Abstract
Patients are more likely to ask pharmacists than other healthcare professionals for advice about Complementary and Alternative Medicine (CAM) therapy. Yet, little is known about pharmacists’ CAM education needs. The study aimed to describe pharmacists’ view about the need to incorporate CAM education into the undergraduate pharmacy programme and to identify perceived barriers and mode of delivery for integration of CAM education. In this cross-sectional survey, pharmacists who graduated from the University of Malaya were identified from the alumni database. Only practicing pharmacists were contacted via an email and asked to respond to a structured self-administered questionnaire. The primary outcome measures were whether the respondents supported the incorporation of CAM into pharmacy curriculum and their perceived barriers to the CAM incorporation. Almost all of the respondents (98%) supported the incorporation of CAM education into the pharmacy undergraduate curriculum. Among factors associated with their report of support were fields of their practice, their belief that CAM was effective and their willingness to receive CAM training. Meanwhile perceived barriers to CAM incorporation were lack of reliable sources of CAM information and trained CAM educators. As a healthcare professional, the CAM education received may provide pharmacist with accurate and impartial information on CAM for better patients’ care. Further research into the content and focus of CAM education is necessary to meet the educational needs of pharmacist.
Keywords: CAM educationpharmacistscurriculumpharmacybarriers
Introduction
The use of complementary and alternative medicine (CAM) has been growing rapidly worldwide especially in countries such as the United States (Clarke et al., 2015), Canada (Esmail, 2017), Norway (Naberezhneva, 2014) and Australia (Xue et al., 2007). As compared to other ASEAN countries, Malaysia ranked the highest in terms of CAM usage (Peltzer & Pengpid, 2015). A baseline survey in Malaysia showed that 70% of the respondents have used CAM in their lifetime and more than half of them have used it in the last 12 months (Siti et al., 2008). The use of CAM among Malaysians are undeniably high particularly for asthma (Alshagga et al., 2011), hypertension (Mahfudz & Chan, 2005), chronic disease (Hasan et al., 2009) and cancer (Farooqui et al., 2016).
The escalating trend of CAM use significantly contributes to the growth of CAM industry. According to Health Expenditure Report 1997-2014 by the Health Ministry (Malaysia National Health Accounts Unit of Ministry of Health, 2016), Malaysian’s out-of-pocket expenditure on CAM rose from 380 million USD in year 2010 to 513 million USD in year 2014. The same report showed that Malaysian have the tendency to spend more on CAM rather than on conventional medicines. The increasing demand of CAM can be related to two important global issues: an ageing population and a rise in the number of chronic disease; and the emerging awareness regarding the importance of preventative health and wellbeing (Complementary Medicines Industry Survey, 2014).
Malaysians are more likely to obtain their CAM such as supplements and natural products from community pharmacies due to the absence of such medicines in a hospital and to avoid long waiting time in public hospitals or clinics which offer CAM services (World Health Organization, 2003). The major concerns of natural products are the possibilities of interaction between natural products and conventional medicines and the possibilities of toxicity from natural products or contaminants (Curtis, 2004). These factors trigger patients or customers to frequently question community pharmacists about CAM (Simmon-Yona et al., 2012). Thus, pharmacists play a vital role as a first line reliable healthcare professional in advising and counseling the public.
However, only a handful of pharmacists are very confident in providing advice about therapeutic function, the direction of use and safety of CAM. One of the main reasons is the deficiency of formal CAM training, thus being equipped with the relevant knowledge especially at the undergraduate level is essential (Semple et al., 2006; Tam et al., 2014). As part of healthcare professionals, pharmacists should only advise the patients based on their CAM knowledge and competency. They must only recommend CAM from a reputable or known source of supply as well as good quality and safe CAM. Information regarding CAM can only be provided if the pharmacists receive such education or training previously (Mason, 2005).
