Abstract
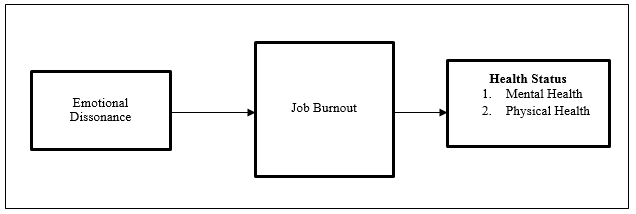
Healthcare system in a country plays an essential role in promoting the well-being of its citizens. Healthcare workers, particularly medical doctors who act as front-liners, are exposed continuously many occupational stressors due to time pressure, work overload and lack of social support at work. These occupational stressors cause emotional dissonance, which can influence their job burnout as well as to health status. Although studies on employee’s health status are voluminous, studies on factors that help predict one’s health status are still scarce. Moreover, limited attention has been given at exploring the mechanism with which emotional dissonance affects employees’ health both mentally and physically. Hence, the purpose of this paper is to review the literature and subsequently propose a model linking emotional dissonance and health status (mental health and physical health) among medical doctors in Malaysian public hospitals. The Job Demand-Resource Model and Conservation of Resource (COR) theory serves as the foundation in developing the model. Job burnout is proposed as a mediator in the relationship mentioned above.
Keywords: Emotional dissonancejob burnoutmental healthphysical healthhealthcare professionalsMalaysia
Introduction
Over the last decade, doctors were unhappy with their jobs due to feelings of overworked and lack of support (McManus et al., 2004; Siu et al., 2012). The phenomenon of “unhappy doctors” has caused a breakdown in medical history not only in developed countries but in every part of the world (Edwards et al., 2002). Reformation in the healthcare system has undergone several changes due to economic constraints, more massive patient demands, higher workload among healthcare professionals especially doctors, and higher standards imposed in the provision of medical care (McManus et al., 2004; Siu et al., 2012). Besides, doctors also encountered several challenges such as the inability to communicate freely with patients, lack of ability to control over their work environment, physical exhaustion, excessive calls, shift duties and unhealthy sleep patterns (Schweitzer, 1994; Siu et al., 2012).
Health Status
The concept of health involves three domains, namely mental, physical and social (Huber et al., 2011; World Health Organization, 1948). However, several studies suggest that researchers should adopt a broader view by focusing on mental health and physical health as both categories are increasingly important at the workplace and in clinical settings (Danna & Griffin, 1999; Page & Vella-Brodrick, 2009). Mental health and physical health potentially affect both employees and organisations in adverse ways. Employees’ health at the workplace is crucial due to the fact the employees spend about one-third of their waking hours at work, and they usually would not leave their job behind even when they leave their work station (Conrad, 1988; Danna & Griffin, 1999). The overlap between work and non-work has become a common issue with the understanding that an employee’s work and personal life are no longer defined as separate entities but instead, they are interrelated and interconnected areas. Hence, work-related stress combined with non-work-related stress lead to detrimental physical and mental problems (Danna & Griffin, 1999). Danna and Griffin (1999) further stated that health status comprises a combination of mental (psychological) indicators such as frustration, anxiety and physical (physiological) indicators such as blood pressure, a heart condition, and general physical health. In the healthcare context, promoting good health among medical doctors is essential to improve their well-being status which ultimately increases their productivity, reduces absenteeism as well as in the aggregate, increases the health providers’ success (Benedict & Arterburn, 2008; Swift et al., 2014). Hence, health promotion in the workplace is necessary for medical doctors (Makrides et al., 2007; Swift et al., 2014). From the preceding discussion, this paper will focus on mental health and physical health.
Predictors of Health Status
There are several antecedents of health status (mental health and physical health) based on the previous literature. The following subsection will discuss the predictors.
