Abstract
Background. Femoral fractures in the elderly are secondary to the loss of slow axial lesions as well as an increased risk of falling. In order to reduce the downward trauma, the neuromuscular re-education program will be adapted to the conditions and needs of the patient's home, recommending exercises for balance, strength, coordination and response time with moderate intensity. Objectives. The aim of the research was to structure a kinetic intervention program tailored to the patient's particularities and to finally achieve a social reintegration at a qualitative level. The planning of each phase of the program includes a didactic component that promotes the improvement of the patient's condition beforehand by providing information and guidance for a successful return to daily activities. Material and methods. The article represents a study case of an 81-year-old patient, G.F., who presented herself at the Kineto Fit Recovery Center in Brasov, Romania, in May 2017, for a medical assessment, accusing the back pain. In the patient's medical history, she was reported to have suffered a right fracture of the femur in June 2016 and started her anti-osteoporotic treatment in the autumn of that year. Results. Following medical consultation, the diagnosis was fracture of the rigid femoral neck straight at the hip. Conclusions. As a result of the research, it was found that by applying a specific kinetic program an improvement of the functional parameters can be obtained, the results obtained, graphically inscribed, confirm this statement.
Keywords: Interventionarticulate mobilitymuscular forcefemoral fracture”
Introduction
The fracture of the femur consists of the rupture of the upper leg (thigh bone). Most femoral fractures occur in the femoral neck (Haider et al., 2018) and in the trochanteric region, just below the femoral neck. Femoral fractures are common and can be very serious because they often occur in the elderly and usually require surgical correction followed by a slow recovery (Zielinski et al., 2013; Madsen, 2010, p.1397; Tache, 2011; Nechita, 2016).
Studies show that adults who break their femur and are not already interned in a hospital or in the hospital may require special care for one year in a proportion of 25% of the cases (Kral et al., 2018; Sheikh et al., 2018; Qureshi et al., 2018). They are usually diagnosed based on objective examination and bone radiography (Hurry et al., 2018). The signs of the femur fracture include the strong pain, the inferior limb shorter than the unaffected and external rotation of the femur.
Femoral fractures are recognized to be a major public health problem (Cooper et al., 1992) and are a global concern, resulting in poor outcomes and high health care costs. They mostly affect people > 80 years (Denk et al., 2018). The femoral neck fracture is one of the elderly-specific disorders, important through its immediate and long-term consequences. The fracture occurs more frequently in women than in men, being in direct relationship to osteoporosis, a condition that tends to fragile the bones, predisposing them to fractures Usually, the elderly, over 65 years of age (possibly dizzy due to neurological conditions) can fall from the feet with an impact on the hip, resulting in femoral fractures. They are serious because a fracture of the femoral neck leads to immobilization of the patient in bed.
Other studies describe the objectives of kinetotherapy in preventing the fall as: improving balance; increasing muscle strength; increase in tonus; increasing mobility; improving coordination; lowering anxiety and increasing confidence in own power. (Ciobanu, et al., 2007)
The elderly with a hip fracture has hip pain, can't lift up, can't get out of bed, can't to go anymore. All this can lead to very serious complications and even to the death of the patient (Sîrbu, 2015). They show acute pain, but the pain is an unpleasant sensory and emotional experience associated with actual or potential femoral damage (Loeser & Treede, 2008).
The operation of the fracture of the femoral is zero without rapid, sustained and correct recovery. After surgery, as soon as the effect of the anesthetize passes, the patient begins the assisted exercises under the supervision of a physical therapist (Sîrbu, 2015; Tache, 2011; Curițianu, 2015).
However, in order to alleviate the trauma of the condition, the kinetic program will be adapted to the conditions and needs of the patient's home, recommending exercises for equilibrium training, strength, coordination, and moderate response times (Lazăr et al., 2008, Nechita, 2013).
Problem Statement
Participants
The study was conducted in 2017 at the Kineto Fit Recovery Center in Brasov, Romania. The subject of the case study was (G.F.) with aged 81. The subject was investigated after having followed a kinetic program on recovery of the femoral fracture.
The research covered two evaluation points, before starting the pre-test procedure and afterwards, the post-test. The articular test (AT) as extension and flexion movement and the muscle test (MT) on movements in the femoral joint.
The program consisted in the application of methods and means based on kinetic activities that will primarily aim at increasing the degree of hip stability by toning the muscles and, secondly, increasing the degree of mobility to achieving functional movement angles. During the application of the kinetic program, a medicinal treatment will also be given to reduce pain and inflammation (oral analgesia).
