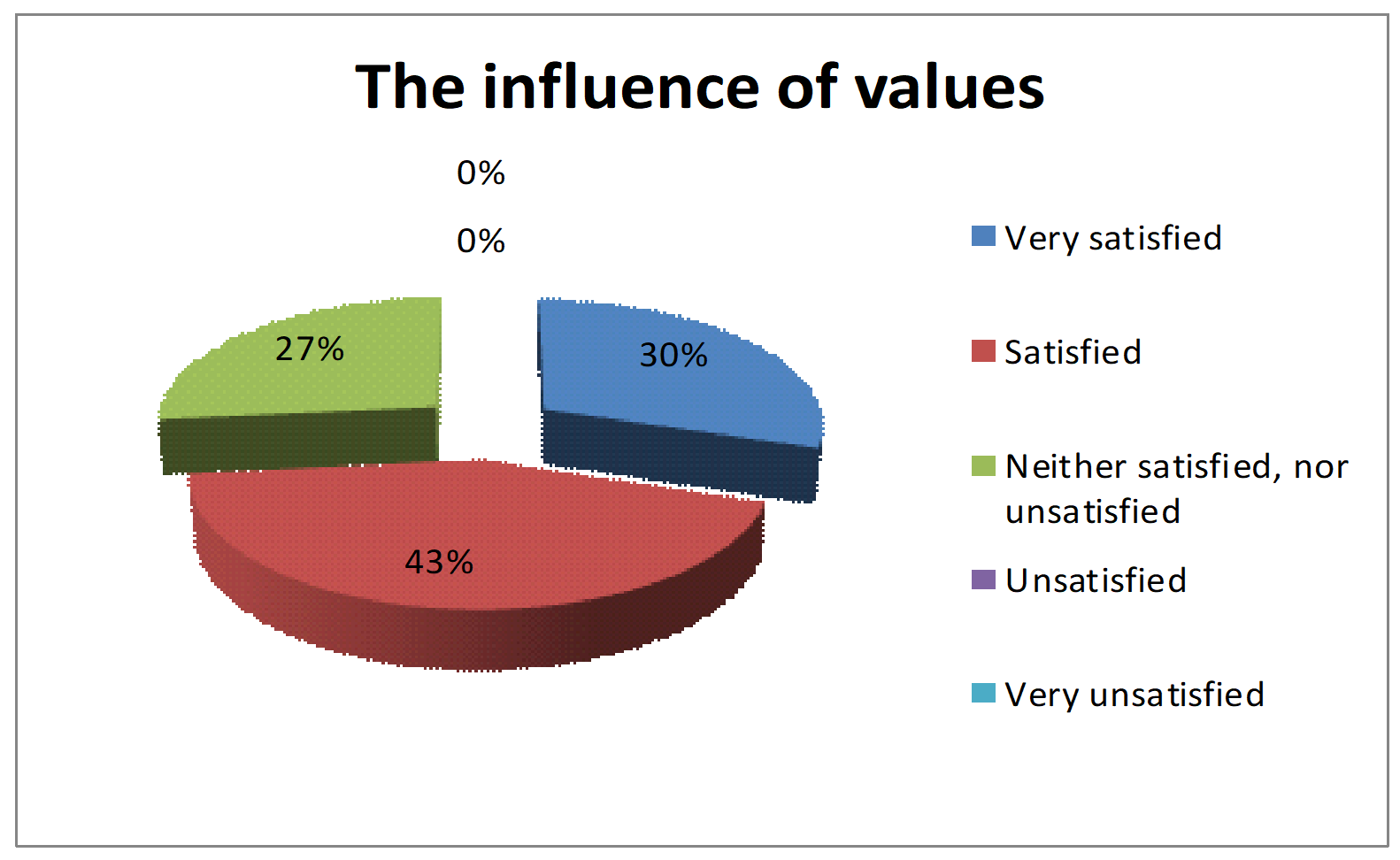
The same grade was given to:(figure 16) by 43% of respondents, 30% replied by “Satisfied” and 27% by “Neither satisfied, nor unsatisfied”.