The widespread and increasing use of CAM leads to the upsurge interest to incorporate CAM education into the pharmacy curriculum (Ventola, 2010). Among the main perceived barriers to integration of CAM education identified were the lack of scientific evidence for practice and the lack of trained and knowledgeable professionals (James & Bah, 2014; Kreitzer et al., 2002). The process and development of pharmacy curricula to include CAM education are limited due to the numerous controversies which surround CAM and the inadequate core curriculum on CAM that is established or authorised.
Despite the perceived barriers, most of the studies support the integration of CAM education into undergraduate curriculum of pharmacy (Hasan et al.,2011; Hussain et al., 2012; James & Bah, 2014). In several western countries, such implementation and development of CAM education have been taking place for years, and the content of CAM courses are being discussed and reviewed actively (Shields et al., 2003; Tam et al., 2014; Tiralongo, 2013). In contrast, there is limited data regarding the perceived need for CAM education for undergraduate pharmacy students in developing countries, particularly in Malaysia. Thus, this study aimed to determine the perceived need for CAM education among pharmacy graduates of University of Malaya.
Problem Statement
Patients are more likely to ask pharmacists than other healthcare professionals for advice about Complementary and Alternative Medicine (CAM) therapy. Yet, little is known about pharmacists’ CAM education needs.
Research Questions
Given the recent use and developing industries for CAM products and lack of CAM education among the pharmacists, it was important to determine:
What proportion of pharmacists supported CAM education to be incorporated into the pharmacy curriculum?
What were their perceived barriers to incorporation of CAM education in pharmacy curriculum?
Purpose of the Study
We aimed to (a) determine the proportion of pharmacists who supported the integration of CAM education into the pharmacy curriculum (b) describe the responses and beliefs of several CAM statements (c) identify sources of CAM information (d) and to identify perceived barriers and mode of delivery for integration of CAM education. The findings of this study would be used to review and improve the curriculum of the undergraduate pharmacy programme.
Research Methods
Study Design and Setting
This study was a descriptive cross-sectional survey, which was conducted using a structured questionnaire. Online questionnaire was emailed to the pharmacy graduates of University of Malaya. There is an average of 70 students for each batch of pharmacy students and graduates from the past 20 years were contacted. Thus, the population size was estimated to be 1400 people. Data from 400 graduates was needed to validate this survey by using sample size formula below, with margin of error 5%.
N: Population size
e: Margin of error (as a decimal)
z: Confidence level (as a z-score)
p: Percentage value (as a decimal)
Source: Calculating the number of respondents you need. Survey monkey.
Study Population and data collection
The target population of this study was qualified pharmacists who graduated from the University of Malaya (UM). They were identified from the Pharmacy department of UM alumni database and chosen on the basis that they had undergone pharmacy undergraduate curriculum of UM and have been practicing as a pharmacist. The questionnaire was piloted by emailing to 20 pharmacists and the results were not included in final analysis. At least two reminder emails were sent within a month to ensure high response rate.
Instrument
The questionnaire comprised of 4 sections. Section A collected the demographic data of respondents (gender, ethnicity, level of education, year of graduation, current occupation and current work place). Section B examined the awareness and use of CAM therapies. Respondents were required to choose a ‘Yes’ or ‘No’ respond for each statement. Section C sought information about the general attitude towards CAM which consisted of 10 statements. These statements were modified from validated Holistic Complementary and Alternative Medicine Questionnaire (HCAMQ) (Hyland et al., 2003) which has been used by many studies (James & Bah, 2014; Tiralongo et al., 2008; Wahab et al., 2014). Five point Likert scale was used to measure each statement with point descriptors ‘strongly disagree’, ‘disagree’, ‘not sure’, ‘agree’ and ‘strongly agree’. As CHBQ was not validated in Malaysia, measurement of mean score to identify the type of attitude was not done Section D examines the sources of CAM information, perceived barrier and perceived need for CAM education in pharmacy undergraduates. The respondents were given a variety of responses to choose from. For the variable ‘perceived need for CAM education in pharmacy undergraduates,’ the response was a ‘Yes’ or ‘No’ options.