Emotional Dissonance
Emotional dissonance refers to a situation where an employee is required to express emotions which are not genuinely felt in a particular case. Emotional dissonance is considered as a personal conflict where an individual response towards conflict with role expectations of desired emotions (Hochschild, 1983; Kahn et al., 1964). Emotional dissonance occurs when expressed emotions clash with true feelings (Abraham, 1998; Rafaeli & Sutton, 1987). Others considered emotional dissonance as a job demand specifically as an emotional regulation problem (Zapf, 2002; Zapf et al., 1999).
Giardini and Frese (2006) and Zapf et al. (1999) defined emotional dissonance as a stressor that may harm an employee’s effort to fulfil their task and it can become a threat to the employee’s well-being specifically to their mental as well as physical health. Expressing appropriate emotions at work is a part of job demand even when the employee is in a good or bad mood.
For instance, emotional dissonance is involved when medical doctors have to play their role in caring for their patients even though those emotions fail to mirror their true feelings. The inability of the employees to express their true feelings is manifested in the form of dissatisfaction towards the job, burnout and lower organisational commitment (Abraham, 2000). Moreover, healthcare professionals which include medical doctors, nurses and social workers that have direct interactions with patients have a higher risk of experiencing emotional dissonance that could jeopardise their mental as well as physical health (Bayram et al., 2012; Leiter, 1991; Schaubroeck & Jones, 2000).
Job Burnout
Job burnout is a psychological state resulting from prolonged emotional or mental stress on the job (Maslach & Jackson, 1981; Maslach et al., 2001). Job burnout has three dimensions comprising emotional exhaustion, depersonalisation and reduced personal accomplishment. Emotional exhaustion refers to feelings of being emotionally exhausted because of the work. Meanwhile, depersonalisation is an attempt to put distance between oneself and service recipients by actively ignoring the qualities that make them unique and engaging people (Maslach & Jackson, 1981; Maslach et al., 2001). Lastly, reduced personal accomplishment described a feeling of reduced competence and a lack of success or achievement in one’s work with people.
The occurrence of job burnout among various professions such as medical doctors, nurses, policeman, teachers, social workers, mental health workers and psychologists can arise from job-related factors and lack of a conducive workplace (Constable & Russell, 1986; Maslach & Jackson, 1981, 1984). Till today, job burnout among healthcare professionals has been recognized as a severe phenomenon in several cultures and developed countries since such occupations are interpersonally stressful and emotionally demanding (Alexandra-Karamanova et al., 2016; Bakker & Heuven, 2006; Lloyd et al., 2002; Ogundipe et al., 2014). This may result in mental disorders such as alcohol abuse, anxiety, depression, posttraumatic stress disorder, and even suicidal attempts. Also, job burnout may have serious psychosomatic consequences including headaches, hypertension, cardiopulmonary diseases, musculoskeletal disorders, gastritis, stomach ulcers, insomnia and dizziness (Arrogante & Zaldivar, 2017; Constable & Russell, 1986; Maslach et al., 2001). The effect of job burnout may also indirectly affect the individual’s work outcomes such as more significant number of medical errors, reduced quality of care, and lower patient satisfaction (Arrogante & Zaldivar, 2017).
Propositions
The study will propose four (4) propositions based on the previous literature. In reviewing the previous literature, the following subsection will discuss the propositions.
Emotional Dissonance and Health (mental health and physical health)
There is growing empirical support for the claim that emotional dissonance is associated with work strain, such as psychological distress and somatic complaints (Cheung & Tang, 2010). The results gathered from this study is in line with previous studies, all of which, showed that a high level of emotional dissonance is typically related to physical and psychological ill-health (Bakker & Heuven, 2006; Lewig & Dollard, 2003; Zapf et al., 1999). Thus, higher emotional dissonance is associated with reduced work motivation and lower well-being of employees (Wegge & Dick, 2010). This state of affairs could lead to employees’ turnover and absenteeism (Lewig & Dollard, 2003).