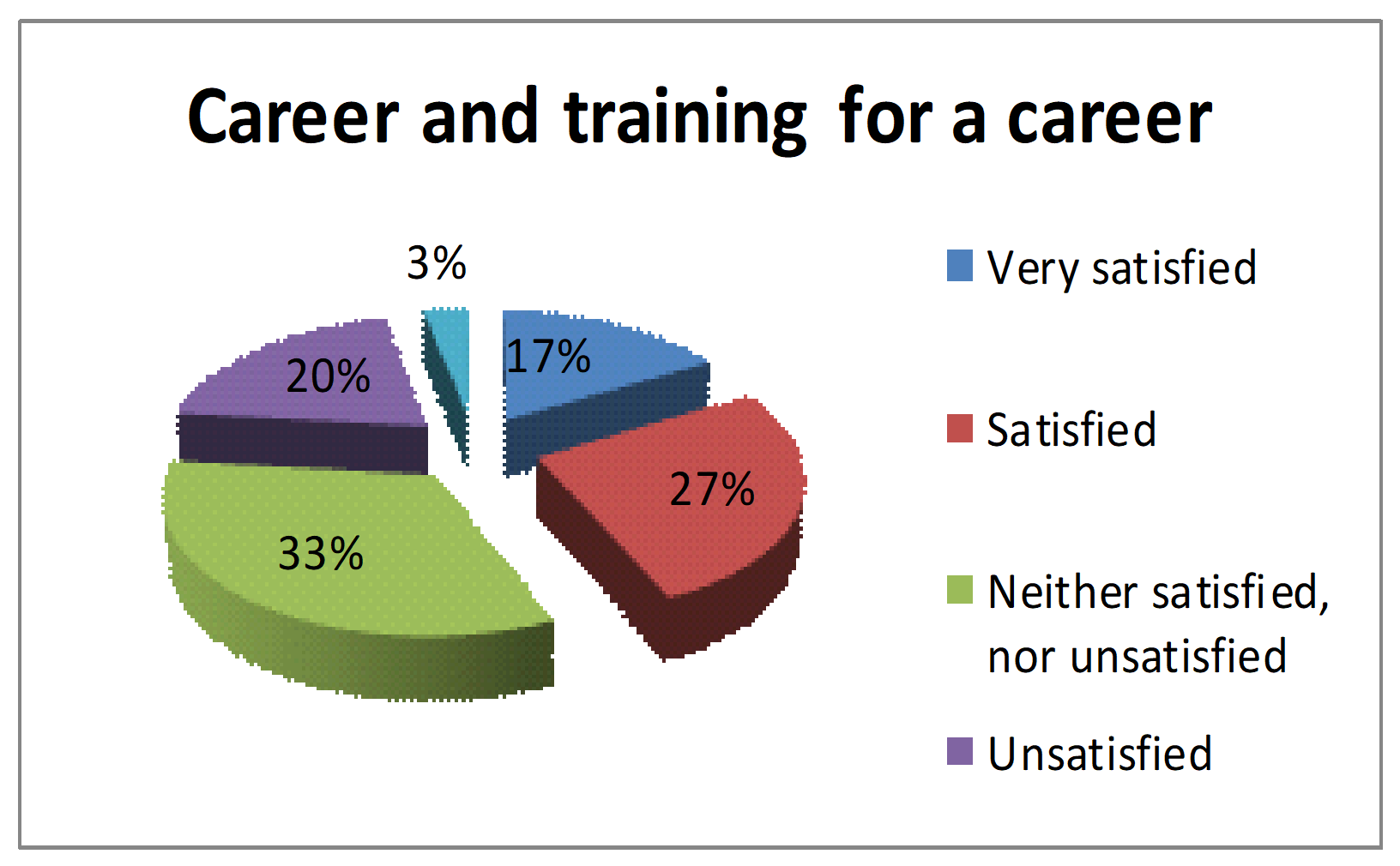
Replies concerning the career and training for a career (figure 17) were preponderantly (33%) graded by “Neither satisfied, nor unsatisfied”, followed by a percentage of 27% of the option “Satisfied”, 20% being unsatisfied, 17% very satisfied and only 3% unsatisfied.
