Non-Invasive And Minimally Invasive Prosthetic Therapies – Present Days Trajectories With Formative Character
Abstract
Introduction. Adhesive prosthetic therapies anchored in the registry of minimally invasive prosthetic therapies, in conjunction with the evolution of biomaterials and techniques, materializes in a viable solution for rehabilitation of reduced edentations, in the context of analysing local and loco-regional conditions of patients. The purpose of this study is to manage non-minimally invasive and minimally invasive prosthetic therapies in a clinically-technological vision based on a rapid, efficient algorithm adapted to the particularities of clinical cases. Material and method. Analysis of the criteria for the choice of noninvasive and minimally invasive therapeutic solutions for rehabilitation of partially reduced edentation by the wax-up method and various types of mathematical simulations in order to quantify the forces acting in the prosthetic field, individualized on different clinical situations. Results and discussions. A comparative study of the most commonly used and non-invasive methods of rehabilitation of various clinical situations of partial edentation has been carried out, with the help of mathematical simulations, resulting in the selection of the choice solution depending on the type of edentation, its location, the biomaterials and adhesives chosen, as well as the tensions involved. Conclusions. These non-invasive and minim-invasive therapies, which are predominantly anchored in the adhesive register, lead to successful results with a very good functional integration, their choice being in full agreement with a series of parameters represented by the etiology of edentation corroborated with the architecture of the edented ridge, and the type of occlusion.
Keywords: Prosthetic therapyoral rehabilitationadhesive therapypartially edentation
1.Introduction
Modern dentistry has seen the development of many new materials and techniques. Two major
developments lately are adhesion to dentin and stronger ceramic systems in the past. These technologies
are still relatively new and therefore have not passed the test of time; uncontested scientific evidence is
rare. The dentist is left with the presumption of trying to make clinical decisions based on scientific research
and still be able to offer his or her patients the latest materials and techniques. The key to making a decision
is a good understanding of the limitations and clinical indications of these new materials as well as the use
of correct techniques. Dentists must also take into account basic biomechanical principles and be aware of
the information provided by companies with extensive commercial influence.
Fractured plate generally appears as an aesthetic defect of minor importance and is easily corrected
by polishing or intraoral repairs; often goes unnoticed by the patient. For this reason, the resistance rates of
zirconium fixed dental prostheses and ceramic-metallic restorations are estimated to be equivalent (97-99%
over five years) (Gupta, Tandon, & Prabhu 2002; Whitmore, 2002; Christensen, 2004).
The greatest number of complications resulting from the use of zirconium oxide in prosthetic
treatments occur in fixed partial prostheses or decks. Current literature has identified numerous clinical
trials in which the cohesive fracture of plated material is the main and most common defect. However, there
are some controversies about the frequency of this mechanical failure as a result of variations in the
variables analysis from different studies. Regarding the mechanical behaviour of fixed prosthetic
restorations, the most important requirement is that they resist masticatory forces without fracture..
2.Problem Statement
The search for more resilient and lasting aesthetic restorations has been ongoing since the inception
of dentistry. Currently, dentists are working to combine ease of preparation and application with acceptable
aesthetics and predictable clinical longevity in a manner that enhances the efficiency and economy of the
dental office. In balancing the functional performance of a material with today's high aesthetic standards,
dentists often have to give up a certain amount of aesthetic concerns in order to gain more resistance and
durability (Holt & Drake, 2008; Ravinett, 1965; Hebel, Gajjar, & Hofstede, 2002).
Along with these philosophical options, there is often contradictory information on the best way to
use and handle these new materials and techniques - whether or not they are burly or not, bamboos or not,
photopolymerisation or self-curing, cement or glue? (Thilander et al., 2001; Edelhoff & Sorensen, 2002;
Goodacre, Bernal, Rungcharassaeng, & Kan, 2003).
Over the past few years, in terms of indirect aesthetic materials such as lithium disilicate and
zirconia have offered the profession higher degrees of resistance and aesthetics.
3.Research Questions
In order to have a pertinent study on an issue that is anchored in the reality of the immediate dental
practice it is necessary to be able to answer a series of questions:
1. In these clinical situations can we approach minimal and non-invasive therapies?
2. What are the criteria for long-term stability of these therapies?
3. To what extent do the clinical particularities and type the chosen biomaterial influences the
ultimate therapeutic success?
4.Purpose of the Study
The purpose of this study is to manage non-minimally invasive and minimally invasive prosthetic
therapies in a clinically-technological vision based on a rapid, efficient algorithm adapted to the
particularities of clinical cases.