Human service professions have been identified as having greater risks of experiencing both mental health and physical health problems (Johnson et al., 2005). For instance, healthcare professionals dealing with dying and chronic patients every day and they were overloaded emotionally. The difficulties appear when the employees unable to express their genuine emotions and trigger them to hide their feelings. This situation may eventually lead to negative consequences to the employees, especially to their health status, such as mental health problems such as anxiety and depression (Mann & Cowburn, 2005). Previous studies have found that approximately employees unable to manage their emotions adequately at work as they regularly interacting with clients and in recent years the syndrome of job burnout appeared in response to their emotional attachment towards the clients (Johnson et al., 2005; Mann & Cowburn, 2005; Schaible & Gecas, 2010; Sonnentag et al., 2010). In short, employees frequently express their emotions in the workplace and such expressions are typically genuine and may also induce stress among them that could indirectly lower their health productivity or job performance such as job satisfaction and increase their intentions to quit (Cote & Morgan, 2002). Based on the discussion mentioned above, it can be posited that:
Emotional Dissonance and Job Burnout
There is growing support for the claim that emotional dissonance can be stressful, leading to job burnout. A study conducted among nurses and healthcare workers from a general hospital indicated that emotional dissonance was positively related to job burnout (Andela et al., 2016). Specifically, the results suggested that the existence of a strong correlation between emotional dissonance and job burnout. Besides, another study among healthcare workers in large hospitals in Netherland found that emotional dissonance was significantly and positively related to burnout dimensions of emotional exhaustion and cynicism (Bakker & Heuven, 2006). The results yielded by this study provided strong evidence that healthcare workers dealing with patients experience a discrepancy between genuine and displayed emotions, which in turn, lead to emotional exhaustion and depersonalization that may deplete their energy and ruin their work performance (Lewig & Dollard, 2003). Generally, service employees cannot express their authentic feelings during a service transaction. If they do, they might be at risk of acting unprofessionally and create discomfort for their clients. For instance, even though service employees are feeling tired due to working long hours, they have to continue smiling and being empathic all the time. There is growing support for the claim that when employees feel fatigued faking their genuine emotions, they may feel emotionally and physically drained and unable to display necessary emotions when interacting with clients. Hence, our second proposition is as follows:
Job Burnout Influencing Health Status (mental health and physical health)
In a recent study by Bianchi et al. (2018), job burnout was found to be positively related to depressive symptoms, and the correlation was found is strong (r=0.82). Besides, empirical evidence shows that burnout is strongly associated with mental health and physical health (Melamed et al., 2016). A study conducted by Arrogante and Zaldivar (2017) indicates that there is a negative relationship between job burnout and mental health. Their results showed that job burnout was negatively associated with mental health. The analysis showed that emotional exhaustion and depersonalization were negatively related to mental health, while reduced personal accomplishment was positively related to mental health. Mental health problems lead to depression, where the individual is likely to experience feelings of helplessness, hopelessness, and meaninglessness (Schaufeli & Buunk, 1996). On a similar note, emotional exhaustion was found to be negatively associated with physical health (Arrogante & Zaldivar, 2017). Therefore, based on the afore-mentioned empirical evidence, it can be surmised that job burnout will be negatively associated with mental health and physical health (Aasland et al., 1997; Felton, 1998). Hence, our third proposition is as follows:
The Role of Job Burnout as a Mediator in the Emotional Dissonance-Health Status Relationships
Human service professionals including doctors, are being described as having greater risks in experiencing mental health issues and physical health problems (Johnson et al., 2005). In the healthcare context, medical professionals such as doctors encounter dying and chronic patients every day. In such a risky situation, doctors would be unable to express their genuine emotions, which, in turn, make them become overloaded emotionally. As such, they become overloaded emotionally. This difficulty appears when employees unable to express their genuine emotions and trigger them to hide their feelings. This situation may eventually lead to negative consequences to employees’ health status, such as greater anxiety and higher depression (Mann & Cowburn, 2005). In recent years, the syndrome of job burnout appeared in response to their emotional attachment towards clients (Johnson et al., 2005; Mann & Cowburn, 2005; Schaible & Gecas, 2010; Sonnentag et al., 2010). Healthcare employees are more likely to experience higher burnout. This is more so when they have to take care of terminally sick patients including those who have cancer. Caring for these patients will make them feel responsible for their patients’ life. So, when patients die, these healthcare workers tend to feel sad, frustrated, anger, guilty, and shocked. Since they have to work, as usual, these employees tend to suppress their negative emotions, leading to burnout, which eventually has deleterious effects to their mind and body. As a result, it has been shown that emotional dissonance harms mental illnesses (Bowman, 2001) and physical complaints (Kovacs et al., 2010; Schaubroeck & Jones, 2000). As such, it is posited that:
