Abstract
Anesthesiologists-resuscitators, performing their professional duties in stressful, and often extreme activity conditions (with a risk to life and health), can be classified as a risk group for various negative mental states. Anesthesiologists-resuscitators’ professional activity makes significant demands on their personality. The purpose is to identify and describe the characteristics of anesthesiologists-resuscitators mental states in extreme activity conditions. Methods. 49 anesthesiologists-resuscitators of the Arkhangelsk region (Russia) were examined. Methods were used: questionnaires, psychological testing -the organizational stress scale, the dominant status measurement, the multilevel personal questionnaire "Adaptability", the questionnaire "Attitude to work and professional burn-out", the Lüscher colour test, the Russian form of the state-trait-anxiety inventory and the statistical processing of the empirical results. It was found that in the performing professional duties course, more than 79.6 % of anesthesiologists-resuscitators often face stressful situations; every third person is exposed to a threat to life or the injury risk, injury in the work process. More than half of the respondents have a high organizational stress level, 67.3 % have a professional burnout syndrome, 35.3 % are characterized by fatigue, concentration lack, lethargy, inertia, low performance, and 1 / 3 have a high situational anxiety indicator. Every second anesthesiologist-resuscitator has an adaptiveabilities reduced level, 14.2 % – expressed asthenic, and 24.4 % – psychotic reactions and conditions. Recommendations for the negative mental states prevention in anesthesiologists-resuscitators were made in several areas: professional & organizational, social, individual psychological.
Keywords: Anesthesiologists-resuscitatorsmental statesorganizational stressextreme conditions of activity
Introduction
Currently, much attention is paid to professional health studying of specialists working in increased emotional and physical stress conditions, responsibility, risk to life and health (Karamova et al., 2017; Shchelkova, 2007; Taskina, 2020). The anesthesiologists-resuscitators’ work in stressful, and often extreme activity conditions, makes increased demands on specialist’s personality, his professional qualities and emotional stability (Ironosov et al., 2019). Anesthesiologists-resuscitators’ features professional activity are the maintenance and vital functions restoration of the body in life-threatening conditions, the need to maintain calm in emergency situations, rapid decision-making, the daily schedule intensity, work in uncertainty and overload conditions, the exceptional patients’ severity (Gurman et al., 2012; Korehova et al., 2019; Mamas & Kosarevskaya, 2010).
Problem Statement
The anesthesiologists-resuscitators work is similar to the air traffic controllers activity and airliner pilots in terms of the information load intensity, since the only correct solution choice is limited by a strict time frame (Shvetsky et al., 2016). Night shifts have a significant negative impact on the neuropsychological state of doctors, which is manifested in a decrease in mental stability, the workability and efficiency in work degree (Netesin & Gorbachev, 2018).
Anesthesiologists-resuscitators, performing their professional duties in stressful and extreme activity conditions, can be classified as a risk group for various negative mental states, the professional burnout syndrome (PBS) development and mental maladaptation, which in turn can affect the specialist’s personality, his health, the effectiveness and his professional activities quality, relationships with colleagues, patients and relatives.
PBS signs occur in 25-60 % of anesthesiologists (Mamas & Kosarevskaya, 2010; Parfenov, 2012). High PBS rates were found in both young professionals under of 30 y. o. and doctors with long work experience (Netyosin et al., 2017; Nyssen et al., 2003; Sanfilippo et al., 2018; Vasilieva & Grigoriev, 2017). The distress prevalence among anesthesiologists-resuscitators is 17-37 %, and depression is 9-15 % (Sun et al., 2019). Almost every second specialist in the anesthesiology departments and intensive care thought about suicide (Ohtonen & Alahuhta, 2017; Sinbukhova et al., 2019).
Research Questions
Anesthesiologists-resuscitators have to perform their professional duties in difficult, and often in extreme activity conditions. As a result, they are highly likely to develop negative mental states, including maladaptive ones. The main research questions were: What mental states are found among anesthesiologists-resuscitators who carry out their professional activities in extreme conditions?
How often are marked by various non-adaptive condition have doctors anesthesiologists-resuscitators? What are anesthesiologists-resuscitators mental states in extreme activity conditions?