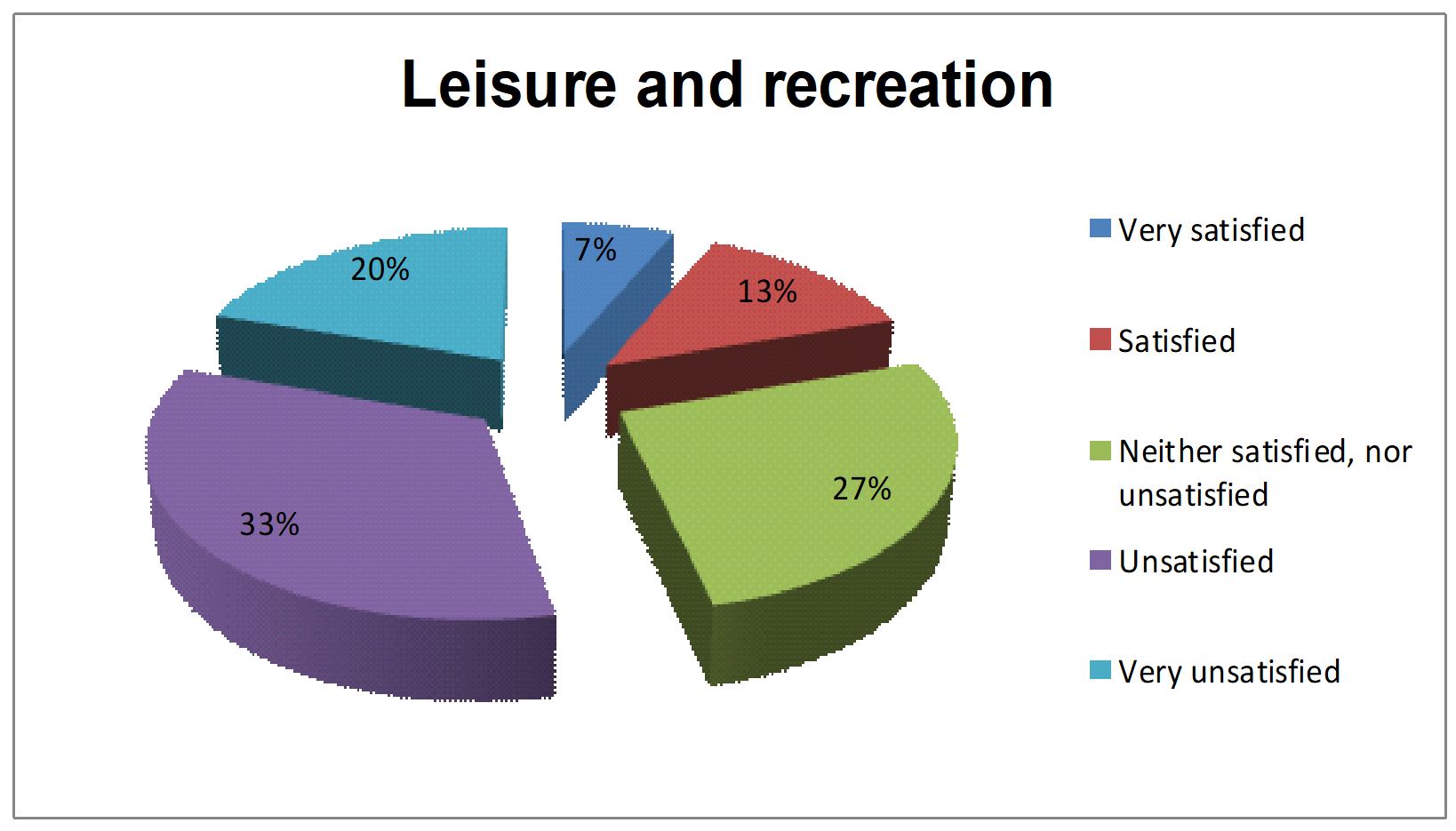
A percentage of 33% of respondents were unsatisfied with leisure and recreation activities of the family, (figure 18) showing just how important time is in everyday life. In this case, the lowest percentages were reported by those who were very satisfied or satisfied.
