Abstract
Introduction: Elderly people suffer from balance disorders that can, unfortunately, lead to moderate or even severe injuries that limit their mobility and reduce their independence. Worldwide, it is estimated that 2.9% of patients over 60 years of age and 3.8% over 75 years of age present disturbances of balance, as a result of vestibular hypofunction or a combination of deficiencies in the vestibular, visual and somatosensory systems. Purpose: Through this paper, we intend to highlight the importance of early evaluation of vestibular disorders and the efficiency of using the Multitest-Equilibre Framiral Platform in combination with the PosturoPro software. Both methods can make a significant difference for elderly people with balance disorders, both in assessing and recovering them. Subjects and methods: The Multitest-Equilibre Framiral Platform is used for the evaluation and rehabilitation of 20 patients aged 60 to 80 years (10 women and 10 men) in a rehabilitation clinic. The subjects were evaluated in both static and dynamic scenarios, by measuring the following indicators (prior to and right after rehabilitation): proprioceptive, visual and vestibular ones, related to various (pendulous, saccadic or optokinetic) stimuli. Results and conclusion: The results obtained after 5-8 sessions of dynamic multisensory rehabilitation on Multitest-Equilibre Framiral Platform have clearly demonstrated its usefulness in obtaining a fair and objective evaluation of balance disorders and also its effectiveness in restoring balance. Vestibular rehabilitation has reduced the risk of falling, stabilised balance, retrained the proprioceptive system and the gait and restored independent living.
Keywords: Rehabilitationbalance disorderelderly peopleMultitest-Equilibre Framiral Platform
Introduction
Elderly people suffer from balance disorders that, unfortunately, can lead to moderate or severe injuries, can limit their mobility and can reduce their independence. Worldwide, it is estimated that 2.9% of patients over 60 years of age and 3.8% of patients over 75 years of age present disturbances of balance, as a result of vestibular hypofunction or a combination of deficiencies in the vestibular, visual and somatosensory systems (Herdman, 2007)
Patients with vestibular disorders often complain of balance disorder, spatial orientation problems or dizziness related to position or movement. These early symptoms are often accompanied by secondary symptoms which may have a negative impact on the quality of their daily life. Secondary symptoms include a decrease in muscular strength, a range-of-motion impairment, a cervical or shoulder tension which may lead to headaches and muscle fatigue. (Shumway-Cook, 2008) Balance disorders associated with dizziness can be caused by multiple factors, such as inner ear dysfunction, cardiovascular or neurological disease, cervical arthritis, imbalanced nutrition, visual acuity problems, or environmental factors and lifestyle (Alexander, Rivara, & Wolf, 1992).
Therefore, an important component in restoring the functional independence of the elderly is the management of patients through vestibular rehabilitation therapy. Recently, more and more methods and innovative techniques have been found and, with their help, balance and stability have been restored, and the proprioceptive system has been retrained without side effects.
Problem Statement
The functional rehabilitation of balance in elderly people, a vital condition for an independent life at this age, is the topic we have approached in this article.
Research Questions
In this study, we intend to check whether the Multitest-Equilibre Framiral Platform, such a modern method of research, could be at least as effective as the other methods of assessment and rehabilitation of balance.
Purpose of the Study
In this paper, we intend to highlight the importance of early evaluation of vestibular disorders and the efficiency of using the Multitest-Equilibre Framiral Platform combined with the PosturoPro software. These two methods can have a significant impact on elderly people with balance disorders, both in assessing and recovering them.
We have conducted this study starting from the hypothesis that vestibular or proprioceptive rehabilitation by multisensory stimulation can reduce, via the Multitest-Equilibre Framiral Platform, postural instability and improve balance.
Research Methods
The experiment was performed in a rehabilitation clinic in Bucharest, over a period of 8-10 weeks, on a group of 10 men and 10 women aged between 60 and 80, who agreed to participate in our study; we also received their consent to interpret and process the data and disseminate the obtained results. All patients showed various forms of balance disorders associated with vestibular dysfunctions. The Multitest-Equilibre Framiral Platform (Figure

Through a mathematical analysis of the stabilometric signal (Figure
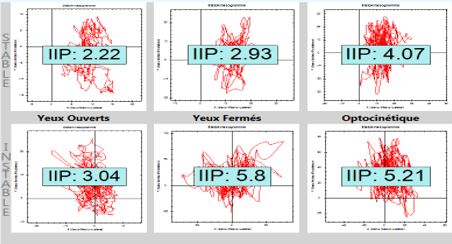
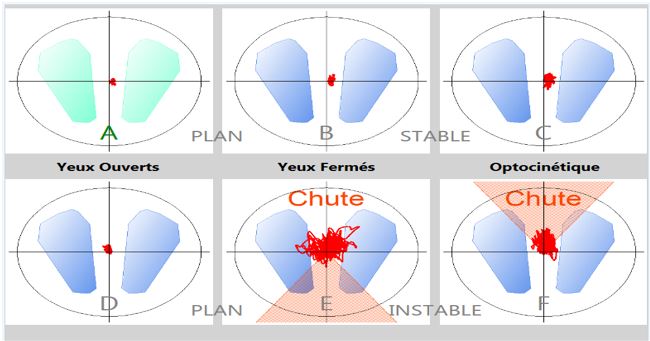
The test was performed in a static mode, in three sequences of 30 seconds each: 1. open-eyes mode (YO), during which the subjects had to maintain their balance by focusing on a visual target located 2.5 meters straight in front of them; 2. closed-eyes mode (YF), 3. open-eyes mode, focusing on the target, but in darkness, with an optokinetic stimulus. (Figure
After the initial assessment, patients were recommended 5 to 8 Dynamic Vestibular Rehabilitation Therapy sessions with Multitest-Equilibre Framiral Platform, an important tool in the rehabilitation of the elderly. Of all rehabilitation programs available on the Platform, only the fall prevention program and the impulse re-education program were selected for this research.