Purpose of the Study
At the moment, there are quite a large works number on the professional stress problem and PBS of various medical specialties. However, the anesthesiologists-resuscitators’ mental states issues in extreme activity conditions have not yet been studied enough and require clarification. The purpose is to identify and describe the anesthesiologists-resuscitators’ mental states in extreme activity conditions.
Research Methods
49 anesthesiologists-resuscitators of the Arkhangelsk region took part in the study; average age is 34.6 ± 13.6 y. o. (M ± SD), among them 32.6 % are female and 67.4% are male. Methods used: psychological testing, questionnaires and statistical processing of empirical results. The McLean’s (1979) organizational stress scale, adapted by Vodopyanova (2009) was used to assess an organizational stress severity. With the Vinokur’s questionnaire (Vinokur & Klitcenko, 2012) "Attitude to work and professional burn-out" (the Russian global cycling project) was estimated by the formation of PBS. The Maklakov - Chermyanin’s multi-level personal questionnaire "Adaptability" (MPQ-A) was used to determine the adaptive individual abilities, as well as asthenic and psychotic states (Maklakov & Chermyanin, 1993, as cited in Raigorodskii, 2001). The Hanin – Spielberger’s (1983) questionnaire was used to assess measures of anxiety, the Lüscher color test – to study the current state of a person; the coefficient of vegetative tone and deviation from the autogenic norm were calculated. The Kulikov’s (2003) method for determining the dominant state was used to diagnose relatively stable conditions using subjective subject assessments. The results were processed using the SPSS Statistics application software package (version 23.00, license Z125-5301-14). The U-Mann-Whitney test was used to evaluate the differences between two independent samples based on the trait level. Pearson's χ2 criterion was used to analyze differences in the trait occurrence frequency.
Findings
Research results
According to the survey results, 79.6 % of anesthesiologists-resuscitators considered their work to be stressful factors full that they have to face almost daily, 28.6% – faced a threat to life in the performing professional duties course, 40.8 % – with threats, insults and intimidation, 14.3 % – received bruises and minor injuries, 20.4 % - often experienced a anxiety state in the activities course, and 26.5 % – a decrease in performance. 53.3 % of the subjects had a high organizational stress level according to the McLin’s scale, i. e. they had a low tolerance to the stress factors action of stress dotors arising at work and a high predisposition to professional stress.
The average integrative PBS index according to the Vinokur's method in anesthesiologists-resuscitators corresponded to high values (49.4 ± 9.4). In 67.3 %, formed PBS was detected, characterized by severe physical, mental and emotional exhaustion, a decrease in self-esteem of the work quality and its significance, and the health problems appearance.
In 46.9 %, using the MPQ-A method, a reduced adaptive abilities level was detected, while only 4.1 % – had good adaptive abilities. 14.2 % of the subjects were characterized by asthenic reactions and adaptive abilities high situational anxiety states, hypochondriacal fixation, increased fatigue and weakness. In 24.4 %, reactions and conditions indicating the impulsive reactions presence, aggressiveness and, in general, expressed neuro-psychic tension were detected.
According to the Hanin-Spielberger’s (1983) method, 30.0 % of anesthesiologists-resuscitators had a high situational anxiety level, characterized by increased nervousness and anxiety.
The dominance of trophotropic tendencies according to the Lusher’s method was revealed in 55.9 % of the subjects.
The total deviation from the autogenic norm was 15.6 ± 6.2, which indicates good performance reserves, but with a tendency to accumulate fatigue, which is not so easy to get rid of and can only be overcome by significant willpower. In 14.7 % of anesthesiologists-resuscitators, the general emotional background was characterized by increased excitability, anxiety, uncertainty, and a high nervous breakdown probability. Increased fatigue, sharp mood swings, and powerlessness feelings were observed in 5.9 %.
According to the Kulikov’s (2003) method of determining the dominant state, 35.3 % of doctors were characterized by fatigue, concentration lack, lethargy, inertia, low efficiency, 29.4 % – a passive and pessimistic attitude to life, 17.6 % – a reduced mood, a gloom sense and frustration, 11.6 % – reduced emotional stability.
For a more detailed analysis, all subjects were divided into two groups, depending on the maladaptive states signs presence:
Group 1 (18 people, 36.7 %) – anesthesiologists-resuscitators who have maladaptive conditions signs (formed PBS level, asthenic presence and psychotic conditions, maladaptation signs).