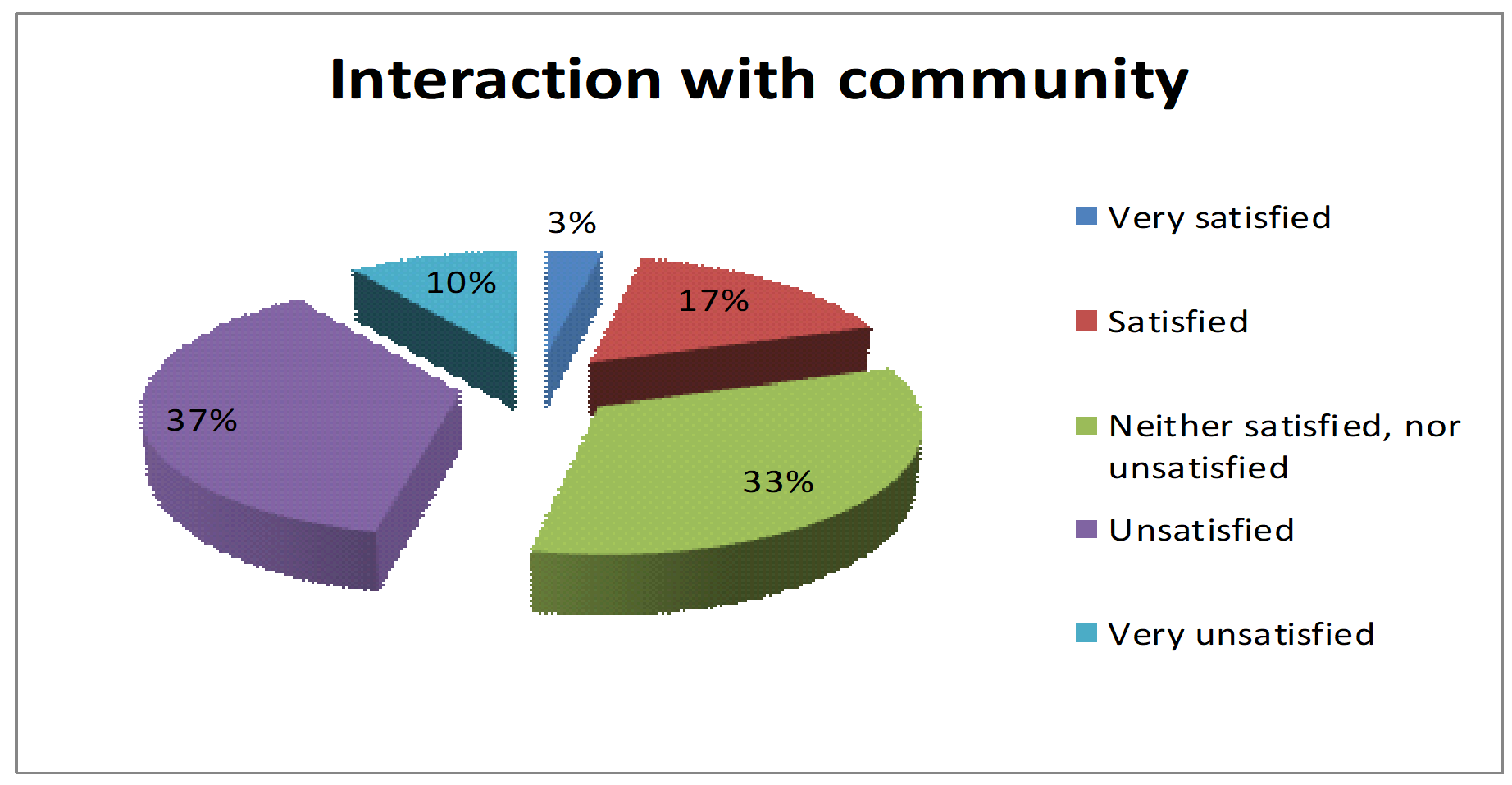
Replies given by respondents to the section on interaction with community (figure 19) were not positive, rather they were negative, a large part (33%) consisting of “Neither satisfied, nor unsatisfied”.
