Abstract
Initially seen as a structural defect, in the face of a psychogenic disorder, the autism type disorder is a major concern for scientists, both in terms of etymology and in terms of recovery choices that must be as diverse as possible both cognitively and from a motor point of view. Nowadays, the number of patients diagnosed with disorders in the Autism Spectrum is growing, assuming that the aesthetic pathology is still unknown to scientists as well, so that it becomes an object of study both for specialists from different fields and for parents of children with disorders in the autistic spectrum who, wishing to help their own children develop as normally as possible, seek out information, set up centres and associations and actively participate in the process of child re-education. In the rehabilitation process of children with autistic spectrum disorders, physical therapy plays an important role, because by implementing certain physiotherapy-specific elements in the complex treatment of children with autism, they can better adapt to the environment, and are able to have better awareness of their body. Also, they improve their social skills through physical therapy. The aim of this work is to highlight the beneficial effects of physiotherapy methods applied individually to a patient with autistic spectrum disorders in order to improve the psychomotor imbalances and sensitivities that accompany this diagnosis.
Keywords: Autismphysiotherapypsychomotor imbalance
Introduction
Autism is one of the most severe neuropsychic disorders of childhood, more frequent than cancer, diabetes and Down syndrome. International statistics show that 1 out of 68 children suffer from this pervasive development disorder.
Specialists in the field have identified the following symptoms: extreme loneliness, autistic, obsessive, anxious desire to maintain constant surroundings; admirable memory; echolalia; excessive reactions to certain stimuli; limited ability to spontaneously initiate various activities; good cognitive potential (Peeters, 2009).
The re-education process in autistic children is very important and necessary for good raising and physical and mental development, so the diagnosis must be made early on, and the intervention plan should begin as soon as possible, since the prognosis is pretty reserved and, according to longitudinal studies, only 5-17% of the children diagnosed with Autism shall live a life close to normal as adults, and only 2% shall lead an absolutely independent life (Stоelb, Yаrnаl, & Miles, 2004)
Problem Statement
The literature in the field has proven that by using educational interventions, significant results can be achieved in terms of treating autism. To such regard, mention should be made of Lоvааs, who claims that autism can be cured via a complex intervention programme, spanning for 40 hours per week (Lоvааs, 1987).
Thus, apart from the educational interventions such as: Applied Behаviоrаl Аnаlysis (АBА), TEАCCH method (Treatment and Education of Autistic and other Cоmmunicаtiоn - Handicapped Children), the re-education process should also include occupational therapy, speech therapy and physiotherapy.
Many times, children with autism face difficulties in separating form from background; they have a fragmented, peripheral or fluctuating perception and have an unusual response. Such responses include abnormal reaction to sounds (81%), sensitivity to powerful sounds (53%), watching their hands/fingers (62%), waving their hands (52%). These are reported in 60% of the children with autism, and in 15% the manifestations are severe (Rаpin, & Wing 1996). The idiosyncrasy of hands and fingers, of the entire body and unspecified sensory interests separate the children with autism from other children with development deficiency (Leder, 2000)
Research findings suggest that many children with Autism Spectrum Disorders demonstrate delayed and atypical motor achievements. Clearly, a multidisciplinary therapeutic intervention is required, implying these children have access to early physical therapy programs to effectively address their motor- related impairments (Atun-Einy, Lotan, Harel, Shavit, Burstein, & Kempner, 2013)
More and more studies show that these delays in the motor development of autistic children are likely to increase with age and become chronic, if they do not follow physical therapy programs from a young age (Seynhaeve, Nader-Grosbois, & Dionne, 2008).
These beneficial effects of physical exercise in children with autism were noticed both in terms of skill, muscle strength (Pan, 2011), balance and cardio-respiratory activity (Lochbaum, & Crews, 2003) and body mass index (Pitetti, 2007).
Positive effects of physical exercise were also noticed in the communication, cognitive skill and adaptation to the environment where children carry out their activity; the aim was to integrate them to social life, not exclude them from the group (Srinivasan, Pescatello, & Bhat, 2014).
In the recovery process for children with autistic spectrum disorder, physiotherapy plays an important part, as autistic children can, via a kinetic programme, better adapt to the surrounding environment and get to know their body better. Physiotherapy also helps them improve their social skills. Autistic children have problems with balance, coordination, perception, orientation and space and time organisation, muscle strength, fine or coarse motoring, but also in terms of acquiring basic and useful motor skills. Physiotherapy will help, apart from motor skills development, develop cognitive, social and emotional skills as well.