Group 2 (31 people, 63.3 %) – anesthesiologists-resuscitators who have no maladaptation conditions signs.
According to the survey results, 11.1 % of the subjects in Group 1 and 32.2 % in Group 2 believed that they were more likely to be in a good mood. A greater Group 1 number (44.4 %) compared to Group 2 (16.1 %) (p ≤ 0.05) noted a decrease in their performance. Also, Group 1 anesthesiologists-resuscitators were more likely to have health complaints (63.2 %) compared to group 2 (29.0 %) (p ≤ 0.01).
Results analysis using the MPQ-A method showed that Group 1anesthesiologists-resuscitators had lower adaptive potential personal indicators (68.6 ± 13.1), compared with Group 2 (38.4 ± 13.8) (p ≤ 0.001), that is, Group 1 doctors are more difficult to cope with difficult situations and they are more likely to have neuropsychiatric breakdowns.
Compared to Group 2, the Group 1 subjects had lower behavioral regulation indicators (p ≤ 0.001), communication potential (p ≤ 0.001), and moral normativity (p ≤ 0.01) (Figure
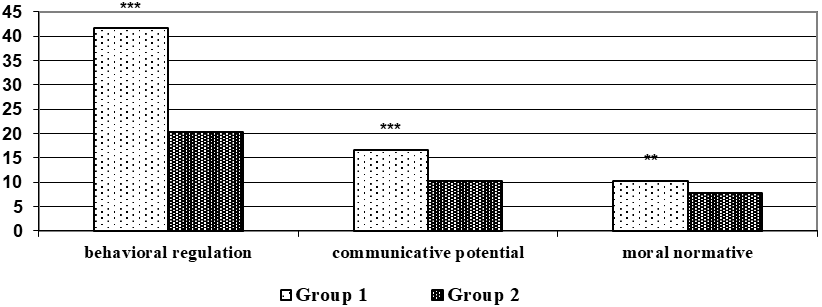
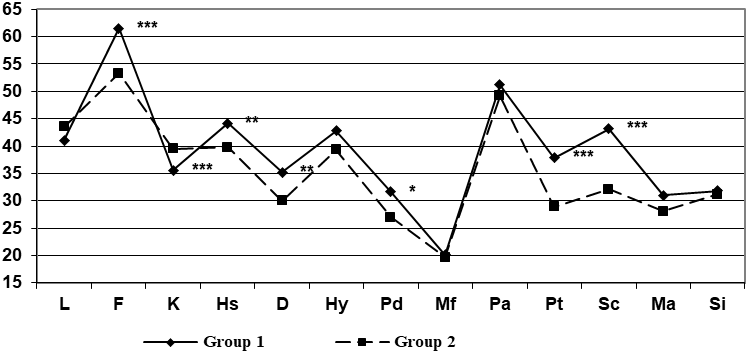
Group 1 doctors were characterized by greater social passivity, slower adaptation to changes in professional activity, a tendency to a reduced mood background, self-doubt, anxiety, volitional control weakening, impulsivity and conflict, in comparison with Group 2 (Figure
The total deviation from the autogenic norm was significantly higher in Group 1 (19.4 ± 6.6) compared to Group 2 (12.9 ± 4.3) (p ≤ 0.01), which indicates that the Group 2 anesthesiologists-resuscitators had more additional performance reserves and resistance to stress.
The Group 1 subjects had higher situational indicators (49.7 ± 4.9) and personal anxiety (55.0 ± 6.0) compared to Group 2 (33.4 ± 9.3, 41.9 ± 8.2, respectively) (p ≤ 0.05), that is, Group 1 anesthesiologists-resuscitators were more prone to anxiety, tension and excessive experiences.
According to the Kulikov’s (2003) method (Table
Results discussion
According to their own opinion, the anesthesiologists-resuscitators activity was many stressful factors full. 1/3 faced extreme factors at work, related to the risk to life and health. More than half of the anesthesiologists-resuscitators had a low tolerance to organizational stress, a reduced adaptive abilities level, characterized by difficulties in adaptation, low neuropsychological stability and a high functional disorders probability. Almost 2 / 3 were found to have formed PBS. Our results indicate a higher PBS incidence among anesthesiologists-resuscitators than according to other researchers (Parfenov, 2012; Sanfilippo et al., 2018).