Research Questions
The program with assisted exercises is a neuromuscular reeducation program aimed at toning the muscles and increasing the articular mobility.
The kinetic program aims at strengthening the fracture of the femur. This process is dependent on the subject's age and location of the condition.
The program was structured over 3 months and included two main intervention stages:
Stage I. Pharmaceutical treatment.
Stage II. Neuromuscular re-education program.
The program consisted of 20 minutes sessions and the exercises included in the program had the role of neuromuscular reeducation the patient's femoral fracture.
Purpose of the Study
The paper aims to present the advantages of implementing a neuromuscular re-education program of femoral fracture pathology in elderly patients.
The medical recovery in this case, by the means used, leads to improved health, thus contributing to maintaining health through better functioning of all joints and leg muscles.
The theme of this study is to show the benefits of well-planned assisted kinetic exercises in improving the pathology of fracture of the femur.
Research Methods
The research covered two evaluation points, before starting the pre-test procedure and afterwards, the post-test. The articular test as extension and flexion movement and the muscle test on movements in the femoral joint.
Implementation of physical therapy was performed by the following stages using different means:
At this stage, the modalities of intervention included the following:
-
-
Cardio warm up - the ergonomic bicycle. Performing a 10-20 minutes cardio exercise before stretching and assisted kinetic exercises. This will help prevent injuries and provide optimum performance.
Stretching: Hamstring stretch with band – dorsal decubitus position, stretched legs, the band held with two hands and trapped by the foot. The simultaneous lifting of the leg with the extension of the rope, 4 series of 5 repetitions, maintaining the position 10 seconds, 20 seconds break.
Stretching: Groin stretch - Cobbler’s position, bending the knees and bringing legs to the pelvis so that the soles of the feet touch. Push your elbows on your thighs, bringing them closer to the floor, 4 series of 5 repetitions, maintaining the position 10 seconds, 20 seconds break.
Stretching: piriformis stretch - dorsal decubitus position, the legs bending and the pulling one knee in towards your chest. The grab the ankle of involved leg and pull towards the chest. This will cause a rotation of hip. A stretch will be felt deep within the buttocks. 4 series of 5 repetitions, maintaining the position 10 - 15 seconds, 20 seconds break.
The assisted kinetic exercises:
1.Initial position: dorsal decubitus position, hands near the body, bending knees.
T1 – dorsal flexion of the bilateral foot;
T2 – plantar flexion of the bilateral foot, dosage: 2 series of 10 executions.
2.Initial position: idem1.
T1 – external rotation of the bilateral foot;
T2 – internal rotation of the bilateral foot, dosage: 2 series of 10 executions.
3.Initial position: standing on the mattress, backwards support on the palms
T1 – triple flexion of the right limb;
T2 – returning to the initial position;
T3 – triple flexion of the left limb;
T4 – returning to the initial position (with heels remaining on the floor), dosage: 2 series of 8 executions.
4.Initial position: lateral decubitus position on the healthy inferior limb side, hand under the head.
T1 – inferior limb abduction from the hip articulation;
T2 – inferior limb adduction from the hip articulation, dosage: 2 series of 4 executions.
5.Initial position: sitting on a chair with hands near the body.
T1 – neck flexion – inhale;
T2 – neck extension (movements executed with opened eyes) – exhale, dosage: 2 series of 6 executions.
6.Initial position: sitting on a chair, hands on the iliac crests.
T1 – head rotation to the left;
T2 – head rotation to the right (movement executed with opened eyes following the objects around), dozing: 3 series of 4 executions.
7.Initial position: sitting on the chair, hands grabbing a stick from its ends.
T1 – lifting the stick above the head (inhale);
T2 – lowering the stick in the initial position (exhale), dozing: 1 series of 8 executions.
8.Initial position: sitting on the chair, hands on the iliac crests.
T1 – twisting the torso to the right;
T2 – twisting the torso to the left, dozing: 1 series of 8 executions.
9.Initial position: sitting slightly apart, facing the espalier, hands grabbing the slat from the shoulder level. The therapist is sitting behind the patient with his hands on the patient’s hips and executes light off balanced movements, the patient trying to find his way back to that initial balance; dozing: 1 series of 10 executions.
10. Initial position: sitting on a ball with a large diameter, the patient grabbing his companion’s hands. The therapist sitting behind the patient executes light rolling of the ball, the patient finding herself in an off balanced situation; dozing: 1 series of 10 executions.
