Abstract
The aim of the research was to study the formation of students' communicative skills in the learning process using the example of the Standardized Patient methodology. The method of analysis of the products of activity (analysis of checklists) was used. An assessment was made of the effectiveness of classes on the formation of communication skills in the process of simulation training. A pronounced inconsistency of the assessment parameters of communicative techniques at the first stage of classes and its subsequent levelling at the final stage were revealed. Students were more likely to choose everyday speech strategy by using «household» level of encouraging and many specific medical terms in a process of communication with simulative patient at the beginning of the training. That strategy was not enough to score enough points according to the check-list of the station. The study showed the effectiveness of the method of developing communicative skills by introducing the “Difficult patient” cases for two days. These cases allow to evaluate several aspects of training: the ability to reveal a patient’s psychological status, the ability to choose the appropriate communication strategy based on the status, as well as the ability to provide recommendations on the patient’s adaptation in the situation of somatic disease.
Keywords: Simulation trainingcommunicative skillssimulated patientstandardized patientprofessional communication competences,
Introduction
The relevance of this study is dictated by the problems of a communicative skills forming with the patient in the process of students training in medical universities. The efficiency in the field of communication depends little on ethno-cultural traits, socio-economic and political situation, having a direct dependence on the individual psychological features of the person himself, in the field of the doctor’s professional activities, particularly. The scientific sources review showed that modern researches study the effectiveness of developing communicative skills depends on the specific form of training. In particular, the use of communicative skills can be realized only with the participation of simulated patients, which implies the construction of a patient-oriented model of interaction and, as a result, the formation of psychological and pedagogical competencies. According to the latest data from the Ministry of Health of the Russian Federation (2016-2017), patient complaints about doctors related to the lack of communicative competence of the latter have become more frequent. To date, there are no special disciplines in the curriculum, aimed only at the formation of communication skills. However, various simulation techniques exist and are actively used in the educational process. So, on the basis of the Kazan State Medical University, we made an attempt to create a specific set of tasks, based, in general, on the universal principles of simulation training for the communicative skills formation. 12 cases have been developed and implemented to evaluate various aspects of communication in problem situations. The main goal of the introduction of these cases was to prepare future specialists who should be capable to resolve potentially possible communicative problems in the doctor-patient dyad.
Problem Statement
In connection with the introduction of new educational standards of medical education in Russia, focused on a competency-based approach, increasing importance is being given to the formation of communication skills. Many Russian medical universities are implementing “standardized patient” (SP) programs, including for the formation of professional communications among medical students ( Davydova, Borodulina, Dyachenko, & Noskova, 2016; Davydova, Chernyadev, & Makarochkin, 2017; Svistunov, Shubina, & Gribkov, 2016; Serkina, 2017).
The problem of the communicative competence formation of medical students is relevant, as indicated by the article of Sanson-Fisher, Hobden, Waller, and Boyd ( 2018). Analyzing articles published in English from 2007 to 2016, the authors note an increase in publications devoted to the topic of comunicative compentencies (52 - from 2007 to 2008, 75 - from 2011 to 2012 and 116 - from 2015 to 2016) while the predominant were descriptive articles ( Sanson-Fisher et al., 2018).
Ali, Pelletier, and Shields ( 2017) presented a second-year analysis of the curriculum for students at Harvard-MIT School of Medicine. The goals of the program were the opportunity to practice communication skills with voluntary patients at the preclinical stage in a medical school, to receive immediate feedback from patients and doctors, to teach different styles and effective communication strategies. Bruen, Kreiter, Wade, and Pawlikowska ( 2017) noted the effectiveness of adaptive modeling of medical consultation. Adaptive simulations provide students with the opportunity to receive feedback and expert coaching to facilitate self-regulatory learning. The adaptive modeling platform offers 2 cycles, during which students are invited to analyze the results using automatic evaluations and personalized feedback. They are also encouraged to plan how they will improve their work through focused practice.
