Abstract
Children with type 1 diabetes mellitus (T1DM) incorporate the uniqueness concept of the World Health Organization related to the reshaping of disability, as a limitation in performing activity, not simply as a medical condition or a certain defect that an individual might have. This topic is relevant for the specialists in sport, social and medical sciences, given the metrics which emphasise that Europe has one of the highest incidence rates of T1DM, with more than 21,000 new cases recorded every year. The study aims to underline the general framework for encouraging social inclusion and equal opportunities in grassroots sport for children and teenagers with insulin dependency, an idea which is widely provided by the European policies. Research methods: EU policies and relevant reference analysis, historical method and observation. The EU health and sport agenda interconnect, providing ruling to enhance physical activity participation for all people with limited condition. Concerning the T1DM children, the social model strongly acknowledged by the European policies involves participation in joint educational activities, including physical activities delivered in a friendly inclusive approach, with customised content and a totally risk-free performed effort. School has a major role in raising awareness of peers on the equal opportunities and positive attitudes that have to be promoted during classes and extracurricular activities, concerning the chronic disease approach in mainstream education. Recently, examples of good practice promote sports and social inclusion for T1DM either through Erasmus+, the Sweet Initiative within the International Diabetes Federation, or under different European framework cooperation programmes.
Keywords: European policiessocial modelinsulin dependency
Introduction
The last decades have provided scientists, academics and practitioners with new paradigms and approaches to children with health limitations, as a resource for creating worldwide policies in the educational, medical and social areas.
Children with type 1 diabetes mellitus (T1DM) incorporate the uniqueness concept of the World Health Organization (2001) related to the reshaping of disability, as a limitation in performing activity, not simply as a medical condition or a certain defect that an individual might have.
This topic is relevant for the specialists in sport, social and medical sciences, given the metrics which emphasise that Europe has one of the highest incidence rates of T1DM, with more than 21,000 new cases recorded every year. Certain areas, such as Sardinia, Finland, Sweden and Norway, are even more affected by this chronic condition, due to factors that are not clearly argued. In Romania, statistics show that there is an upward trend in juvenile-onset diabetes, with a 10.6% increase rate since 2002 to date. From a shallow perspective, one might consider that 3,000 cases in Romania is not an alarming figure; however, in the next two decades, the number is expected to reach more than 5,000-6,000 cases, each of them requiring complex healthcare measures, specialised medical staff and complementary educational framework for parents, teachers, coaches, therapists and the wider public (Șerban, 2015).
In some recently published studies, the International Diabetes Federation (IDF) (2018) has identified major disparities in accesing healthcare system and medical devices across European countries. In less developed regions, the burden of managing diabetes is mostly felt by families who have to handle by themselves the diagnosis, therapies, diet and adapted physical activities. In Romania, for example, the standard of care is limited to providing fingerstick glucose testing and insulin therapy, while in other countries, children with diabetes are also provided with Continuous Glucose Monitoring Systems (CGMS) and wireless insulin pumps.
In the European Union (EU), there are certain intitiatives, such as the Joint Action on Chronic Diseases, with workpackages specially designed for diabetes, and the Action Plan on Childhood Obesity, both stressing the importance of a cross-sectoral policy approach, as a response to this health limitation. Promoting a healthier lifestyle for T1DM children is a key contributor to their quality of life and long-term social integration. In addition, EU policies support the idea of promoting regular exercise for all chronic diseases, as an efficient tool for health and social inclusion.
Problem Statement
The child with insulin dependency
The general framework of approaching T1DM children includes at least three interconecting pillars, according to relevant literature (Sherrill, 2004): celebrating differences between individuals, providing physical activity experiences and striving for social inclusion.
Generally known as a chronic disease, T1DM is an incurable health condition with early onset, described by a pancreatic failure in providing insulin. This type of diabetes is managed by daily insulin injections or pump therapy, through glucose monitoring, careful diet and individualised physical exercise regimen, according to the (ADA) (American Diabetes Association 2018). Despite the clinical symptoms, children with T1DM have often similar fitness and motor profiles to those of their healthy peers, being able to engage in various activities, both grassroots and performance sports.