5.Research Methods
Analysis of the criteria for the choice of non-invasive and minimally invasive therapeutic solutions
for rehabilitation of partially reduced edentation by the wax-up method and various types of biomechanic
simulations in order to quantify the forces acting in the prosthetic field, individualized on different clinical
situations. The study lot was represented by a number of 50 patients treated within the practical stage of the
final years of study of the Faculty of Dental Medicine, Iasi, students. The patients were diagnosed with
frontal and frontal – lateral reduced edentation and the therapeutic option used for these pathological entities
was represented by adhesive methods: bounded bridges and minimally invasive methods. Another research
direction approached was represented by the comparative analysis of the flexibility degree of various types
of biomaterials used. The test were made on a Textenser mechanical trials equipment. The data were
collected using MS Excel, the statistical processing was performed in SPSS 20.0 and the charts were
generated also in Excel.
6.Findings
A comparative study of the most commonly used and non-invasive methods of rehabilitation of
various clinical situations of partial edentation has been carried out, with the help of mathematical
simulations, resulting in the selection of the choice solution depending on the type of edentation, its
location, the biomaterials and adhesives chosen, as well as the tensions involved.
Figure
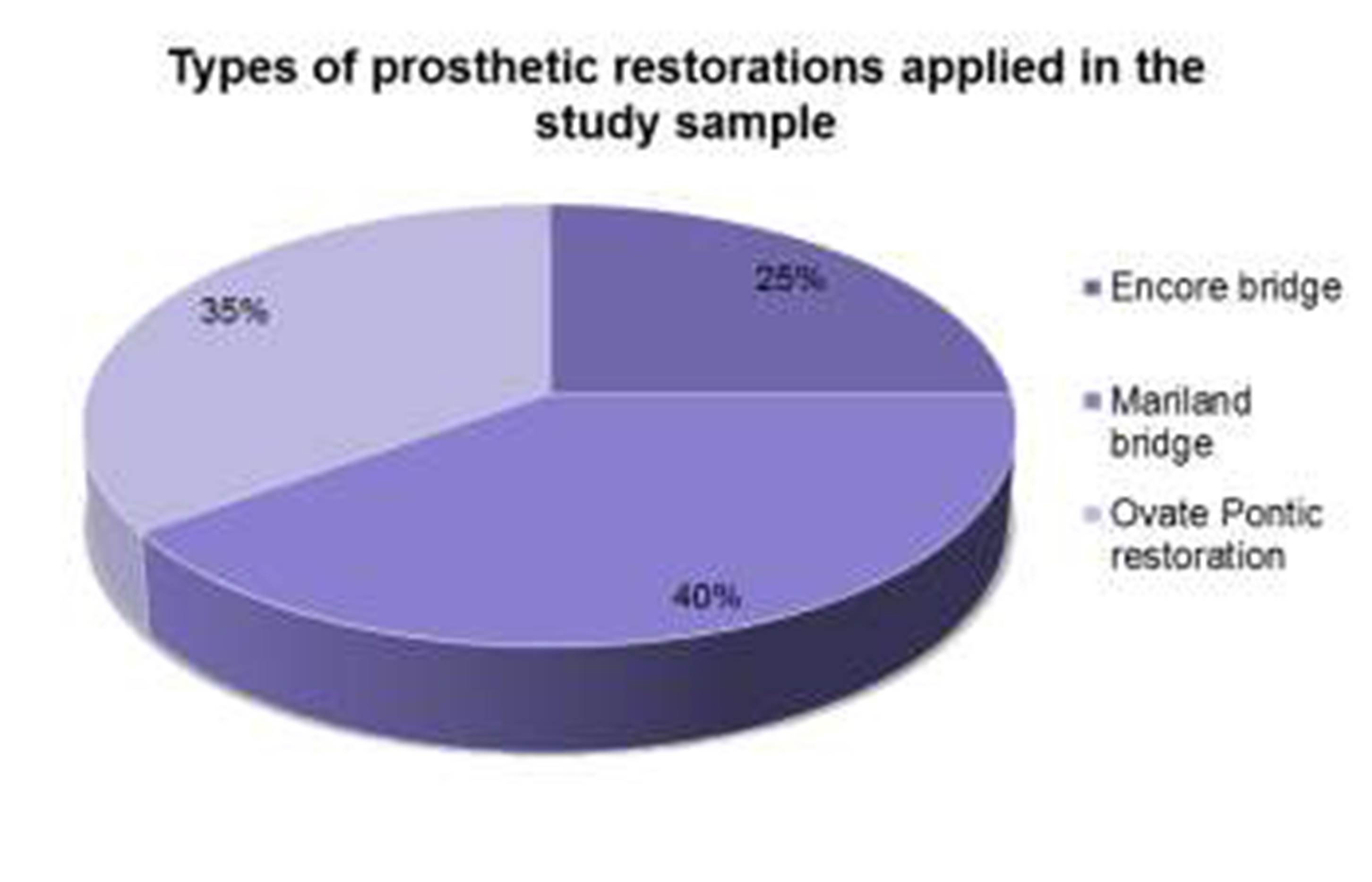
Regarding the prevalence of types of restorations analyzed, we remark a percentage of 40 % for
Mariland bridge, a percentage of 35% for pontic ovate restorations returning them a percentage of 25% for Encore Bridge.