The fall prevention program was set for 5 minutes and was performed on an inclined plane and directions preset by the therapist (anterior-posterior, left-right), with a pause of 4 seconds when changing the direction (latency phase). During this exercise, the patient follows the instructions: eyes closed, eyes open, focusing on a target or optokinetic stimulus. The impulse re-education program uses the platform on the unstable mode, with impulses set by the therapist at the pressure of 1 bar, in the left-right and anterior-posterior directions, and with a latency of 3 seconds. As in the previous program, the time dedicated for this one was 5 minutes, and the subjects followed the therapist’s instructions (eyes open, eyes closed).
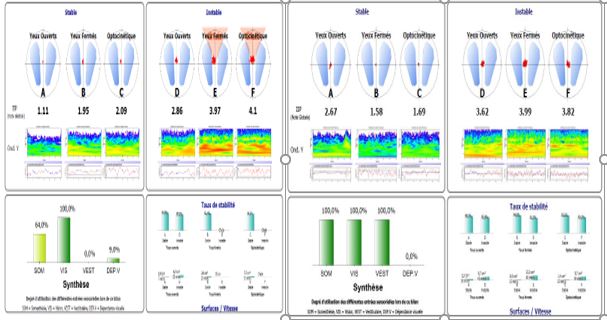
At the end of the 5/8 rehabilitation sessions, the tests (final assessments) were redone and the obtained data were statistically processed. (Figure
Findings
The results obtained at the end of 5-8 sessions of dynamic multisensory rehabilitation on the Multitest-Equilibre Framiral Platform have clearly demonstrated both its usefulness in doing a fair and objective evaluation of balance disorders and its effectiveness in restoring balance.
The statistical analysis proves a significant difference between the average age for men (75.60 years) and the average age for women (67.6 years); this means that, for men, balance disorders may appear later. At a complete group scale, for both women and men, the average age is 71.6. (Table
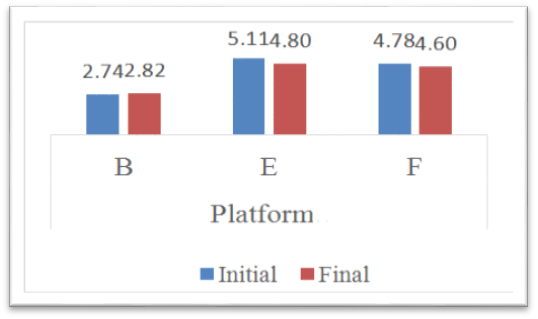
For women, at the final assessment, the Postural Instability Index (PII) (Table
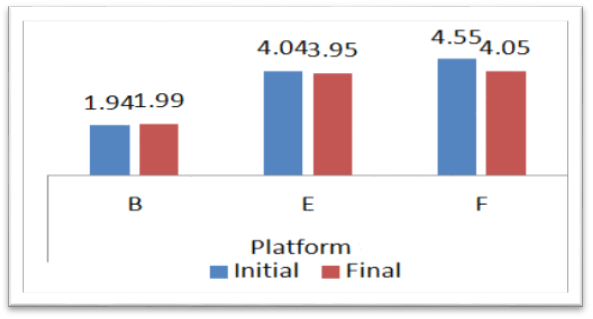
For men, at the final assessment, the Postural Instability Index (PII) (Table
Comparing the two groups (men and women), we could highlight the following: in both men and women, at the final assessment, the Postural Instability Index for condition B (stable platform, eyes closed) increased by 0.07, from 2.34 units to 2.41. The Postural Instability Index for condition E (unstable platform, eyes closed) decreased by 0.19, from 4.57 units to 4.57. The average PII for condition F (platform unstable, eyes open and optokinetic stimulation) decreased by 0.34, from 4.66 to 4.32. (Figure
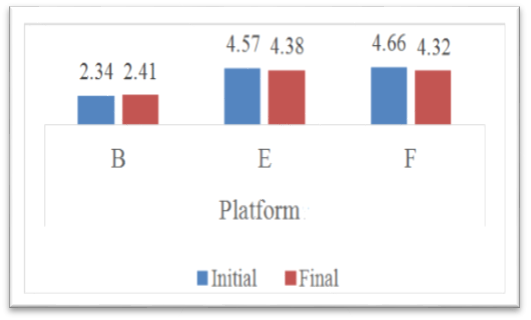
For better statistical representation, we compared the average between initial and final results for PII by the Wilcoxon Nonparametric Test (“b” based on negative ranks and “c” based on positive ranks) and we have found out that, for both men and women, there are no statistically significant differences between the initial and final values of the postural instability indexes for any of the conditions B, E or F. In all these cases, the significant p-value threshold > 0.05, Z-values belonging to the interval (-1.96, 1/96) (Table
Also, we have compared the average final results of PII, for men and women, by the Mann-Whitney Nonparametric Test and we can prove a significant difference between men and women for Platform B and E conditions, where p <0.05 and Z-statistic values are lower than the -1.96 threshold. Regarding Platform F, differences between men and women are not statistically significant, p> 0.05 for Z = -1.285 (Table
In most cases, the initial assessment for the elderly with balance disorders shows high postural instability indexes for condition B. After the rehabilitation program, due to the neuronal plasticity, the PII for condition B has improved, increasing its value. Training the patients in dynamic conditions (E & F) shows that they adjust their responses in the static condition in the same way they respond to dynamic conditions. The structural and functional neuronal reorganization reveals an anticipatory and compensatory postural strategy, which has been created in order to control postural responses. All this can be explained by the phenomenon of neuronal network plasticity. (Lacour & Bernard-Demanze, 2015)