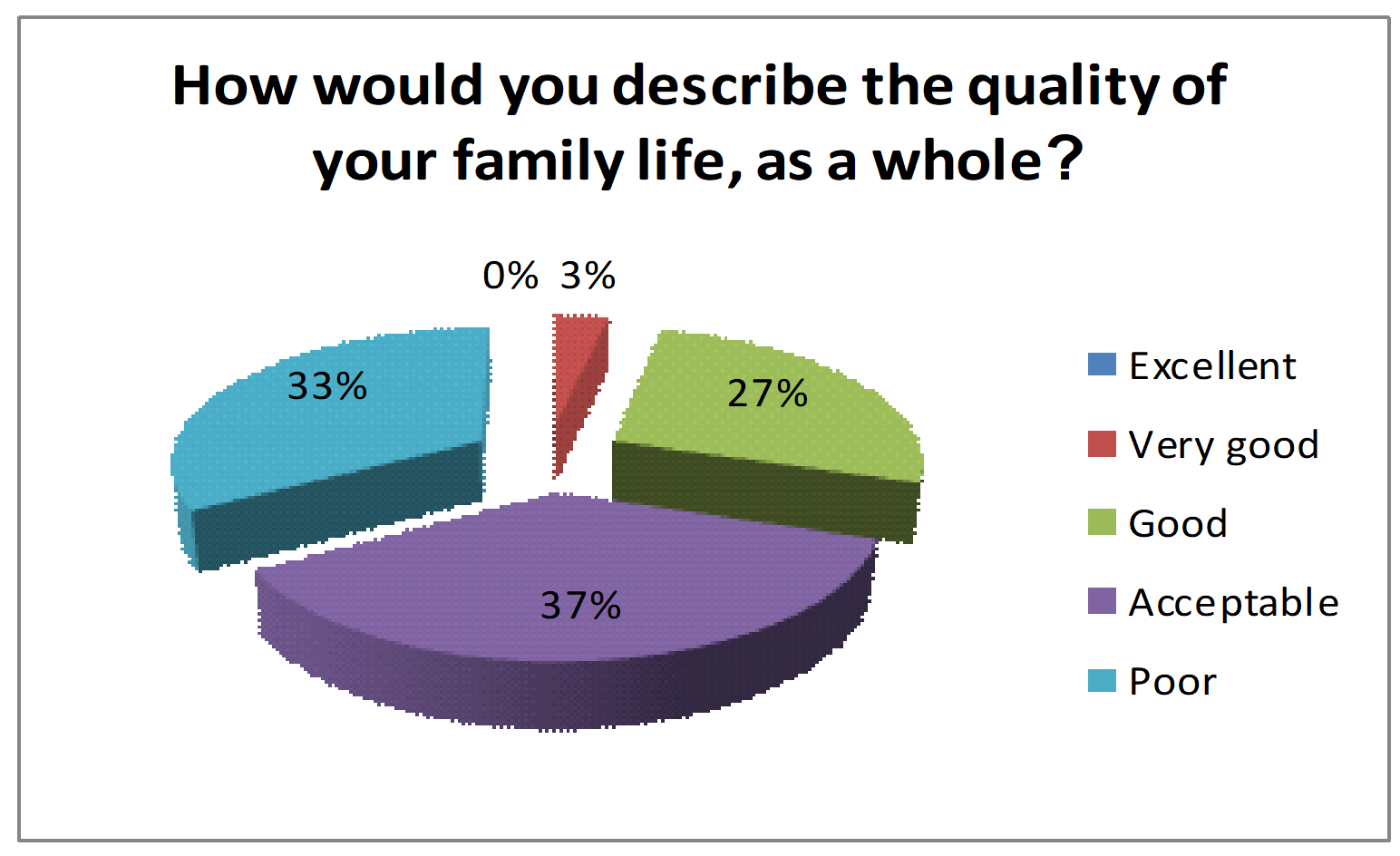
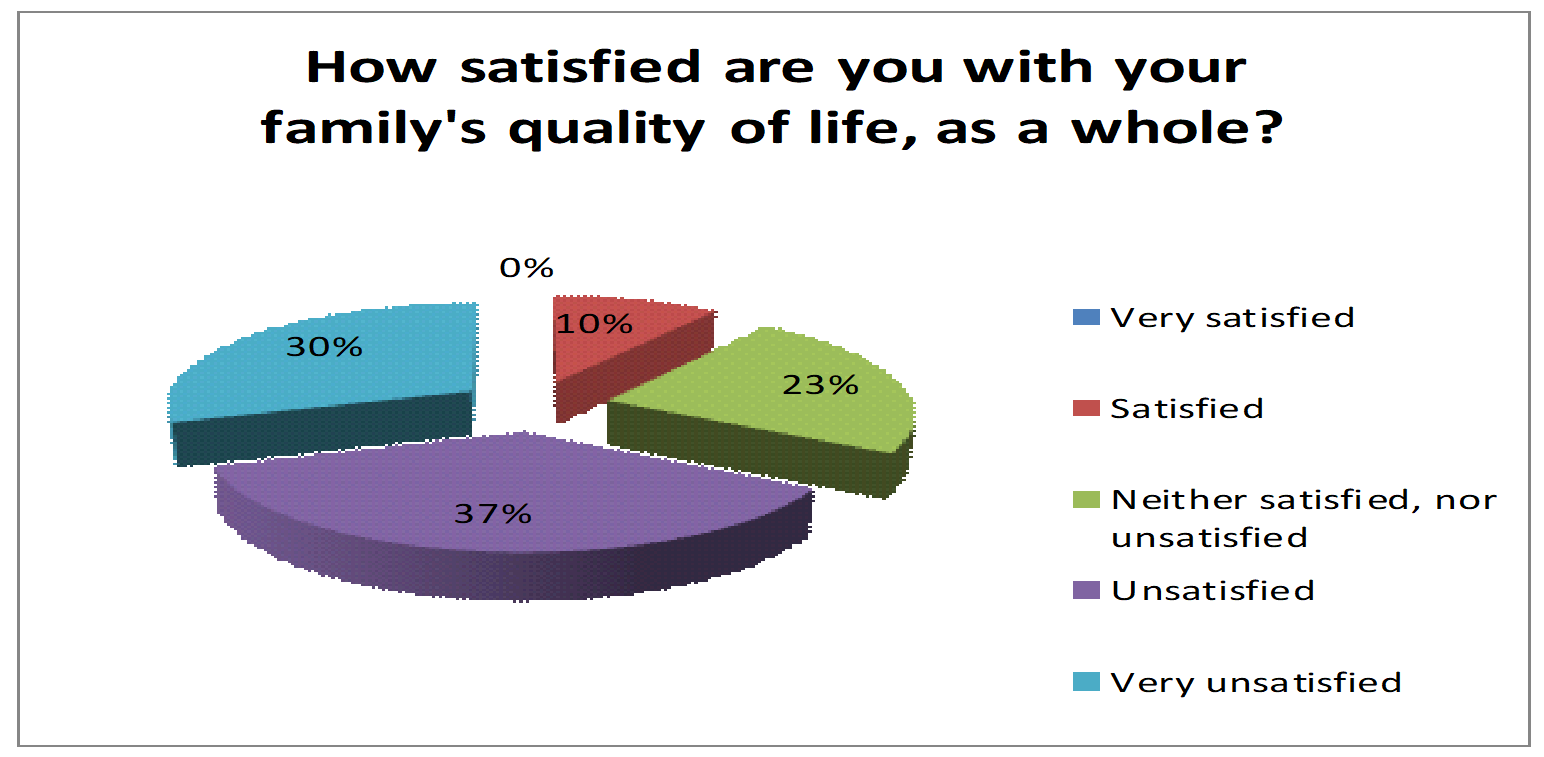
The final, shorter part of the Survey was intended to gathering general impressions on the quality of family life, figure 20 and 21. Thus, to conclude, the results of the last two questions in the survey shall be presented, general in nature, on the quality of family life as a whole.
When asked to describe their own quality of life, 37 % of those surveyed described it as “Acceptable”. It was described as “Poor” by 33%, “Good” by 27% and only 3% believed it to be “Very good”. However, nobody responded that they would describe their overall family life as “Excellent”.
Results to the last question were not very different from the one before, registering the same percentage (37%) for those to have replied by “Unsatisfied”. Next, there were those with “Very unsatisfied” by a percentage of 30%, then “Neither satisfied, nor unsatisfied” by 23% and those who were “Satisfied” in a percentage of 10%. Again, as in the previous question, there was no reply by “Very satisfied”.
Conclusions
Although it refers to an irreversible damage, Cerebral Motor Deficit’s symptoms and manifestations can improve, producing various adaptive processes, through the use of various treatment methods.
Efficient measurement of the quality of life in children with Cerebral Motor Deficit is also important. Also, in such cases, seeing that it is impossible to question/ interview the child with Cerebral Motor Deficit, the quality of family life of the member with disabilities is assessed, as it is conclusive to the child’s quality of life.
This research confirms just how important physical and mental health’s influence over family quality of life is and, implicitly, over the child with cerebral motor deficit.
Balanced parental style is the one to sustain good quality of life for a child with cerebral motor deficit; children in such families are described as happy, approved, bold, sociable, kind and skilled.
Early diagnosis of children with cerebral motor deficit allows for early therapeutic intervention and detection of other related symptoms, since Cerebral Motor Deficit is a title, not consisting of just one aetiology.
A multidisciplinary approach, with a common mission, goals and objectives is a must.
Accurate knowledge of existing treatment methods for children with cerebral motor deficit makes a realistic, correct planning of objectives and ways to reach them possible.
Using combination therapies for children with cerebral motor deficit favours the improvement of quality of life from all points of view, not just with regard to physical development, but also cognitive, social etc.