The need for rest, the desire to spend less energy was identified in more than half of the anesthesiologists-resuscitators; 1 / 3 were characterized by low performance, passive and pessimistic attitude to life. Increased fatigue, sharp mood swings, and a powerlessness sense were observed in 5.9 %. 36.7 % showed maladaptive states signs, the formed PBS level, the asthenic presence and psychotic states, and maladaptation signs. Anesthesiologists-resuscitators who have maladaptive conditions signs, more often noted a decrease in performance and complaints about their health status compared to those who did not have these signs.
Anesthesiologists-resuscitators with maladaptive states signs were characterized by difficulties in self-regulation, building contacts with colleagues and patients, increased conflict and reduced behavior normativity. They were characterized by greater social passivity, slower adaptation to changes in professional activity, a tendency to a reduced mood background, self-doubt, anxiety, and a volitional control weakening.
Doctors who had no maladaptive states signs had a satisfactory adaptive abilities level neuropsychiatric stability, adequate self-esteem, well-developed communication abilities, a high socialization level, and additional performance reserves and resistance to stress. They are more active, sociable, optimistic, resistant to physical and mental stress, more confident, able to make decisions independently, without unnecessary doubts about its correctness.
The results obtained should be taken into account when organizing preventive measures to reduce the developing maladaptive conditions likelihood in anesthesiologists-resuscitators. Preventive measures should be carried out in several directions at once: professional & organizational, social, individual psychological. Professional & organizational direction should be focused on reducing organizational stress, rationalizing the work and rest regime, providing, if necessary, additional paid vacations, necessary, modern and ergonomic workplace equipment, a room presence for psychological unloading. The social direction, first of all, includes measures aimed at diagnosing the social climate in the team, developing communication skills and the ability to resolve difficult situations without conflict. Individual psychological direction of prevention: individual and personal diagnostics; measures aimed at developing self-confidence and forming an adequate self-esteem; skills development to recognize and manage their emotions; training in self-regulation skills.
Conclusion
The anesthesiologists-resuscitators activity takes place in severe, extreme conditions. Every third specialist faces a threat to life in the performing professional duties course. More than half of anesthesiologists-resuscitators have a low tolerance to organizational stress and a reduced adaptive abilities level. 1/3 is characterized by fatigue, concentration lack, low performance, passive and pessimistic attitude to life. Increased fatigue, sharp mood swings, and powerlessness feelings are observed in 5.9 % of doctors.
36.7 % of anesthesiologists-resuscitators have maladaptive states signs, the formed PBS level, the asthenic presence and psychotic states, maladaptation signs. They are characterized by social passivity, a tendency to a reduced mood background, difficulties in self-regulation, conflict, self-doubt, anxiety and reduced behavior normativity. The results obtained should be taken into account when organizing preventive measures to reduce the developing maladaptive conditions likelihood in anesthesiologists-resuscitators. Preventive measures should be carried out in several directions at once: professional & organizational, social, individual psychological.
Acknowledgments
References
- Gurman, G. M., Klein, M., & Weksler, N. (2012). Professional stress in anesthesiology: a review. Journal of Clinical Monitoring and Computing, 26(4), 329-335. https://doi.org/10.1007/s10877-011-9328-7
- Hanin, Y. L., & Spielberger, C. D. (1983). The development and validation of the Russian Form of the State-Trait Anxiety Inventory. Series in Clinical & Community Psychology: Stress & Anxiety, 2, 15–26.