Due to uncontrollable hyper- or hypoglycaemic fluctuations, the T1DM child is exposed to further medical complications, social isolation, school absenteeism and poor self-esteem.
Nowadays, it is an argued fact that physical exercise is beneficial for juvenile diabetes mellitus. Although the child usually experiences fatigue when performing prolonged and strenuous effort, the teacher, coach or therapist has to prepare backup solutions for low intensity tasks, as well as opportunities for rest. As T1DM can exhibit various secondary health conditions, the practitioner has to be aware of the medical history of the child, by meeting their parents and the medical professionals before planning physical activity (American Diabetes Association 2018).
Sport is generally regarded as a way to develop and self-express for every child with special needs. Being essentially a social experience, physical activities are recognised as a resource of fostering interpersonal skills in a friendly environment, gathering T1DM children next to peers, schoolmates, community members and family. One of the methods to nurture children’s confidence and self-esteem is to encourage them to discover the world and themselves through the sport experience, which allows them to learn who they are and what they might become. The sense of belonging, of worthiness, perceived competence, self-acceptance and uniqueness are illustrative for the physical activity and sports values. So, each parent and educator should stimulate the physical participation of children in all kinds of educational programs.
T1DM children and teenagers are difficult to manage as sports participants, because they must perform all activities under the strict monitoring of blood glucose fluctuations. Keeping in mind that T1DM children and teenagers usually face the risk of hypoglycaemia, practitioners should deliver various appropriate physical exercise contents, so that the child remains within safe glycaemic values. This objective is feasible only by using CGMS as a higher standard of care device, which helps the educator to set the exercise intensity according to real-time blood glucose monitoring (Urzeală & Vlăiculescu, 2015).
One of the basic rules required to ensure risk-free sports practice is “Safety comes first!” So, teachers and coaches will manage the specific health risks during exercise at a level considered acceptable for that sport activity (Bota & Teodorescu, 2007). T1DM children and teenagers should be encouraged to participate in risk-free physical exercise programs, camps and trips, due to the use of CGMS, gradually giving up parental supervision.
Research Questions
How to raise awareness on the characteristics and sports practice of T1DM children, considering the priority of EU policy in the health and social inclusion areas?
Purpose of the Study
The aim of this study is to underline the need to encourage social inclusion and equal opportunities in grassroots sport for children and teenagers with insulin dependency, an idea which is widely provided by the European policies.
Research Methods
The research methods used were:
analysis of EU policies referring to chronic diseases, as a general framework for implementing social models in the area of physical activities addressed to T1DM children;
analysis of relevant references regarding health, sports and the social inclusion of T1DM children;
observation of T1DM children during physical activities performed on a regular basis, as a support for identifying the best models, practices and theoretical paradigms to be implemented by professionals (physical education teachers, coaches, therapists);
historical method, in terms of analysing and interpreting the EU legislation on disability, in order to identify the trends and the systemic strategy for implementing it.
Findings
EU policies regarding social inclusion of T1DM children
One of the key documents emphasising the fundamental right of a child to access opportunities to learn and benefit from regular education, taking into account diversity and the acceptance of an inclusive framework, was the Salamanca Statement and Framework for Action on Special Needs Education (UNESCO, 1994). This document established a set of beliefs delivered as part of the general teaching and learning practice, according to some core principles which we tailored for the T1DM child (Table
EU policies regarding sport and disability were delivered under the United Nations (UN)
As children and teenagers with insulin dependency are considered, in some European countries, as disabled, the
Another relevant European document was the
Regarding the sports practice of children with insulin dependency, we mention the
Another important EU ruling was linked to the
It is widely known that diabetes is strongly connected to overweight problems, so another topic-related EU document is the
As a continuum, the EU set the
The social model in chronic diseases
The philosophy embraced by different authors reveals at least three models for disability, each of them reflecting a certain approach to the concept of disability, its perception, the terminology used and the type of service delivered (Sherrill & Yilla, 2004).