Problem Statement
The Malaysian healthcare industry is affected by internal issues such as shortage of medical doctors and increasing number of patients seeking treatment at public hospitals, which ultimately, resulted in greater work burden for the medical doctors especially the housemen who have been known to experience high level of emotional pressure (Razak et al., 2011). Substantial evidence is indicating that medical doctors are at higher risks of experiencing stress, depression, anxiety, substance misuse, and addiction than the general population (Brooks et al., 2017). Doctors who suffer from these risks jeopardize not only their quality of life but also the quality of care that they provide to their patients. Furthermore, doctors who experience job burnout have a higher rate of depressive symptoms and suicide attempts and are often unable to meet the demands of patients (Wieclaw et al., 2008). Doctors are significantly crucial to the public, and thus their illnesses and sufferings may result in a delay in care delivery, which will have a spillover effect on their patients (Kay et al., 2004; Uncu et al., 2006). According to the Malaysian medical and health services, shortage of doctors in the public sector, and the increasing number of patients seeking treatment at government clinics and hospitals have resulted in greater work burden for doctors especially the junior ones (Rajaendram, 2017). It has been reported that junior doctors who worked under severe stress had sought psychiatric help (Free Malaysia Today, July 23, 2018). On average, one medical doctor working in a public hospital quit his/her job and move to a private hospital. This is especially rampant among specialists. For instance, at least 124 specialist doctors resigned in 2015 and 128 in 2016 (Awani, 2016).
On the basis of the evidence mentioned above, it seems reasonable to suggest that there is a need to enhance the quality of healthcare professionals, particularly medical doctors in the Malaysian public healthcare sector to provide quality services to patients. This is because patient care has always been considered as an important goal in healthcare, as suggested by Brickell and McLean (2011). Healthcare professionals, mainly medical doctors play a vital role in providing quality medical treatment to their patients according to their patients’ needs, wants and preference (Firth-Cozens, 2001).
Research Questions
The research questions of this study are as below:
Do emotional dissonance influence job burnout?
Do job burnout influence health status, mental health and physical health?
Does job burnout mediate the relationship between emotional dissonance and health status, mental health and physical health?
Purpose of the Study
The purpose of the study is to review the literature and subsequently propose a model linking emotional dissonance and health status (mental health and physical health) among medical doctors in Malaysian public hospitals.
Research Methods
This study is a cross-sectional study, with all variables and data gathered over a set period in order to answer the research questions. Data collection will be conducted at the public hospitals where the medical doctors’ normal working environment and with minimum interference from the researcher. In this study, all variables will be measured at an individual level. Data will be gathered from each individual in selected state hospitals.
Findings
Based on the preceding review of the literature and consistent effect of emotional dissonance on employee’s mental health and physical health, a model has been developed as depicted in Figure
Conclusion
Healthcare system in a country plays a vital role in the well-being of the nations, including society, organisations, and individual. Healthcare workers, particularly medical doctors, act as front-liners as they have direct contact with the patients. A medical doctor is someone who provides preventive, curative, promotion or rehabilitative healthcare services in a systematic way to individuals, families, or communities. They have exposed continuously many occupational stressors such as emotional dissonance, role conflict, role overload, and role ambiguity. Hence, medical doctors’ well-being is vital, which can influence directly to their job performance. In the workplace, faking genuine emotions particularly become personal conflict to employees as desired by role expectations. Professions that regularly interact with human service are being described as having greater risks experiencing health problems such as mental health issues and physical health complaints (Johnson et al., 2005). The difficulties appear when the employees unable to express their genuine emotions and trigger them to hide their feelings. This situation may eventually lead to negative consequences to the employees, especially to their health status, such as mental health problems typically anxiety and depression (Mann & Cowburn, 2005). Therefore, to prevent and reduce the impact of emotional dissonance on mental and physical well-being, there is a need for greater attention to variables explaining to what extent emotional dissonance is related to health status as well as to job burnout.