Communication programs for communicative skills of medical students with different groups of patients were also studied by Frost et al. ( 2015): the effectiveness of scenario-based teaching of clinical communication in teaching pediatric medicine was revealed. However, Pettit et al. ( 2018) in their study did not reveal a significant improvement in the students' use of communication elements or patient satisfaction after retraining in the communication script of the emergency department.
Thereby, medical programs based on simulation training, (standardized patient), are becoming more widespread. It is indicated that scenarios reflecting real situations (environment, atmosphere, interpersonal difficulties, etc.) contribute to the development of communication skills of future medical workers (Bressmann & Eriks-Brophy, 2012; Putter-Katz et al., 2018; MacLean, Geddes, Kelly, & Della, 2018; Ulutaş, Sözen, Yeğenoğlu, & Elçin (2018). It is noted by Kaplonyi et al. ( 2017) that programs based on the “standardized patient” methodology are widely recognized as an effective means of teaching communication skills, but there is insufficient evidence of how this affects patient outcomes and the economic benefits of this training method are not indicated. Gibson and Davidson ( 2016) found that within the framework of the Standardized Patient program, no benefits were found for students who received a video about their meeting with the simulative patient. The authors conclude that it is necessary to consider the use of SP in the context of the costs and resources associated with student learning.
Research Questions
The main research questions were:
An effectiveness in using “Difficult patient” cases
How effective is the use of simulation training for the formation of students’ communication skills during the training period and immediately after its completion by crossing the “Difficult patient” case station?
An observation of the dynamics of communication skills presented before, during and right after the training
Are there any significant differences in assessing the dynamics of the development of communication skills at different stages of formation?
Purpose of the Study
The main purpose of the study was to evaluate the effectiveness of the “Standardized Patient” methodology for the formation of student’s communication skills to perform high results in final exams.
The objectives of the study were:
To identify features of the assessment of the student's communication skills at the initial stage of the lesson, in the process and in the final stages.
To identify features of the dynamics of assessing communication skills.
Research Methods
A study of communication skills used in the learning process was carried out on the example of 5-year students (350 people) using the SP methodology.
Since 2014, on the basis of the Kazan State Medical University, a special set of tasks has been introduced to develop communicative skills of students (general medicine faculty and paediatrics faculty) in the framework of the discipline "medical psychology". It was the first time when the special set of communicational tasks were introduced at Russian medical university named like “difficult patient”. The set consisted of 6 training cases, the number of which was increased to 12 due to the growing needs in the field of “doctor-patient” communication, taking into account current trends in healthcare. Initially, the cases were more focused on assessing individual psychological features of character and personal traits of the patient, the cases were supplemented with tasks of finding proper communicative techniques in a particular situation, which was generally aimed at increasing the communicative competence of the future doctor.
The development of the stations included several stages:
First stage
That step included writing a station scripts based on the specifics of communicative problems in the healthcare system. We conducted an anonymous survey among patients from various clinics in Kazan. Based on the received information, the most common complaints and claims by patients on the communicative component of therapeutic interaction were “inattention”, “indifference”, “lack of empathy”, which caused patients to appear aggression, anxiety, hypochondria, etc. We developed the “Difficult Patient” set of tasks, which included 12 training stations with the participation of actors (for example, the station “Angry Patient”. The example of the task:
Second stage
The second stage was devoted to the development of curatorial documentation for a student playing the role of a doctor (curator student) and checklists of experts and actors, based on the criteria necessary for the formation of competencies in accordance with the Federal State Educational Standard within the framework of the discipline “Medical Psychology”.
Third stage
The third stage included the selection of actors and their preparation, one of the selection criteria was the lack of pedagogical and medical education, in order to avoid distortion of the student’s assessment of the actor. Actors were recruited from among third-year students of the theatre college who were trained at the Department of Psychology of Kazan State Medical University with practicing psychologists, psychotherapists and psychiatrists according to given scenarios. As a part of the adjustment of tasks, one of the stations was tested by teachers of the Department of Medical and General Psychology. The technical component of the educational process was to provide a recorded video of consultation from a box in a play situation, with subsequent analysis if necessary.