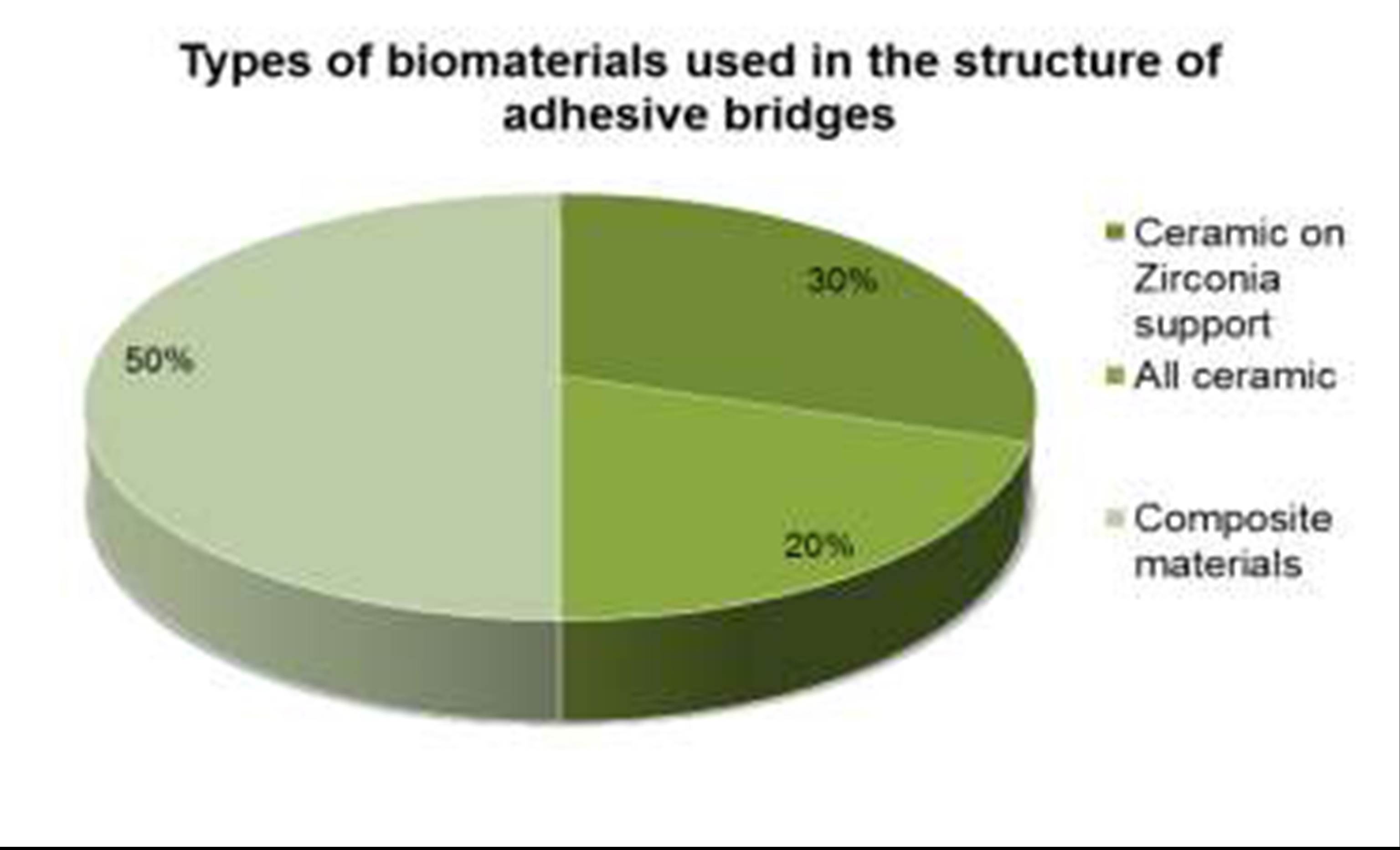
Regarding the type of biomaterial involved in adhesive and minimally invasive restorations,
illustrated in Figure
restorations in ceramic on zirconium, in proportion 30%, of the whole ceramic being distributed a
percentage of 20%. Figure
of frontal and frontal-lateral edentulous, followed by congenital causes, 27%, periodontitis 18%, and
orthodontic extraction, 8%.