Data Analysis
SPSS version 20 was used to analyze data. Descriptive statistics such as frequency and percentage were used to describe data. Chi-square test or Fisher-exact were carried out to show the association of categorical data. A p-value less than 0.05 was considered to be statistically significant.
Findings
Characteristics of respondents
Out of 951 emails sent out and web link posted in social media namely Facebook, 400 respondents completed the questionnaire form. The response rate was 42.1%. Table
Attitudes towards CAM
Ten statements were modified from validated Holistic Complementary and Alternative Medicine Questionnaire (HCAMQ) (Hyland et al., 2003) to determine general attitudes towards CAM (Table
Awareness and use of CAM
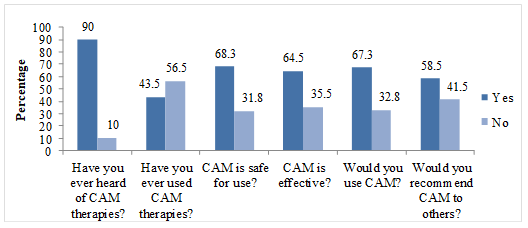
Several questions explored the awareness and use of CAM among respondents (Figure
Source of CAM information
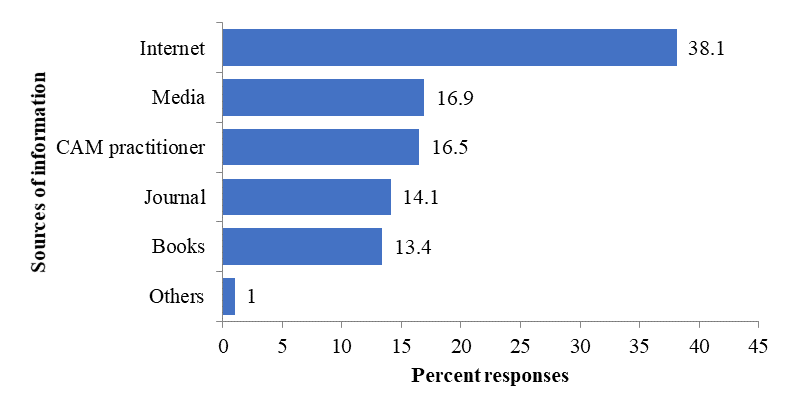
Slightly more than half of the respondents (n=213) had sought information on CAM (Figure
Perceived barriers to CAM education
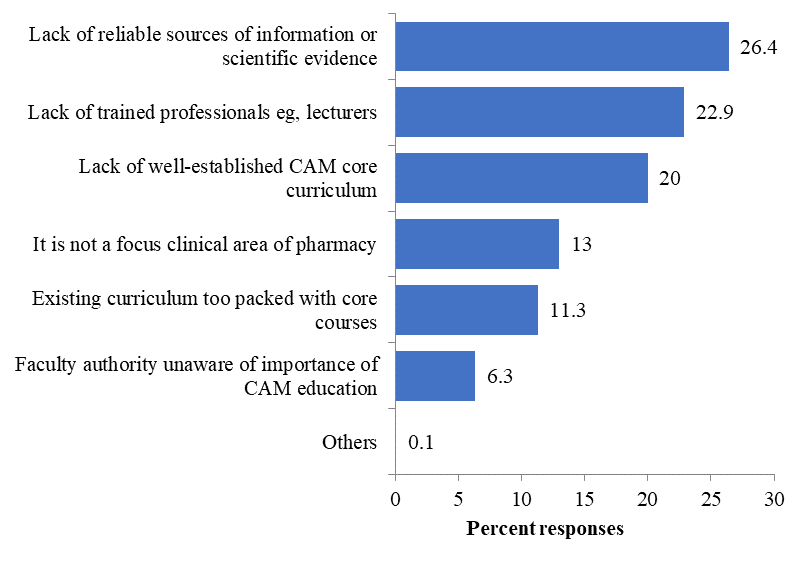
The number of responses received for perceived barrier to CAM education was 1217 as respondents could choose more than one answer for their responses (Figure
Need for integration of CAM into Pharmacy curriculum
Almost 80% of the respondents were interested in receiving training about CAM with slightly more than half of them were non-CAM users. Approximately four fifth of respondents supported the inclusion of CAM topics into Pharmacy curriculum. About a quarter of the respondents felt that CAM subject was not required in the pharmacy curriculum as it was the job of a CAM practitioner and among these respondents, most of them are non-CAM users.