3 people had to participate playing each case of the station: a curator student (doctor), an expert student, and an actor (patient). Before the start of the training, a briefing was held with students, during which the main tasks for the corresponding role were identified. The main task of the curator student was to demonstrate communication skills in accordance with the station scenario, in a separate box, imitating a ward or viewing room. The play of a case was broadcasted by means of a video camera to the screen of an expert student who was in a specially equipped computer class, which made it possible to observe the situation and evaluate it in real time. After passing the station, each of the participants was offered to fill in the relevant documentation: the student-curator filled out a curatorial documentation, the expert and actor - check-lists. At the end of each lesson, a briefing was also conducted with an analysis of the main mistakes and questions of students.
Since the training was carried out as a part of the “Medical Psychology” subject, the curatorial documentation included a description of psychological traits of the patient such as temperament, character and personality features, the reasons for the patient’s state and the main communicative techniques aimed at solving the problem of a “Difficult patient”.
An expert checklist other than traditional assessment (done/not done) was included blanc space for an expert’s own opinion for valid communicative turns giving an outside perspective.
An actor checklist was conditionally divided into two parts: compulsory skills (welcoming, selfpresentation etc.) and special skills aimed at overcoming a particular communicative difficulty of the case. Also, an actor could leave an open response feedback to a student.
The training process was divided into two days: each student was playing 6 times per day being a curator (3 cases) and an expert (3 cases different from the first). In this way all 12 cases were passed by a student during two days.
Findings
In the course of the analysis of the documentation of the first day training, the following data were obtained.
The analysis and the discussion of the first training day results
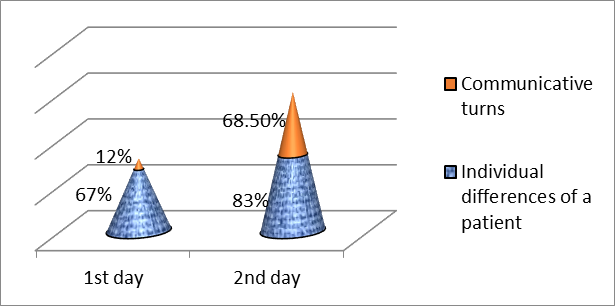
When analysing the curatorial documentation, conditionally divided into two parts (individual psychological traits and communicative techniques), it could be noted that for the majority of students (67%) assessment of the individual psychological characteristics of the patient was not difficult, however, for more than a half of the students it was difficult to describe how to talk with a patient, what to say and how to react. There were only 12% of students who could find valid communicative techniques for solving the problem that coped with this part of the task (Fig.
As a rule, students offered general recommendations like to “reduce an anxiety”, “psychologist consultation”, which was noted in the actor’s checklist in the form of an unsatisfactory student assessment.
In particular, many students did not achieve the satisfactory result demonstrating skills from the mandatory section: greeting, self-presentation, obtaining informed consent for conversation and physical examination, washing hands. In addition, many actors noted such shortcomings of students' work as a too loud voice, fast pace of speech, improperly chosen posture and distance for communication, and such subjective comments as “strong smell of perfume”, “smell of garlic”, “too long nails”, etc.
From the positive subjective comments could be noted such statements as “a good doctor”, “easy to communicate”, “very convincing”.
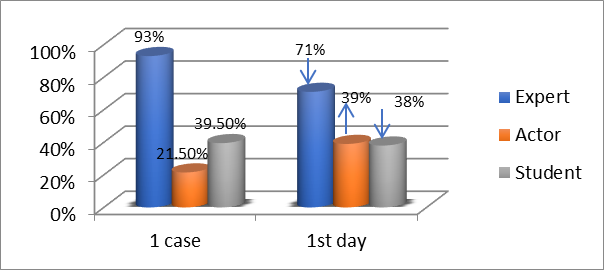
The expert’s work at the beginning of the assessment was poorly differentiated: on the first day, most students used only a formalized approach (done/ failed), experts in 93% of cases rated their colleagues as “completed the task”, although the actor’s assessment was unsatisfactory.
Thus, a large number of discrepancies could be noted on the first day of the training - the discrepancy between three types of documentation is quite pronounced. Experts rated the work of colleagues highly (93%), while the actor rated a student as a doctor only in 21.5%, and the number of students who completed the task for the curator (doctor) (by fulfilling the documentation) was 39.5% (Fig.