Acknowledgments
This paper is sponsored by the School of Management (SOM) Fund 2019.
References
- Aasland, O. G., Olff, M., Falkum, E., Schweder, T., & Ursin, H. (1997). Health complaints and job stress in Norwegian physicians: the use of an overlapping questionnaire design. Soc. Sci. Med., 45(11), 1615–1629.
- Abraham, R. (1998). Emotional dissonance in organizations: antecedents, consequences, and moderators. Genetic, Social, and General Psychology Monographs, 12(2), 229–246.
- Abraham, R. (2000). The role of job control as a moderator of emotional dissonance and emotional intelligence–outcome relationships. The Journal of Psychology, 134(2), 169–184.
- Alexandra-Karamanova, A., Todorova, I., Montgomery, A., Panagopoulou, E., Costa, P., Baban, A., … Mijakoski, D. (2016). Burnout and health behaviors in health professionals from seven European countries. Health Int Arch Occup Environ, 89, 1059–1075.
- Andela, M., Truchot, D., & Doef, D. M. A. (2016). Job stressors and burnout in hospitals: the mediating role of emotional dissonance. International Journal of Stress Management, 23(3), 298–317.
- Arrogante, O., & Zaldivar, E. A. (2017). Burnout and health among critical care professionals: The mediation role of resilience. Intensive and Critical Care Nursing, 42, 110–115.
- Awani, A. (2016). More than 120 medical specialists resign every year - Dr Hilmi.
- Bakker, A. B., & Heuven, E. (2006). Emotional dissonance, burnout and in-role performance among nurses and police officers. International Journal of Stress Management, 13(4), 423–440.
- Bayram, N., Aytac, S., & Dursun, S. (2012). Emotional labor and burnout at work: a study from Turkey. Procedia-Social and Behavioral Sciences, 65, 300-305.
- Benedict, M., & Arterburn, D. (2008). Worksite-based weight loss programs: a systematic review of recent literature. American Journal of Health Promotion, 22(6), 408–416.
- Bianchi, R., Mayor, E., Schonfeld, I. S., & Laurent, E. (2018). Burnout and depressive symptoms are not primarily linked to perceived organizational problems. Psychology, Health & Medicine, 1–12.
- Bowman, G. S. (2001). Emotions and illness. Journal of Advanced Nursing, 34(2), 256–263.
- Brickell, T. A., & McLean, C. (2011). Emerging issues and challenges for improving patient safety in mental health: a qualitative analysis of expert perspectives. Journal of Patient Safety, 7(1), 39–44.
- Brooks, S. K., Gerada, C., & Chalder, T. (2017). The specific needs of doctors with mental health problems: qualitative analysis of doctor-patients’ experiences with the Practitioner Health Programme. Journal of Mental Health, 26(2), 161–166.
- Cheung, F., & Tang, C. (2010). The influence of emotional dissonance on subjective health and job satisfaction: testing the stress-strain-outcome model. Journal of Applied Social Psychology, 40(12), 3192–3217.
- Conrad, P. (1988). Health and fitness at work: a participants’ perspective. Social Science Medicine, 26, 545–550.
- Constable, J. F., & Russell, D. W. (1986). The effect of social support and the work environment upon burnout among nurses. Journal of Human Stress, 12(1), 20–26.
- Cote, S., & Morgan, L. M. (2002). A longitudinal analysis of the association between emotion regulation, job satisfaction and intentions to quit. Journal of Organizational Behavior, 23(8), 947–963.