- Ironosov, V. E., Lytayev, S. A., & Gordeev, V. I. (2019). Uroven' emotsional'noy i stressornoy ustoychivosti vrachey anesteziologov-reanimatologov [Level of emotional and stress resistance of resuscitation anesthetists]. Medicine: Theory and Practice, 4(5), 230-231. https://elibrary.ru/item.asp?id=39199129
- Karamova, L. M., Krasovsky, V. O., Akhmetshina, V. T., Khafizova, A. S., Vlasova, N. V., Bulyakov, R. M., Nafikov, R. G. (2017). Professional'nyy risk zdorov'ya meditsinskikh rabotnikov stantsii skoroy meditsinskoy pomoshchi [Occupational health risk for medical personnel at ambulance stations]. Occupational Medicine and Human Ecology, 4(12), 28-36. https://cyberleninka.ru/article/n/professionalnyi-risk-zdorovya-meditsinskih-rabotnikov-stantsii-skoroi-meditsinskoi-pomoschi
- Korehova, М. V., Soloviev, A. G., Kirov, M. Y., & Novikova, I. A. (2019). Comparative regional peculiarities of the professional burnout syndrome in doctors of anaesthesiologists-reanimatologists. V.M. Bekhterev Reviev of Psychiatry and Medical Psychology, 2, 84–94. https://doi.org/10.31363/2313-7053-2019-2-84-94
- Kulikov, L. V. (2003). Rukovodstvo k metodikam diagnostiki psikhicheskikh sostoi͡aniĭ, chuvstv i psikhologicheskoĭ ustoĭchivosti lichnosti. Opisanie metodik, instrukt͡sii po primenenii͡u [Guide to methods for diagnosing mental states, feelings, and psychological stability of the individual. Description of methods and instructions for use]. Saint-Petersburg.
- Mamas, A. N., & Kosarevskaya, T. A. (2010). Issledovaniye sindroma emotsional'nogo vygoraniya u vrachey anesteziologov-reanimatologov [Study of burnout syndrome in anesthetist-resuscitation doctors]. Surgery News, 18(6), 75-81. https://elibrary.ru/item.asp?id=17818825
- McLean, A. A. (1979). Work stress. Addison-Wesley.
- Netesin, E. S., & Gorbachev, V. I. (2018). Otsenka ustoychivosti vnimaniya i dinamika rabotosposobnosti vrachey anesteziologov-reanimatologov [Assessment of attention sustainability and performance dynamics of resuscitation anesthetists]. Occupational Medicine and Industrial Ecology, 4, 24-28. https://elibrary.ru/item.asp?id=32834691
- Netyosin, E. S., Gorbachev, V. I., Nelyubin, A. G., & Mitkinov, O. E. (2017). Professional'noye vygoraniye u vrachey anesteziologov-reanimatologov [Professional burnout by resuscitation anesthetists]. Acta Biomedica Scientifica, 1(113), 7478. https://elibrary.ru/item.asp?id=28856202
- Nyssen, A. S., Hansez, I., Baele, P., Lamy, M., & De Keyser, V. (2003). Occupational stress and burnout in anaesthesia. British Journal of Anaesthesia, 90(3), 333–337. https://doi.org/10.1093/bja/aeg058
- Ohtonen, P., & Alahuhta, S. (2017). Mortality rates for Finnish anaesthesiologists and paediatricians are lower than those for the general population. Acta Anaesthesiologica Scandinavica, 61(8), 880–884. https://doi.org/10.1111/aas.12936
- Parfenov, Y. A. (2012). Patogeneticheskiye determinanty psikhosomaticheskikh rasstroystv pri arterial'noy gipertenzii u vrachey-anesteziologov s sindromom professional'nogo vygoraniya [Pathogenetic determinants of psychosomatic disorders in arterial hypertension in anesthetists with burnout syndrome]. Basic Research, 5(2), 325329. https://elibrary.ru/item.asp?id=17867953
- Raigorodskii, D. Y. (2001). Mnogourovnevyĭ lichnostnyĭ oprosnik “Adaptivnostʹ” (MLO-AM) A.G.Maklakova i S.V.CHermi͡anina [Multilevel personal questionnaire “Adaptability" (MPQ AM) by A. G. Maklakov and S.V. Chermyanin]. In D. Y. Raigorodskii (Ed.). Prakticheskai͡a psikhodiagnostika: Metodiki i testy [Practical psychodiagnostics: Methods and tests] (pp. 549-558). Bahrah-M.