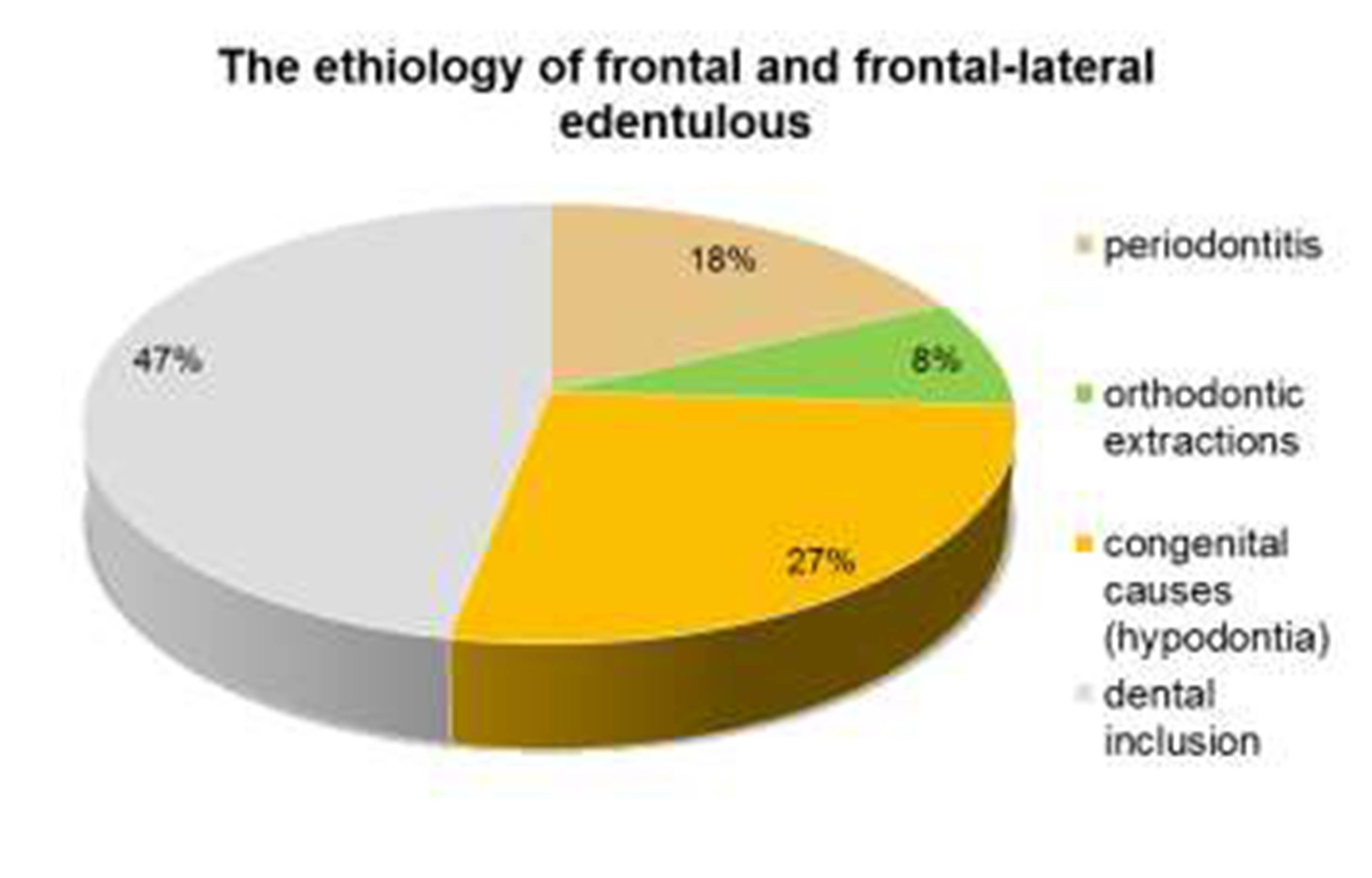
Significant implications for the choice of the therapeutic solution chosen from the regression of
minimally invasive adhesives rests on the etiology of the edentation, at the frontal and frontal-frontal level,
frequent clinical situations where the therapeutic indications refer to the curved bridges, the minimally
invasive restorations, whose characteristics must cover the aesthetic binomial -functionality.