- Danna, K., & Griffin, R. W. (1999). Health and well-being in the workplace: a review and synthesis of the literature. Journal of Management, 25(3), 35–384.
- Edwards, N., Kornacki, M. J., & Silevrsin, J. (2002). Unhappy doctors: what are the causes and what can be done? BMJ, 324, 835–838.
- Felton, J. S. (1998). Burnout as a clinical entity- its importance in health care workers. Occup. Med., 48(4), 237–250.
- Firth-Cozens, J. (2001). Interventions to improve physicians’ well-being and patient care. Social Science and Medicine, 52(2), 215–222.
- Giardini, A., & Frese, M. (2006). Reducing the negative effects of emotion work in service occupation: emotional competence as a psychological resource. Journal of Occupational Health Psychology, 11(1), 63–75.
- Hochschild, A. R. (1983). The managed heart. In Practice: contemporary issues through the lenses. University of California Press.
- Huber, M., Knottnerus, J. A., Green, L., & van der Horst, H. (2011). How should we define health? BMJ, 343, d4163.
- Johnson, S., Cooper, C., Cartwright, S., Donald, I., Taylor, P., & Millet, C. (2005). The experience of work-related stress across occupations. Journal of Managerial Psychology, 20(2), 178–187.
- Kahn, R. L., Wolfe, D. M., Quinn, R. P., Snoek, J. D., & Rosenthal, R. A. (1964). Organizational stress: studies in role conflict and ambiguity. John Wiley.
- Kay, M. P., Mitchell, G. K., & Del Mar, C. B. (2004). Doctors do not adequately look after their own physical health. Medical Journal of Australia, 181(7), 368.
- Kovacs, M., Kovacs, E., & Hegedus, K. (2010). Is emotional dissonance more prevalent in oncology care? Emotion work, burnout and coping. Psycho-Oncology, 19, 855–862.
- Leiter, M. P. (1991). Coping patterns as predictors of burnout: the function of control and coping patterns. Journal of Organizational Behaviour, 12, 123–144.
- Lewig, K. A., & Dollard, M. F. (2003). Emotional dissonance, emotional exhaustion and job satisfaction in call centre workers. European Journal of Work and Organizational Psychology, 12(4), 366–392.
- Lloyd, C., King, R., Chenoweth, L., Llyod, C., King, R., Chenoweth, L., … Chenoweth, L. (2002). Social work, stress and burnout: a review. Journal of Mental Health, 11(3), 255–265.
- Makrides, L., Heath, S., Farquharson, J., & Veinot, P. (2007). Perceptions of workplace health: building community partnership. Clinical Governance: An International Journal, 123, 178–187.
- Mann, S., & Cowburn, J. (2005). Emotional labour and stress within mental health nursing. Journal of Psychiatric and Mental Health, 12, 154–162.
- Maslach, C., & Jackson, S. E. (1981). The measurement of experienced burnout. Journal of Occupational Behavior, 2, 99–113.
- Maslach, C., & Jackson, S. E. (1984). Burnout in organizational settings. Journal of Occupational Behaviour, 2, 99–113.
- Maslach, C., Schaufeli, W. B., & Leiter, M. P. (2001). Job burnout. Annual Review of Psychology, 52(1), 397–422. https://doi.org/10.1146/annurev.psych.52.1.397
- McManus, I. C., Keeling, A., & Paice, E. (2004). Stress, burnout and doctors’ attitudes to work are determined by personality and learning style: a twelve year longitudinal study of medical graduates. BMC Medicine, 2(29), 1–12.
- Melamed, S., Shirom, A., Toker, S., Berliner, S., & Shapira, I. (2016). Burnout and risk of cardiovascular disease: evidence, possible casual paths and promising research directions. Psychological Bulletin, 132(3), 327–353.
- Ogundipe, O. A., Olagunju, A. T., Lasebikan, V. O., & Coker, A. O. (2014). Burnout among doctors in residency training in a tertiary hospital. Asian Journal of Psychiatry, 10, 27–32.