The exercise program has been taking place in a rather slow pace, interspersed with resting periods and relaxation. The structure of the exercises was based on a combination of isotonic and isometric contraction.
At first, the exercises were analytical, after which the effect of the exercises was to stimulate as many muscle parts.
Findings
The data gathered from the Pre and Post evaluation of the articular and muscular testing are presented in the following Table
The articulate limitation to the level of the affected hip has occurred due to the apparition of pain, the right leg, the healthy one, being immobilized to the patient’s possibilities. The mobilization muscular force of the right leg has been initially conducted only against gravitational force, in comparison to the healthy leg, which the patient managed to mobilize to a maximum muscular force (Sbenghe, 1981; Cordun, 2009). The following graph presents the evolution of the articulate amplitude (Figure
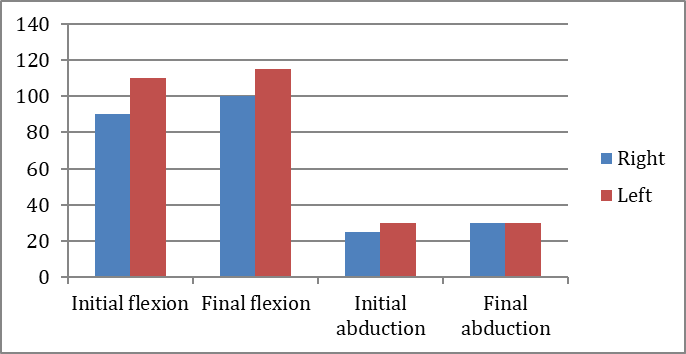
Figure
- For Flexion and Abduction, AT – The right femoral fracture values were increased at Pre and Post – test. These values were significantly increased from Pre to Post – test: by 10° - Flexion and 5°- Abduction.
Recorded values were compared to significantly the left leg healthy values. Thus, the values of 10° Flexion/Post - test right leg parameters was compared to left leg values at a difference of only 15° (Table
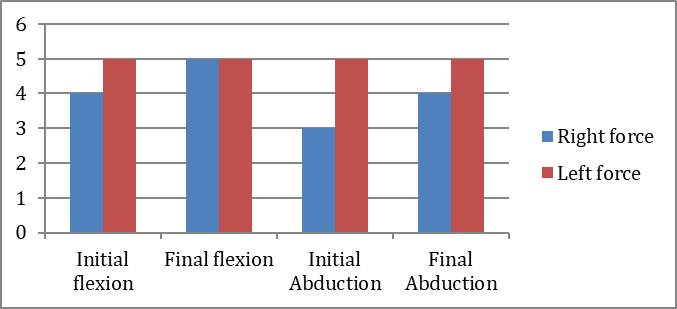
The Figure
On the abduction movement, was noticed the growth of the muscular movement from the F3 degree to the F4, within this movement, the right leg being weaker than the left leg. However, muscle movement with the F4 value of the right foot compared to the healthy left leg degree F5 has not been completely rehabilitated.
Also, both to flexion and abduction in the Post test, the subject shows significant improvements obtained following the neuromuscular re-education program.
Conclusion
The neuromuscular re-education program introduces a significantly improvement in Post - test values at TA and TM. Thus, the program meets the established objectives, recording significant differences in Pre and Post - test, improving the health of the subject.
The findings of the present study demonstrate a positive effect in the improvement of right femur fracture at TA with a progress of 10° to flexion and 5° to abduction and to TM marking a maximum degree of movement of the force F5 to flexion and F4 to abduction
The effects of the program presented the values of the leg affected at values close to those of the healthy leg, diminishing the back pain and forming the patient's habit of practicing the exercises.
The indications given to the patient at the end of the recovery treatment included: repeating the home exercise series.
]
References
- Ciobanu, D., Dan, M., Lozincă, I., Marcu, V., Pâncotan, V., Serac, V., & Şerbescu, C. (2007). Kinetoterapia în patologia geriatrică [Kinetotherapy in geriatic pathology]. Craiova: Editura Universitaria.
- Cooper, C., Campion, G., & Melton, L. (1992). Hip fractures in the elderly: a world-wide projection. Osteoporos International, 2(6), 285 -289.
- Cordun, M. (2009). Kinantropometrie [Kinanthropometry]. Bucureşti: CD PRESS.
- Curitianu, I.M. (2015). Echipamente, aparate şi instalaţii utilizate în kinetoterapie [Equipment, apparatus, installation used in kinetotherapy]. Brasov: Editura Universităţii Transilvania din Braşov.