Mode of offering CAM education
Opinion of respondents was sought regarding how CAM should be offered. Ten respondents felt that CAM should not be offered at all while the majority (72.5%) preferred CAM to be offered as elective subject. Another 20.3 % of the respondents indicated that CAM should be offered as part of an existing compulsory subject. Only 20 respondents preferred CAM to be offered as a compulsory subject.
Discussion
We describe pharmacists’ view about their opinion about the need to incorporate CAM education into the undergraduate pharmacy programme and identify perceived barriers and mode of delivery for integration of CAM education. The demographic variables that influence the opinion regarding the need of CAM incorporation are difficult to interpret, as none of the variables examined are statistically associated with the opinion on the need for CAM integration.
Even though all respondents had previously heard of CAM therapies but less than half of them had used it. This result disagrees with most studies in which prevalence of CAM use is more than 50% in Australia, Japan, and Malaysia (Siti et al.,2008; Xue et al., 2007; Yamashita et al, 2002). The lower prevalence rate of CAM use in our study is probably explained by the fact that unlike other studies, our target respondents are practicing pharmacists trained in conventional medicine. They may prefer conventional medicine over CAM. However, around two-thirds of the respondents think that CAM is safe for use, is effective and that they would probably use it in the future. The result is compatible with a study from India which found that most of the doctors believed in the beneficial effects of CAM and would recommend patients to use CAM (Roy et al., 2015).
Healthcare professionals specifically pharmacists is the most important and reliable resources for information on medicines (Mason et al., 2005; Ellinoy, 2006), and yet they are incapable of searching reliable and required CAM information (Owen et al., 2003). Our findings that the most common sources of CAM information are from the internet, followed by media such as newspaper and CAM practitioners is consistent with a study involving pharmacists in the Czech Republic (Pokladnikova & Desiree 2014). The reliability and accuracy of the internet as the source of information on CAM is questionable and doubtful as the posted information was not regulated or validated. Hence, formal training or CAM education which has a very high degree of reliability should be given attention.
Similar with previous studies (James & Bah 2014; Kreitzer et al., 2002) we found lack of reliable sources of information or scientific evidence as the most common perceived barrier for integration of CAM education in the pharmacy curriculum. Besides that, the scientific research on efficacy and effectiveness of integrative therapy is still limited despite the publication of several studies (Li et al., 2009; Wolever et al., 2011). Thus, it would be a challenging task for the academic professional to establish a CAM core curriculum which is applicable for future practice.
Like other studies (Hasan et al.,2011; Hussain et al., 2012; James & Bah, 2014; Tam et al., 2014), the majority of the respondents agreed that current Pharmacy curriculum should include topics on CAM and most respondents preferred CAM to be offered as an elective course. The CAM education was usually introduced as an elective course in universities (Shields et al., 2003; Tam et al., 2014). Although the elective course was able to increase the knowledge of students, it was suggested to integrate CAM into each module of pharmacy undergraduate curriculum (Tam et al., 2014). Despite CAM being integrated into pharmacy curriculum as an elective course for eight years in the University of Alberta, Canada (Tam et al., 2014), pharmacists who graduated from the University were still uncomfortable and lacked the confidence to advise patients on CAM. A position statement of CAM education has recommended CAM to be mandatory (Tiralongo et al., 2008).