The medical model, also known as the deficit model, links the disability to the individual physical body, mostly addressing the weaknesses and impairements of the individuals. This approach is often subjected to criticism by the advocates of social inclusion, who argue that a person cannot be limited to his/her dysfunctions and cannot adapt him/herself only by medication or adaptive technologies (Brisenden, 1986). Speaking about T1DM children, the medical approach is mainly directed to the use of CGMS and insulin pump in order to manage blood glucose fluctuations. Still, the quality of life for a child with insulin dependency involves more factors, like the educational, social and sports-oriented ones, so that he/she can perceive him/herself as a complete person.
The social minority model has started to spread in the 80s, based on the idea that disability is just a difference, neither good nor bad, and represents only a part of the whole person. Some of its advocates (Nixon, 1989; Oliver, 1990) claim that a disability is caused by the way society relates to the individual rather than by the person’s dysfunction or limitation. In contrast with the medical model, the social model is about the personal experience of disability and how to develop inclusive ways of living. The focus is shifted from impairement to disability, the latter referring to disabling social environmental and attitudinal barriers encountered by the individual (Crow, 1996).
The social model narrative overlooks social exclusion and marginalisation, the lack of confidence and self-esteem, the limited physical health, bringing to the surface inclusion and friendship, an active lifestyle, a reinforced self-concept and enhanced autonomy (Hassan, Dowling, & McConkey, 2014). These outcomes have to be generated by the social majority, and its social action consists in removing barriers and including disabled persons in all areas of social life. Basically, society creates the problem and it is its responsibility to remove all roadblocks between individuals. Disability is a social construct created by the dominant majority population, which also applies to sports practice, generically considered as an activity exclusively for highly-trained healthy people. Thus, exclusion seems like a common way to handle the differences between individuals.
Concerning T1DM children, the social model involves participation in joint educational activities, including physical activities delivered in a friendly-inclusive approach, with customised content and a totally risk-free performed effort. Generally speaking, school has a major role in raising awareness of peers on the equal opportunities and positive attitudes that have to be promoted in classes and extracurricular activities, concerning the chronic disease approach in mainstream education.
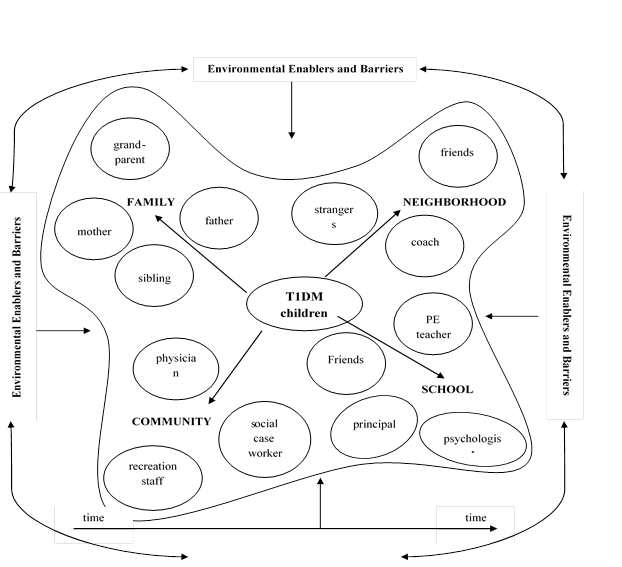
The ecological model emphasises the interactions between individuals and their social and physical environment. Both persons with chronic diseases and their healthy peers have to get involved in promoting changes that occur via a collaborative and systematic effort to remove barriera and enhance enablers. Specialists have asserted that social transformation can be attributed to both “participatory and directive change cycles” (Hersey, Blanchard, & Johnson, 2001). In the context of EU policies, leaders shape attitudes and behaviours in a top-down system by a directive change cycle, while individuals, small groups and NGOs use a bottom-up approach for reaching the same outcomes.
Recent literature has addressed the topic of ecological pathways towards social inclusion, starting from Bronfenbrenner’s ecological model for individual development (Overmars-Marx, Thomese, Verdonschotem, & Meininger, 2013). In this context, social inclusion is an outcome of the way in which individual, interpersonal, organisational, community and socio-political variables act like enablers or barriers, in an ecological perspective (Figure
Best practice examples
Some projects that promote sports and social inclusion for T1DM are:
The Erasmus+ Not-for-profit Sport Events project, which has been implemented since 2017 by the Spoleto Municipality, in Italy, entitled “Diabetics runners and cyclists for more sport for all in Europe – SportGiveChance”. The central theme of this project is to organize a European sports event of running, bike ride and hand-bike, involving diabetics and disabled athletes, to raise awareness of sport and physical activity in promoting health, wellbeing and social inclusion, during a week of sports activities. The participants were 320 athletes with diabetes from 16 European countries and 700 from Italy.