- Page, K. M., & Vella-Brodrick, D. A. (2009). The ’ What’, “Why” and “How” of employee well-being: a new model. Soc Indic Res, 90, 441–458.
- Rafaeli, A., & Sutton, R. (1987). Expression of emotion as part of the work role. Academy of Management Review, 12, 23–37.
- Rajaendram, R. (2017, August 20). Headache over lack of specialised medical practitioners. New Strait TimesStrait Times. https://www.thestar.com.my/news/education/2017/08/20/headache-over-lack-of-specialised-medical-practitioners/
- Razak, A. Z. A., Yunus, N. K. Y., & Nasurdin, A. M. (2011). The impact of work overload and job involvement on work-family conflict among Malaysian doctors. Labuan E-Journal of Muamalat and Society, 5, 1–10.
- Schaible, L. M., & Gecas, V. (2010). The impact of emotional labor and value dissonance on burnout among police officers. Police Quarterly, 13(3), 316–341.
- Schaubroeck, J., & Jones, J. R. (2000). Antecedents of workplace emotional labor dimensions and moderators of their effects on physical symptoms. Journal of Organizational Behavior, 21, 163–183.
- Schaufeli, W. B., & Buunk, B. P. (1996). Professional burnout. In Handbook of Work and Health Psychology (pp. 311–346). John Wiley & Sons Ltd.
- Schweitzer, S. (1994). Stress and burnout in junior doctors. S Afr Med J, 84, 352–354.
- Siu, C., Yuen, S. K., & Cheung, A. (2012). Burnout among public doctors in Hong Kong: cross sectional survey. Hong Kong Med J, 18(3), 185–194.
- Sonnentag, S., Kuttler, I., & Fritz, C. (2010). Job stressors, emotional exhaustion and need for recovery: a multi-score study on the benefits of psychological detachment. Journal of Vocational Behavior, 76(3), 355–365.
- Swift, V. D., Christopher, F., Marshall, K., Welch, N., & Wilis, J. (2014). What really improves employee health and wellbeing Findings from regional Australian workplaces. International Journal of Workplace Health Management, 7(3), 138–155.
- Today, F. M. (2018). Why junior doctors won’t report bullying. Free Malaysia Today.
- Uncu, Y., Bayram, N., & Bilgel, N. (2006). Job related affective well-being among primary health care physicians. European Journal of Public Health, 17(5), 514–519.
- Wegge, J., & Dick, R. V. (2010). Emotional dissonance in call centre work. Journal of Managerial Psychology, 25(6), 596-619. https://doi.org/10.1108/02683941011056950
- Wieclaw, J., Agerbo, E., Mortensen, P. B., Burr, H., Tuchsen, F., & Bonde, J. P. (2008). Psychosocial working conditions and the risk of depression and anxiety disorders in the Danish workforce. BMC Public Health, 8(1), 280.
- World Health Organization. (1948). Constitution of the World Health Organization. WHO.
- Zapf, D. (2002). Emotion work and psychological well-being: a review of the literature and some conceptual considerations. Human Resource Management Review, 12, 237–268.
- Zapf, D., Vogt, C., Seifert, C., Mertini, H., & Isic, A. (1999). Emotion work as a source of stress: the concept and development of an instrument. European Journal of Work and Organizational Psychology, 8(3), 371–400.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
06 October 2020
Article Doi
eBook ISBN
978-1-80296-087-7
Publisher
European Publisher
Volume
88
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-1099
Subjects
Finance, business, innovation, entrepreneurship, sustainability, environment, green business, environmental issues
Cite this article as:
Omar, N. F., & Mohd Nasurdin, A. (2020). The Effect Of Emotional Dissonance On Mental And Physical Well-Being Among Healthcare Professionals. In Z. Ahmad (Ed.), Progressing Beyond and Better: Leading Businesses for a Sustainable Future, vol 88. European Proceedings of Social and Behavioural Sciences (pp. 1078-1087). European Publisher. https://doi.org/10.15405/epsbs.2020.10.101