Each student had an opportunity to watch a video of his work. The following data was received, when requesting feedback from students at the end of the first training day: many students were anxious, noted fear and tension before starting work, which they associated with the novelty of the assignment. However, on the first day it was noted the “usefulness” of this format of classes, “the interesting work of the actors”, “the opportunity to observe oneself from the outside”.
The analysis and the discussion of the second training day results
The results obtained after the second day of class, significantly differed from those on the first day: the percentage of students who completed the task increased significantly (39.5% at the beginning of the first day and 82% at the end of the second), also significantly increased the percentage of students who completed the tasks with the description of communicative techniques (68.5%) (see fig.
Significant changes occurred in the student’s assessment of the actor, during the study period, the grade increased from 21.5% to 75%. In addition, the expert’s work was slightly adjusted, a decrease was noted: some students rated their colleagues more critically (from an overvalued 93% to 85%) and offered their own methods of communicative techniques more detailed (Fig.
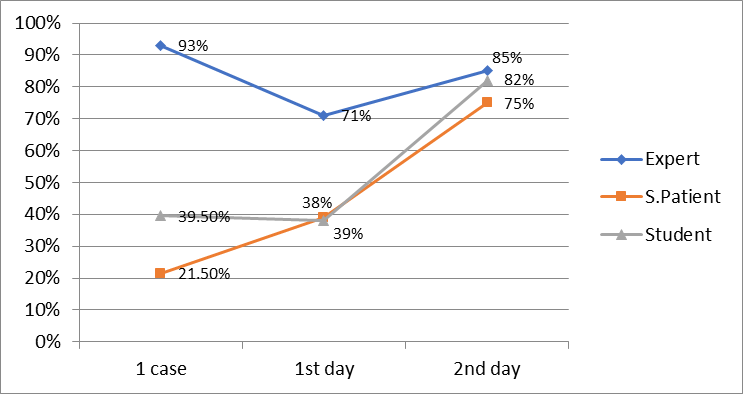
At the end of the second day of the training, students noted that it was much easier for them to cope with the task. The main evidence of the positive dynamics and effectiveness of that format of classes was an indicator of the consistency of three student assessment parameters, which is illustrated in Figure
Conclusion
As a result of the study, the following conclusions were made:
Communication skills at the first step of training
Many students in practice tried to communicate correctly with patients on an intuitive level, but, in the end, could not implement certain communicative techniques and techniques aimed at solving the problem. This aspect allows us to note the importance of certain psychological and pedagogical skills of a doctor for building communication and, subsequently, teaching the patient constructive behaviour.
Communication skills formation at the last step of training
It is possible to be said that there is a high efficiency of such educational technology as a training station for the formation of students' communication skills. The developed program allows to evaluate several aspects of training: the ability to evaluate the patient’s psychological status, the ability to choose the appropriate communication strategy based on the status, as well as the ability to provide recommendations on the patient’s adaptation in the situation of somatic disease.
However, it is worth noting that the study showed a certain trend in the effectiveness of the method of developing communication skills by introducing the “Difficult patient” stations for only two days, further research and the expansion of the extra methods of assessment are needed to obtain more objective and accurate data.
The question remains open about maintaining the acquired knowledge and skills by the student over a longer period of time.
Acknowledgments
The work is performed according to the Russian Government Program of Competitive Growth of Kazan Federal University.
References
- Ali, N., Pelletier, S., & Shields, H. (2017). Innovative curriculum for second-year Harvard-MIT medical students: practicing communication skills with volunteer patients giving immediate feedback. Adv Med Educ Pract, 8, 337–345. https://doi.org/10.2147/AMEP.S135172
- Bressmann, T., & Eriks-Brophy, A. (2012). Use of simulated patients for a student learning experience on managing difficult patient behaviour in speech-language pathology contexts. International Journal of Speech-Language Pathology, 14(2), 165-173.