World Diabetes Tour, which organises leisure activities only for T1DM individuals from Slovenia, France, Spain, Italy, Germany, Israel, Greece, Norway and other countries worldwide, consisting in trekking, snow-racquets walking, canoeing, paddling and yoga.
An example of good practice was represented by the Camp-D Germany, having as a motto “The future belongs to me”. This camp was open to young people with T1DM aged between 16 and 25 years, residing in Germany, Austria and Switzerland. The program included sports activities and thematic workshops delivered by medical professionals and caregivers.
Since 2015, the SWEET project has been organising the T1DM Youth challenge program addressed to young people with diabetes from SWEEET centers in Europe (France, Spain, Italy, Czech Republic, Portugal) and not only. The program usually involves 11-12 young people in 5 days of trekking. SWEET carries out under the aegis of the International Diabetes Federation.
Evidence shows that around 30,000 T1DM children have attended diabetes camps in North America and over 180 diabetes camps have been organised every year in the rest of the world. The aim of this kind of camps is to facilitate a traditional camping experience in a medically safe environment, based on increased physical activity and food control (American Diabetes Association 2018).
The Juvenile Diabetes Research Foundation and Diabetes Education & Camp Association are recognized for working successfully to educate and to support T1DM children and their families in the US, having international affiliations in Australia, Canada, Denmark, Israel, Netherlands and the United Kingdom.
In Romania, Yuppi Camp Association, in the framework of the Swiss-Romanian Cooperation Programme, organised camps for children with several chronic diseases (430 participants). The sports activities foreseen for the participants were: archery, rowing, equestrian, climbing.
Support for Diabetes Association (SDA) is specialised in the camps for T1DM young people (almost 200 participants) organised in the last 5 years. This a ssociation organises camps exclusively for children with T1DM, accompanied by their parents.
Unlike the above sport events/camps addressed solely to T1DM children and teenagers, we emphasise the importance of joint activities, which gather children with and without diabetes in socialising, playful, recreational physical activities.
Conclusion
Theoretical approaches and European examples of good practice have underlined the neccesity to implement a social inclusion framework and provide equal opportunities in grassroots sport for children and teenagers with insulin dependency.
The prevalent model regarding the disability, based on the European policies widely promoted in the last decades, is represented by the social minority approach, which gradually replaces the medical perspective.
Using the best practices addressed solely to T1DM children, there is a growing need to move forward, towards joint sport activities which gather children with and without diabetes in socialising, playful, recreational settings.
Creating and supporting transnational and cross-sectorial cooperation between international communities, national authorities and NGOs have proved to be an incentive for conceiving, implementing and assessing the policies addressed to T1DM children.
Acknowledgments
Both authors contributed equally to this study and should be considered as main authors.
References
- American Diabetes Association. (2018). Standards of medical care in diabetes – 2018. Diabetes Care, 41(Suppl. 1). Retrieved from https://diabetesed.net/wp-content/uploads/2017/12/2018-ADA-Standards-of-Care.pdf
- Bota, A., & Teodorescu, S. (2007). Exercițiul fizic în afecțiunile cronice. București: Editura Didactică și Pedagogică.
- Brisenden, S. (1986). Independent living and the medical model of disability. International Journal of Disability, Handicap and Society, 1(2), 173-178.
- Commission of the European Communities. (2007). White Paper on Sport. Retrieved from https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:52007DC0391&from=EN
- Council of Europe. (2017). Disability strategy 2017-2023. Retrieved from https://www.coe.int/en/web/disability/strategy-2017-2023
- Council of the European Union. (2013). Council recommendation of 26 November 2013 on promoting health-enhancing physical activity across sectors. Retrieved from https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32013H1204(01)&from=GA
- Crow, L. (1996). Including all of our lives: Renewing the social model of disability. Leeds: The Disability Press.