The findings of this study will be useful for pharmacy curriculum review for the Department of Pharmacy, University of Malaya. However, our findings should be interpreted in the context of several limitations. First, it is difficult to define the concept of CAM. There are significant differences between countries in the definition and categorisation of CAM depending on their regulation on CAM. For instance, music therapy may be classified as CAM in one country, but it is not recognised as a therapy in another country. To avoid confusion among the respondents, we have conceptualised CAM as medication or therapy excluded from western conventional medicine or treatment. Some respondents might still have difficulty understanding the specific definition of CAM although we specifically defined CAM at the beginning of the online survey.
Second, we were able to capture only UM pharmacy graduates from the year 2000 to 2015. Graduates earlier than the year 2000 were excluded in our study as their personal information or contacts were unavailable in the department. Thus, our respondents may not be representative of all UM graduates;
Conclusion
The majority of the pharmacists supported the incorporation of CAM education in the undergraduate pharmacy programme. Development of CAM education in pharmacy curriculum of the University of Malaya should be done to establish a comprehensive CAM core curriculum which is useful in future pharmacy practice. Further research into the content and topic od CAM education is needed to fulfill the training needs of the future pharmacists.
References
- Alshagga, M.A., Al-Dubai, S.A., Faiq, S.S.M. & Yusuf, A.A. (2011). Use of complementary and alternative medicine among asthmatic patients in primary care clinics in Malaysia. Annals of Thoracic Medicine, 6(3), 115-119.
- Calculating the number of respondents you need. (n.d.). Retrieved July 10, 2018, from Survey Monkey:http://help.surveymonkey.com/articles/en_US/kb/How-many-respondents-do-I-need?bc=Buying_Responses
- Clarke, T.C., Black, L.I., Stussman, B.J., Barnes, P.M. & Nahin, R.L. (2015) Trends in the Use of Complementary Health Approaches Among Adults: United States, 2002-2012. National Health Statistics Reports, 79, 5.
- Complementary Medicines Industry Survey. (2014). Mawson: Complementary Medicines Australia.
- Curtis, P. (2004). Safety Issues in Complementary and Alternative Healthcare. The Convergence of Complementary, Alternative & Conventional Healthcare: Educational Resources for Health Professionals. Chapel Hill, NC: University of North Carolina.
- Ellinoy, B. (2006). What is an integrative pharmacist? Retrieved July 20, 2018, Retrieved from Integrative Pharmacist.com: http://www.integrativepharmacist.com/whatis.htm
- Esmail, N. (2017). Complementary and Alternative Medicine: Use and Public Attitudes 1997, 2006, and 2016. Fraser Institute, Canada.
- Essential Drugs Monitor. (2003). Retrieved from July 22, 2018, from World Health Organization: http://apps.who.int/medicinedocs/pdf/s4941e/s4941e.pdf
- Farooqui, M., Hassali, M.A., Abdul Shatar, A.K., Farooqui, M.A., Saleem, F., Haq, N.U., & Othman, C.N. (2016) Use of complementary and alternative medicines among Malaysian cancer patients: A descriptive study. Journal of Traditional and Complementary Medicine, 6, 321–326.
- Hasan, S.S., Ahmed, S.I., Bukhari, N.I., & Loon, W.C. (2009) Use of complementary and alternative medicine among patients with chronic diseases at outpatient clinics. Complementary Therapies in Clinical Practice, 15(3), 152-157.
- Hasan, S.S., Yong, C.S., Babar, M.G., Naing, C.M., Hameed, A., Baig, M.R., Iqbal, S.M. & Kairuz, T. (2011). Understanding, perceptions and self-use of complementary and alternative medicine (CAM) among Malaysian pharmacy students. BMC Complementary and Alternative Medicine, 11(1), 95.
- Hussain, S., Malik, F., Hameed, A., Ahmed, S., Riaz, H., Abbasi, N. & Malik, M. (2012). Pakistani Pharmacy Students’ Perception About Complementary and Alternative Medicine. American Journal of Pharmaceutical Education, article 21.