- Bruen, C., Kreiter, C., Wade, V., & Pawlikowska, T. (2017). Investigating a self-scoring interview simulation for learning and assessment in the medical consultation. Adv Med Educ Pract, 8, 353–358. https://doi.org/10.2147/AMEP.S128321
- Davydova, N. S., Borodulina, T. V., Dyachenko, E. V., & Noskova, M. V. (2016). Communicative and practical skills of pediatric health care provider at Ural State Medical University. Medical education and professional development, 3. Retrieved from https://rosomed.ru/theses/342
- Davydova, N. S., Chernyadev, S. A., & Makarochkin, A. G. (2017, September 12). A pilot of assessing of medical workers. Rosomed. Retrieved from https://rosomed.ru/theses/433
- Frost, K., Metcalf, E., Brooks, R., Kinnersley, P., Greenwood S., & Powell, C. (2015). Teaching pediatric communication skills to medical students. Adv Med Educ Pract, 6, 35–43 https://doi.org/10.2147/AMEP.S68413
- Gibson, S. J., & Davidson, Z. E. (2016). An observational study investigating the impact of simulated patients in teaching communication skills in preclinical dietetic students. Journal of Human Nutrition and Dietetics, 29(4), 529-536. https://doi.org/10.1111/jhn.12352
- Kaplonyi, J., Bowles, K. A., Nestel, D., Kiegaldie, D., Maloney, S., Haines, T., & Williams, C. (2017). Understanding the impact of simulated patients on health care learners’ communication skills: a systematic review. Medical Education, 51(2), 1209-1219. https://doi.org/10.1111/medu.13387
- MacLean, S., Geddes, F., Kelly, M., & Della, P. (2018). Simulated patient training: Using inter-rater reliability to evaluate simulated patient consistency in nursing education. Nurse Education Today, 62, 85-90. https://doi.org/10.1016/j.nedt.2017.12.024
- Pettit, K. E., Turner, J. S., Pollard, K. A., Buente, B. B., Humbert, A. J., Perkins, A. J., …& Kline, J. A. (2018). Effect of an educational intervention on medical student scripting and patient satisfaction: A randomized trial. Western Journal of Emergency Medicine, 19(3), 585-592. https://doi.org/10.5811/westjem.2018.1.35992
- Putter-Katz, H., Gvion, A., Wechsler-Kashi, D., Said, L. A. B., Yaacobi, H., Feldman, I., Shalomson, O., & Ziv, A. (2018). Students’ evaluation of simulation-based training in a communication sciences and disorders program. Journal of Allied Health, 47(2), 113-120.
- Sanson-Fisher, R., Hobden, B., Waller, A., & Boyd, L (2018). Methodological quality of teaching communication skills to undergraduate medical students: A mapping review. BMC Medical Education, 18(1), 1. https://doi.org/10.1186/s12909-018-1265-4
- Serkina, A. V. (2017). Views of medical students around the communicative aspects of working with patients. Rosomed. Retrieved from https://rosomed.ru/theses/472
- Svistunov, A. A., Shubina, A. A., & Gribkov, D. M. (2016). Communicative skills in medicine: the experience and perspectives in Russia. Medical education and professional development, 3. Retrieved from https://rosomed.ru/theses/341
- Ulutaş, D. E., Sözen, Ş. B, Yeğenoğlu, S., & Elçin, M. (2018). Feedback for a simulation practice on communication skills in pharmacy education: A pilot study. Marmara Pharmaceutical Journal, 22(2), 314-321. https://doi.org/10.12991/mpj.2018.69
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
23 January 2020
Article Doi
eBook ISBN
978-1-80296-077-8
Publisher
European Publisher
Volume
78
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-838
Subjects
Teacher, teacher training, teaching skills, teaching techniques
Cite this article as:
Sakharova, A. E., Makaricheva, E. V., & Pyrkova*, K. V. (2020). The Simulation Training Analysis For The Communicative Skills Formation In Medical Education. In R. Valeeva (Ed.), Teacher Education- IFTE 2019, vol 78. European Proceedings of Social and Behavioural Sciences (pp. 660-668). European Publisher. https://doi.org/10.15405/epsbs.2020.01.72