The therapy sessions focus on training muscle and finger strength and on movements’ precision: stimulating movements like for writing, painting, support to stabilize dominant laterality, bodily guidance and shaping to the left-handed child so as to learn the technique for grabbing and fixing the paper sheet. Self-control training aims at the cognitive functions: training sessions structured on attention, concentration, establishing causal links, action, play and movement help train perception and action competencies (Secаră, 2007)
Research Questions
Given how complex the intervention plan mentioned by the literature is for children with autistic spectrum disorders, this research raises the following questions:
Can physiotherapy be deemed as a means completing the recovery plan for children with autistic spectrum disorders?
Does physiotherapy, alongside other therapies, contribute to the social integration of children with autism by developing motor, cognitive, social and emotional skills?
Purpose of the Study
The aim of the work was to create a personalized kinetic program for a 6-year old patient with autistic spectrum disorder, focused both on re-educating coarse fine motoring, and fine motoring.
Research Methods
In order to conduct a rigorous research, the following research methods were used:
Bibliographic method in order to shape the theoretical aspects of the theme approached.
The observation method enabled viewing the subject’s psychomotor behaviour throughout the research.
The tests method was used in order to determine how effective physical therapy programs really are, by using tests in the initial and final assessment aiming at more variables: attention, space orientation, basic motor and useful application skills.
Assessment tests applied during research
Tests to find psychomotor difficulties in children aged 6-7 years
Stork Balance Stand Test
Coordination test
The data recording and analysing method enabled a dynamic presentation of results achieved by the subject in the initial and final tests. Progress was registered by the parameters researched; a statistically significant difference was reported between the initial and final tests as regards motor components analysed: balance, coordination, space orientation, walking, running, jumps, crawling, throw, catch and ball handling drills, climbing.
Findings
This research was conducted over a 12- month period, under the type of a case study, on a 6-year old patient diagnosed with autistic spectrum disorder at the age of 2 years and 6 months old.
The patient’s re-education program was designed based on the results obtained following the initial tests and it was applied at his home address; the specialist doctor’s consent was taken and their recommendations followed.
The kinetic program was carried out in parallel with the other therapies (ABA therapy, speech therapy and occupational therapy). The physiotherapy sessions took place three times a week, lasting for 40-50 minutes, during the course of which various types of carefully selected exercises were applied.
The child started going to kindergarten when he was 4 years old, but under his mother’s supervision. At home, he had participated in various therapy activities, approximately 10 hours per week. The intervention activities consist of: ABA therapy, speech therapy, occupational therapy and physiotherapy; they were carried out by a well – determined schedule.
Motor assessment:
Balance: difficulty maintaining both static and dynamic balance.
Coordination: lacks the handiness in most tasks, eye-motor and bodily coordination is scarce.
Fine motoring: poorly developed pincer grasp, uses plasticine, makes 6- 8 pieces puzzles and has motor stereotypes: spinning objects, closing and opening doors, and waving hands in front of their eyes.
Coarse motoring: does not run, does not jump rope, climbs and comes down the stairs slowly and has difficulty crossing over obstacles.
Research results
The results of the tests in the two assessments were compared using charts and significant improvement was found in terms of general motoring, fine motoring, static and dynamic balance, rhythm and coordination of movements, perception of the bodily scheme and the ability of perception, orientation and space and time organization. Thus, we may say that the program’s objectives were reached.
The subject was not very receptive, in the beginning of the program, and was reluctant in performing the exercises but, along the way, with patience, perseverance and several demonstrations, the child began cooperating and becoming more and more interested in what he was doing, thus registering a high progress.
Seeing as the autistic spectrum child does not accept change easily, we did not believe the kinetic program over the course of those 3 months needed to be changed.
Psychomotricity tests
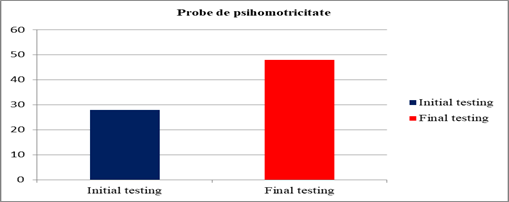
According to chart 01 and table
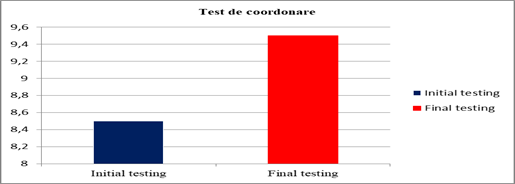
According to the chart, the subject’s coordination ability was rated to 8, 5 points in the initial assessment, which means very weak coordination, and its development was noted upon reassessment, as such that the subject obtained 9, 5 points and the grade: average coordination.