- Denk, K.., Lennon, S., Gordon, S., & Jaarsma, R.L. (2018). The association between decreased hand grip
- strength and hip fracture in older people: A systematic review. Journal of Experimental Gerontology, 111, 1-9.
- Haider, T., Schnabel, J., Hochpochler, J., & Wozasek, G.E. (2018). Femoral shortening does not impair functional outcome after internal fixation of femoral neck fractures in non-geriatric patients. Archives of Orthopaedic and Trauma Surgery, 138(11), 1511 -1517.
- Hurry, J.K., Rehan, S., Spurway, A.J., Laende, E.K., Wilson, J.L.A., Logan, K.J.,…El-Hawary, R. (2018). The reliability of radiostereometric analysis in determining physeal motion in slipped capital femoral epiphysis in standard uniplanar and low-dose EOS biplanar radiography: a phantom model study. Journal of Pediatric Orthopaedics - Part B, 27(6), 496-502.
- Kral, R., Osima, M., Vestgaard, R., Richardsen, E., & Bjornerem, A. (2018).Women with fracture, unidentified by FRAX, but identified by cortical porosity, have a set of characteristics that contribute to their increased fracture risk beyond high FRAX score and high cortical porosity. Journal of Endocrinology & Metabolism, 116, 259 – 265. https://dx.doi.org/
- Lazăr, L., Marcu, F., Cioară, F., & Rus, M. (2008). Rolul kinetoterapiei în prevenţia căderilor la vârstnici. Clujul Medical Revista de Medicină şi Farmacie, 4, 451-454
- Loeser, J.D., & Treede, R.D. (2008). The Kyoto protocol of IASP Basic Pain Terminology. Pain PubMed, 137(3), 473-477. https://dx.doi.org/
- Madsen, J.E. (2010). Treatment of displaced intracapsular hip fractures in older patients. Editorials, BMJ., 340:c2810, p. 1397. https://dx.doi.org/
- Nechita, F. (2013). Gimnastica in kinetoterapie [Gymnastics in kinethoterapy]. Brasov: Editura: Universității Transilvania Brasov.
- Nechita, F. (2016). Effects corrective gymnastics physical education and sport lesson. Revista: Buletinul Universității Transilvania Brasov, 9(58), 53-60.
- Qureshi, M., Liew, I., & Bailey, O. (2018). CRP monitoring in fractured neck of femur. A waste of resource? Injury – International Journaal of the care of the Injured, 49(10), 1855 – 1858.
- Sbenghe, T. (1981). Recuperarea medicală a sechelelor posttraumatice ale membrelor [Medical recovery of post-traumatic limbs sequelae]. Bucureşti: Editura Medicală.
- Sheikh, H.Q., Aqil, A., Hossain, F.S., & Kapoor, H. (2018). There is no weekend effect in hip fracture surgery - A comprehensive analysis of outcomes. Surgeon – Journal of the Royal Colleges of Surgeons of Edinburgh and Ireland, 16(5), 259 -264.
- Sîrbu, P. (2015, October 27). Fractura de col femural: Operaţia, cea mai bună soluţie pentru un vârstnici!. Retrieved from https://www.ziaruldeiasi.ro/stiri/fractura-de-col-femural-operatia-cea-mai-buna-solutie-pentru-un-varstnici--86357.html
- Tache, G.O. (2011, October 26). Metode de recuperare în fractura de col femural. Retrieved from https://www.farmaciata.ro/metode-de-recuperare-in-fractura-de-col-femural/
- Zielinski, S.M., Meeuwis, M.A., Heetveld, M.J., Verhofstad, M.H.J., Roukema, G.R., Patka, P., & Van Lieshout, E.M.M. (2013). Adherence to a femoral neck fracture treatment guideline. International Orthopaedics, 37(7), 1327 – 1334.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
15 August 2019
Article Doi
eBook ISBN
978-1-80296-066-2
Publisher
Future Academy
Volume
67
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-2235
Subjects
Educational strategies,teacher education, educational policy, organization of education, management of education, teacher training
Cite this article as:
Cioroiu*, S. G. (2019). The Study Of The Kinesiotherapeutic Intervention In Femoral Fractures. In E. Soare, & C. Langa (Eds.), Education Facing Contemporary World Issues, vol 67. European Proceedings of Social and Behavioural Sciences (pp. 2203-2210). Future Academy. https://doi.org/10.15405/epsbs.2019.08.03.273