For the initial assessment in dynamic conditions, the values for E and F may point to a visual dependence or multisensory integration disorganization in the patient. Both E and F dynamic conditions are the equivalent of daily activities. After rehabilitation, the values for E and F conditions decreased, which means there has been improvement due to anticipated postural adjustments.
These results emphasise an improvement of the postural instability indexes, irrespective of the subjects’ age or gender. We take into account the improvements, but, because there are no significant differences between men and women in the initial and final values, the study requires a larger number of participants and a shorter age sample.
Conclusion
The Platform has clearly demonstrated its usefulness in assessing and rehabilitating balance disorders in the elderly, through the manipulation of the obtained data. All postural instability indexes allowed having a real-time quantification of the rehabilitation progress for our subjects. There were positive changes reported in the symptomatology of patients with balance disorders, which improved their gait and postural stability. Due to vestibular rehabilitation, part of a multisensory approach to balance rehabilitation in the elderly, the dynamic functions were restored through the process called “sensory substitution”. Visual and somatosensory inputs developed through the manipulation of visual cues (eyes closed, eyes open, optokinetic stimulation) and balance control (stable or unstable surfaces). This dynamic platform provided predictable perturbation which led, on the one hand, to a feedback mechanism to control posture, and on the other hand, to a feed-forward mechanism which allowed patients to anticipate the responses of postural muscles in order to prevent balance perturbation. (Horak, 2010)
In conclusion, vestibular rehabilitation, a multisensory integration process, has reduced the risk of falling, stabilised balance, retrained the proprioceptive system and the gait and enabled the elderly with balance disorders to live independently again.
References
- Alexander, B. H., Rivara, F. P., & Wolf, M. E. (1992). The cost and frequency of hospitalization for fall-related injuries in older adults. American Journal of Public Health, 82(7), 1020-1023.
- Herdman, S. J. (2007). Vestibular rehabilitation (3rd ed.). Philadelphia: F. A. Davis Company.
- Horak, F. B. (2010). Postural compensation for vestibular loss. Restorative Neurology and Neuroscience, 28(1), 57-68.
- Lacour, M., & Bernard-Demanze, L. (2015). Interaction between vestibular compensation mechanisms and vestibular rehabilitation therapy: 10 recommendations for optimal functional recovery. Frontiers in Neurology, 5: 285. doi: 10.3389/fneur.2014.00285
- Shumway-Cook, A. (2008). Vestibular rehabilitation – An effective, evidence-based treatment. Vestibular Disorders Association, Publication no. F-7, 1-8.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
16 February 2019
Article Doi
eBook ISBN
978-1-80296-054-9
Publisher
Future Academy
Volume
55
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-752
Subjects
Sports, sport science, physical education
Cite this article as:
Neacsu, G., Apostu, M., & Pavel, R. (2019). Modern Approaches To Rehabilitation Of Balance Disorders In Elderly People. In V. Grigore, M. Stănescu, M. Stoicescu, & L. Popescu (Eds.), Education and Sports Science in the 21st Century, vol 55. European Proceedings of Social and Behavioural Sciences (pp. 482-489). Future Academy. https://doi.org/10.15405/epsbs.2019.02.60