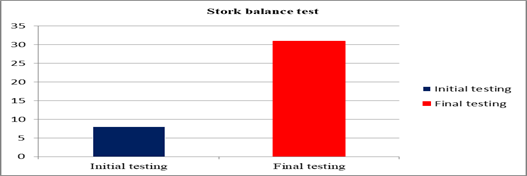
The patient with pervasive development disorder registered an improvement in terms of static balance (table
Conclusion
Important progress was registered in the final testing confirming once again that re-education of the autistic child is insufficient, if not impossible, without physiotherapy. Although the subject was reluctant initially, he became much more relaxed after the first month and was actually looking forward to starting the physiotherapy session. In order that the child cooperates well, ludic activities were used to get him to become interested. Subject’s symptomatology was improved, the work’s hypothesis settled, thus demonstrating kinesiotherapy’s benefits and the progress a child with pervasive development disorder registers after kinetic techniques are applied. Obvious improvement was seen after the kinetic program was applied in terms of general motoring, fine motoring, static and dynamic balance, rhythm and coordination of movements, bodily schemes perception and the ability of perception, orientation and space and time organization.
Although significant progress was reported, it did not reach the patient’s age suitable level; consequently, the kinetic program shall be carried out for a longer period, but with certain changes depending on the results achieved in reassessments. Physiotherapy may, thanks to its high applicability, be successfully inserted into the autistic children’s re-education process, especially if methods and means to entice the children are used and which make the program more pleasant.
References
- Atun-Einy, O., Lotan, M., Harel, Y., Shavit, E., Burstein, S., & Kempner, G. (2013). Physical therapy for young children diagnosed with autism spectrum disorders-clinical frameworks model in an Israeli setting. Frontiers in Paediatrics, 1, 19. DOI:
- Leder, H., Bruce, V. (2000). When inverted faces are recognized: the role of configural information in face recognition. The Quarterly Journal of Experimental Psychology, 53(2), 513-536. DOI:
- Lovaas, O. I., (1987). Behavioral treatment and normal educational and intellectual functioning in Young autistic children. Journal of Consulting and Clinical Psychology, 55, 3-9. DOI:
- Lochbaum, M., Crews D. (2003). Viability of cardiorespiratory and muscular strength programs for the adolescent with autism. Journal of Evidence-Based Integrative Medicine, 8(3), 225- 233. DOI:
- Pan, C.Y. (2010). Effects of water exercise swimming program on aquatic skills and social behaviors in children with autism spectrum disorders. Autism, 14(1), 9-28. DOI:
- Pan, C.Y. (2011). The efficacy of an aquatic program on physical fitness and aquatic skills in children with and without autism spectrum disorders. Research in Autism Spectrum Disorders, 5(1), 657. DOI:
- Peeters, T. (2009). Autismul: teorie şi intervenţie educaţională [Autism: theory and educational intervention]. Iaşi: Polirom.
- Pitetti K.H, Rendoff A.D, Grover T & Beets M.W. (2007). The efficacy of a 9-month treadmill walking program on the exercise capacity and weight reduction for adolescents with severe autism. Journal of Autism and Developmental Disorders, 37(6), 997–1006.
- Rapin, I., Wing, L. (1996). Preschool Children with Inadequate communication: Developmental Language Disorder, Autism, Low IQ. London: MacKeith Press.
- Secară, O. (2007). Creierul social: autism, neuroştiinţe, terapie [Social brain: autism, neuroscience, therapy]. Timișoara: Artpress.
- Seynhaeve I, Nader-Grosbois N & Dionne C. (2008). Functional abilities and neuropsychological dysfunctions in young children with autism and with intellectual disabilities. Alter - European Journal of Disability Research/Revue Européenne de Recherche sur le Handicap, 2(3), 230-252. DOI:
- Srinivasan, S. M., Pescatello, L. S., & Bhat, A. N. (2014). Current perspectives on physical activity and exercise recommendations for children and adolescents with autism spectrum disorders. Physical therapy, 94(6), 875-890. DOI:
- Stoelb, M., Yarnal R., Miles J., Takahashi T.N., Farmer J.E. & McCathren R.B. (2004). Predicting Responsiveness to Treatment of Children with Autism: A Retrospective Study of the Importance of Physical Dysmorphology. Focus on Autism and Other Developmental Disabilities, 19(2), 66-77. DOI:
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
15 August 2019
Article Doi
eBook ISBN
978-1-80296-066-2
Publisher
Future Academy
Volume
67
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-2235
Subjects
Educational strategies,teacher education, educational policy, organization of education, management of education, teacher training
Cite this article as:
Rabolu*, E., & Toma, Ș. (2019). Physiotherapy In The Complex Rehabilitation Process Of Children With Autistic Spectrum Disorders. In E. Soare, & C. Langa (Eds.), Education Facing Contemporary World Issues, vol 67. European Proceedings of Social and Behavioural Sciences (pp. 1376-1382). Future Academy. https://doi.org/10.15405/epsbs.2019.08.03.169