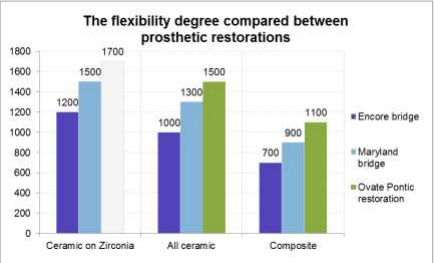
The degree of flexibility of prosthetic restorations, illustrated in Figure
for therapeutic long-term care, which must be correlated with the parameters that characterize the odonto-
periodontal support, the type of occlusion of the patient, and the biomechanical behavior of the chosen type
of restoration.
In the formative aspects, a particularly important direction is given to the implementation of all the criteria
for choosing the therapeutic solution of choice, represented by the practical applications.
A representative clinical case is the application of a collapsed bridge at level 24, applying the two
extensions at levels 23 and 25. The noninvasive structure of the adhesive bridge is shown in Figure
Particularly important aspects of the clinical algorithm are the application of acid to the oral face of
canine and second premolar, on the surface to be applied to the second extension of the bridge, followed
by the spraying, the application of the adhesive, who was polymerized 20s, then a dual cement resin will
be applied.The clinical algorithm and final aspect of adhesive bridge are illustrated in Figure



Another clinically representative case of the problem addressed is the rehabilitation of an interstellar
edentation at level 24, rehabilitated by a fixed ceramic restoration on zirconium, which involved limiting
preparations as soon as the biological criterion prevailed.


7.Conclusion
These non-invasive and minim-invasive therapies, which are predominantly anchored in the
adhesive register, lead to successful results with a very good functional integration, their choice being in
full agreement with a series of parameters represented by the etiology of edentation coroborated with the
architecture of the edented ridge, the type of occlusion with the 2 essential aspects: static and dynamic, as
well as the other features of each clinical case, thus leading to targeted and individualized therapeutic
approaches.
References
- Christensen, G. J. (2004). Post concepts are Am Dent Assoc. , 135(9), 1308-1310, changing. J
- Edelhoff, D.Sorensen, J. A. (2002). Tooth structure removal associated with various preparation designs for anterior Prosthet Dent.,. https://www.ncbi.nlm.nih.gov/pubmed/15493395. , 87(5), 503-509, teeth. J
- Goodacre, C. J.Bernal, G.Rungcharassaeng, K.Kan, J. Y. (2003). Clinical complications in fixed Prosthet Dent. , 90(1), 31-41, prosthodontics. J
- Gupta, K.Tandon, S.Prabhu, D. (2002). Traumatic injuries to the incisors in children of South Kanara district: A prevalence Indian Soc Pedod Prev Dent.,. http://www.jaypeejournals.com/eJournals/. , 20(3), 107-113, study. J
- Hebel, K.Gajjar, R.Hofstede, T. (2000). Single-tooth replacement: Bridge vs implant-supported Can Dent Assoc. , 66(8), 435-438, restoration. J
- Holt, L. R.Drake, B. (2008). The Procera Maryland Bridge: A case Esthet Restor Dent.,. https://www.ncbi.nlm.nih.gov/pubmed/11040527. , 20(3), 165-171, report. J
- Ravinett, S. (1965). Factors influencing fixed partial dentures for Prosthet Dent.,– 888. , 15(5), 880-, adolescents. J
- Thilander, B.Odman, J.Lekholm, U. (2001). Orthodontic aspects of the use of oral implants in adolescents: A 10-year follow-up J Orthod.,. https://www.ncbi.nlm.nih.gov/pubmed/11890067. , 23(6), 715-731, study. Eur
- Whitmore, K. (2002). General dentistry: The Maryland Bridge revisited: Of wings and webbed health and dental practice management https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5030500. , feet. Oral
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
15 August 2019
Article Doi
eBook ISBN
978-1-80296-066-2
Publisher
Future Academy
Volume
67
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-2235
Subjects
Educational strategies,teacher education, educational policy, organization of education, management of education, teacher training
Cite this article as:
Gradinaru, I., Hurjui*, L. L., Dascalu, C. G., & Antohe, M. –. E. (2019). Non-Invasive And Minimally Invasive Prosthetic Therapies – Present Days Trajectories With Formative Character. In E. Soare, & C. Langa (Eds.), Education Facing Contemporary World Issues, vol 67. European Proceedings of Social and Behavioural Sciences (pp. 1213-1219). Future Academy. https://doi.org/10.15405/epsbs.2019.08.03.149