- Sanfilippo, F., Noto, A., Palumbo, G. J., Ippolito, M., Gagliardone, M., Scarlata, M., Bignami, E., Sangalli, F., Cattaneo, S., Blangetti, I. Scolletta, S., Locatelli, A., Tritapepe, L., Lorini, F. L., Arcadipane, A. (2018). Burnout in Cardiac Anesthesiologists: Results From a National Survey in Italy. Journal of Cardiothoracic and Vascular Anesthesia, 32(6), 2459-2466. https://doi.org/10.1053/j.jvca.2018.05.016
- Shchelkova, O. Y. (2007). Psikhodiagnostika v sistemnom issledovanii emotsional'no-lichnostnoy sfery vrachey anesteziologov-reanimatologov (v svyazi so stressogennym kharakterom professional'noy deyatel'nosti) [Psychodiagnostics in a systematic study of the emotional and personal sphere of anesthesiologists-resuscitation doctors (due to the stressful nature of professional activity)]. Siberian Psychological Journal, 6, 154160. https://cyberleninka.ru/article/n/psihodiagnostika-v-sistemnom-issledovanii-emotsionalno-lichnostnoy-sfery-vrachey-anesteziologov-reanimatologov-v-svyazi-so
- Shvetsky, F. M., Potievskaya, V. I., Smolnikov, P. V., & Chizhov, A. Y. (2016). Korrektsiya funktsional'nogo sostoyaniya vrachey anesteziologov-reanimatologov ingalyatsiyami ksenona [Correction of the functional state of resuscitation anesthetists by xenon inhalation]. Bulletin of the Peoples' Friendship University of Russia. Series: Ecology and Life Safety, 4, 96-114. https://elibrary.ru/item.asp?id=27310662
- Sinbukhova, E. V., Petrikov, S. S., Shabanov, A. K., Plotnikov, G. P., Lubnin, A. Y., & Sinbukhova, N. I. (2019). Open Questions of Life Satisfaction and Burnout in Anesthesiology and Resuscitation. Russian Sklifosovsky Journal “Emergency Medical Care”, 8(3), 266–273. https://doi.org/10.23934/2223-9022-2019-8-3-266-273.
- Sun, H., Warner, D. O., Macario, A., Zhou, Y., Culley, D. J., & Keegan, M. T. (2019). Repeated Cross-sectional Surveys of Burnout, Distress, and Depression among Anesthesiology Residents and First-year Graduates. Anesthesiology, 131(3), 668–677. https://doi.org/10.1097/aln.0000000000002777
- Taskina, E. A. (2020). The problem of emotional sustainability of professional burnout of medical workers [Problema emotsional'noy ustoychivosti professional'nogo vygoraniya meditsinskikh rabotnikov]. Bulletin of the Russian New University. Series "Man in the Modern World", 1, 34-39. https://doi.org/10.25586/RNU.V925X.20.01.P.034
- Vasilieva, I. V., & Grigoriev, P. E. (2017). Osobennosti emotsional'nogo vygoraniya vrachey v zavisimosti ot stazha raboty [Features of the burnout of doctors depending on the length of service]. Clinical Psychology, Psychotherapy and Psychoanalysis, 21(1), 21-27. https://cyberleninka.ru/article/n/osobennosti-emotsionalnogo-vygoraniya-vrachey-v-zavisimosti-ot-stazha-raboty
- Vinokur, V. A., & Klitcenko, O. A. (2012). Validizat͡sii͡a metodiki psikhologicheskoĭ diagnostiki professionalʹnogo «vygoranii͡a» v «pomogai͡ushchikh» professii͡akh [Validation of methods of psychological diagnostics of professional "burnout" in "helping" professions]. Medit͡sinskai͡a psikhologii͡a v Rossii [Medical psychology in Russia], (1), http://mprj.ru/archiv_global/2012_1_12/nomer/nomer21.php
- Vodopyanova, N. E. (2009). SHkala organizat͡sionnogo stressa [Organizational stress scale]. In N. E. Vodopyanova (Ed.). Psikhodiagnostika stressa [Psychodiagnostics of stress] (pp. 62-67). Piter.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
26 October 2020
Article Doi
eBook ISBN
978-1-80296-090-7
Publisher
European Publisher
Volume
91
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-340
Subjects
Self-regulation, personal resources, educational goals, professional goals, mental health, digitalization
Cite this article as:
Korehova, M. V., Novikova, I. A., Soloviev, A. G., & Kirov, M. Y. (2020). Anesthesiologists-Resuscitators’ Mental States In Extreme Activity Conditions. In V. I. Morosanova, T. N. Banshchikova, & M. L. Sokolovskii (Eds.), Personal and Regulatory Resources in Achieving Educational and Professional Goals in the Digital Age, vol 91. European Proceedings of Social and Behavioural Sciences (pp. 23-31). European Publisher. https://doi.org/10.15405/epsbs.2020.10.04.4