- European Commission. (2018). 2018 Commission work programme – key documents. Retrieved from https://ec.europa.eu/info/publications/2018-commission-work-programme-key-documents_en
- European Comission. (2014a). Europe 2020 Strategy. Retrieved from https://ec.europa.eu/info/business-economy-euro/economic-and-fiscal-policy-coordination/eu-economic-governance-monitoring-prevention-correction/european-semester/framework/europe-2020-strategy_en
- European Comission. (2014b). EU action plan on childhood obesity 2014-2020. Retrieved from https://ec.europa.eu/health/sites/health/files/nutrition_physical_activity/docs/childhoodobesity_actionplan_2014_2020_en.pdf
- European Commission. (2011). Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions – Developing the European Dimension in Sport. Retrieved from https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=COM:2011:0012:FIN:EN:PDF
- Hassan, D, Dowling, S & McConkey, R. (2014). Understanding sport and intellectual disability: An introduction. In D. Hassan, S. Dowling & R. McConkey (Eds.), Sport, coaching and intellectual disability (pp. 1-10). London: Routledge.
- Hersey, P., Blanchard, K. H., & Johnson, D. E. (2001). Management of organisational behaviours. Leading human resources. Upper Saddle River, NJ: Prentice Hall.
- International Diabetes Federation. (2018). Education – Best of IDF. Retrieved from https://www.idf.org/our-activities/education/best-of-idf.html
- Le Clair, J. M. (2011). Global organizational change in sport and the shifting meaning of disability. Sport in Society, 14(9), 1072-1093.
- Nixon, H. L. (1989). Integration of disabled people in mainstream sports. Adapted Physical Activity Quaterly, 6(1), 17-31.
- Oliver, M. (1990). The politics of disablement. London: Mc. Millan.
- Overmars-Marx, T., Thomese, F., Verdonschotem, M., & Meininger, H. (2013). Advancing social inclusion in the neighborhood for people with intellectual disability: An exploration of the literature. Disability and Society, 29(2), 255-274.
- Sherrill, C. (2004). Adapted physical activity, recreation and sport: Cross-disciplinary and lifespan (6th ed.). Boston: McGraw Hill Education.
- Sherrill, C., & Yilla, A. (2004). Celebrating differences, planning practical experience and striving toward inclusion. In C. Sherrill (Ed.), Adapted physical activity, recreation and sport: Cross-disciplinary and lifespan (6th ed.) (pp. 26-59). Boston: McGraw-Hill Education.
- Șerban, D. (2015). Criza din diabetul pediatric. Viața Medicală, 20(1270). Retrieved from http://www.viata-medicala.ro/Criza-din-diabetul-pediatric.html*articleID_10194-dArt.html
- UNESCO. (1994). The Salamanca Statement and Framework for Action on Special Needs Education. Retrieved from http://www.unesco.org/education/pdf/SALAMA_E.PDF
- United Nations. (2006). Convention on the Rights of Persons with Disabilities and Optional Protocol. (2006). Retrieved from http://www.un.org/disabilities/documents/convention/convoptprot-e.pdf
- Urzeală, C., & Vlăiculescu, M. (2015). Utilization of Continuous Glycemic Monitoring Systems and physical exercise in the diabetic child. In O. Roceanu (Ed.), Proceedings of the 11th International Scientific Conference eLearning and Software for Education, April 23-24, 2015 (Vol. 3, pp. 359-365). Bucharest: Carol I NDU. DOI: 10.12753/2066-026X-15-235
- World Health Organization. (2001). Disabilities. Retrieved from http://www.who.int/topics/disabilities/en/
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
16 February 2019
Article Doi
eBook ISBN
978-1-80296-054-9
Publisher
Future Academy
Volume
55
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-752
Subjects
Sports, sport science, physical education
Cite this article as:
Bota, A., & Urzeală, C. (2019). Social Model Perspective And European Policies Addressing Children With Insulin Dependency. In V. Grigore, M. Stănescu, M. Stoicescu, & L. Popescu (Eds.), Education and Sports Science in the 21st Century, vol 55. European Proceedings of Social and Behavioural Sciences (pp. 46-55). Future Academy. https://doi.org/10.15405/epsbs.2019.02.6