Administration of the “Family Quality of Life Survey: Main caregivers of people with intellectual or developmental disabilities- 2006” also helps assess the quality of life for the child with cerebral motor deficit, being a starting point for setting treatment objectives and methods to be applied.
Adopting a balanced parental style is necessary to enhance the child’s quality of life and self-confidence.
Promotion and implementation of combination therapies applied early and continuously help improve the quality of life for the child with cerebral motor deficit and that of their family as well.
References
Albu, C., Gherguţ, A., & Albu, M. (2007). Dicţionar de kinetoterapie, versiune printată [Kinetic therapy dictionary, Printed version]. Editura Polirom, Iasi, Romania.
Alexander, M. A., & Matthews, D. J. (2010). Pediatric Rehabilitation – Principles and Practice. Demos Medical Publishing.
Bobath, K. (1966). The Motor Deficit in patients with Clinics in Developmental Medicine, no. 23. S.I.M.P. with Heinemann Medical, Philadelphia, Lippincott.
Brown, I., Brown, R. I., Baum, N. T., Isaacs, B. J., Myerscough, T., Neikrug, S., Roth, D., Shearer, J., & Wang, M. (2006). The family life quality assessment questionnaire for the main caregivers of people with intellectual or developmental disabilities [Chestionarul de evaluare a calităţii vieţii familiei pentru principalii îngrijitori ai persoanelor cu dizabilităţi intelectuale sau de dezvoltare-. traducere în limba română: Manuela Oprea]. Surrey Place Centre.
Carr, A. J., & Higginson, I. J. (2001). Measuring quality of life: Are quality of life measures patient centered?. British Medical Journal, 2001 Jun 2;322(7298), 1357-1360.
Carr, A., Higginson, I., & Robinson, P. (2003). Quality of life. BMJ Publishing Group, BMJ Books, 2003.
Hagberg, B., & Hagberg, G. (1984). The changing panorama of cerebral palsy in Sweden. IV. Epidemiological trends 1959-78, ACTA Pediatrica, 1984 Jul; 73(4), 433-440.
Kahneman, D., Diener, E., & Schwarz, N. (Eds.) (1999). Well-Being: Foundations of Hedonic Psychology. New York, NY: Russell Sage Foundation.
Le Metayer, M. (1999). Reeducation cerebro-motrice du jeune enfant. Education therapeutique [Cerebromotor rehabilitation in young children. Therapeutic education]. Masson Editeur.
Menkes, J. H. (1995). Textbook of child neurology, 5th edition. Williams and Wilkins, Baltimore.
Revicki, D. A., & Kaplan, R. M. (1993). Relationship between psychometric and utility-based approaches to the measurement of health-related quality of life. Quality of Life Research, 2(6), 477-487.
Robănescu, N. (1983). Tratamentul sechelelor motorii ale encefalopatiilor infantile-Paralizia spastică cerebrală [Treatment of motor sequelae of infantile encephalopathies- spastic cerebral palsy]. Editura Medicală.
Vereanu, D. şi colab. (1963). Experienţa Spitalului de copii “Grigore Alexandrescu” în tratamentul complex al paraliziilor spastice ale copiilor şi recuperarea lor funcţională, [The experience of the "Grigore Alexandrescu" Children's Hospital in the complex treatment of children's spastic paralysis and their functional recovery]. Editura Medicală.
World Health Organization. (WHO) (1998). The World health report 1998 Life in the 21st century a vision for all: report of the Director-General. https://apps.who.int/iris/handle/10665/42065
Yamada, K. (1994). Incidence rates of Cerebral Palsy, mental retardation and Down Syndrom in Sodeguara. Chiba Prefecture. No To Hattatsu.
Copyright information
About this article
Publication Date
10 April 2023
Article Doi
eBook ISBN
978-1-80296-961-0
Publisher
European Publisher
Volume
5
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-1463
Subjects
Education sciences, teacher education, curriculum development, educational policies and management
Cite this article as:
Toma, S., Toma, G., & Rabolu, E. (2023). Improve The Quality Of Life In Children With Cerebral Motor Deficit. In E. Soare, & C. Langa (Eds.), Education Facing Contemporary World Issues - EDU WORLD 2022, vol 5. European Proceedings of Educational Sciences (pp. 905-921). European Publisher. https://doi.org/10.15405/epes.23045.91