- Hyland, M.E., Lewith, G.T. & Westoby, C. (2003) Developing a measure of attitudes: the holistic complementary and alternative medicine questionnaire. Complementary Therapies in Medicine, 11(1), 33-38.
- James, P.B. & Bah, A.J. (2014). Awareness, use, attitude and perceived need for Complementary and Alternative Medicine (CAM) education among undergraduate pharmacy students in Sierra Leone: a descriptive cross-sectional survey, BMC Complementary and Alternative Medicine, 14(1), 438.
- Kreitzer, M.J, Mitten, D., Harris, I. & Shandeling, J. (2002) Attitudes toward CAM among medical, nursing and pharmacy faculty and students: A comparative analysis. Alternative Therapies in Health and Medicine, 8(6), 44.
- Li, A.Y., Cong,S., Lu, H., Li, J.J., Zhao, L. (2009). Clinical Observation on Treatment of Tourette Syndrome by Integrative Medicine. Integrative Medicine, 15(4), 267-271.
- Mahfudz, A.S. & Chan, S.C. (2005) Use of complementary medicine amongst hypertensive patients in a public primary care clinic in Ipoh. Medical Journal of Malaysia, 60(4), 454-459.
- Malaysia National Health Accounts Health Expenditure Report 1997-2014. (2016). Malaysia National Health Accounts Unit of Ministry of Health
- Mason, P. (2005, January 1). Why should pharmacy students be interested in complementary and alternative medicine? Retrieved July 22, 2018, from Pharmaceutical Journal: http://www.pharmaceutical-journal.com/career/career-feature/why-should-pharmacy-students-be-interested-in-complementary-and-alternative-medicine-/10018088.article
- Naberezhneva, N. (2014) Complementary and Alternative Medicine in Norway. Changes in CAM prevalence and user characteristics in Norway from 2002 to 2012. Reprosentralen, Blindern, Oslo. Retrieved from https://www.duo.uio.no
- Owen, D.J. & Fang, M.-L. E. (2003). Information-seeking behavior in complementary and alternative medicine (CAM): an online survey of faculty at a health sciences campus. Journal of the Medical Library Association, 91(3), 311-321.
- Peltzer, K. & Pengpid, S. (2015) Utilization and Practice of Traditional/Complementary/ Alternative Medicine (T/CAM) in Southeast Asian Nations (ASEAN) Member States. Studies on Ethno Medicine, 9(2), 209-218.
- Pokladnikova, J. & Desiree, L. (2014). CAM Attitudes, Self-reported Use and Client Recommendations of Czech Pharmacists and Pharmacy Technicians: Implications for Training. Klinickafarmakologie a farmacie, 28(2), 49-54.
- Roy, V., Gupta, M. & Ghosh, R.K. (2015). Perception, attitude and usage of complementary and alternative medicine among doctors and patients in a tertiary care hospital in India. Indian Journal of Pharmacology, 47(2), 137-142.
- Semple, S.J., Hotham, E., Rao, D., Martin, K., Smith, C.A. & Bloustien, G.F. (2006). Community pharmacists in Australia: barriers to information provision on complementary and alternative medicines. Pharmacy World and Science, 28(6), 366-373.
- Shields, K.M., McQueen, C.E. & Bryant, P.J. (2003) Natural Product Education in Schools of Pharmacy in the United States. American Journal of Pharmaceutical Education, 67(1), 43-38
- Simmons-Yona, A., Rothb, M.T., Vuc, M., Kavalieratosd, D., Weinbergere, M. &Raob, J.K. (2012). Understanding pharmacists’ experiences with advice-giving in the community pharmacy setting: A focus group study. Patient Education and Counseling, 89(3), 476-483.
- Siti, Z.M., Tahirb, A., Ida, F. A., Ami, F., Sondib, S., Azmanb, Maimunahb, Hanizab., Siti Haslindab, Zulkarnainb, Zakiaha, Wan Zalehab. (2008). Use of traditional and complementary medicine in Malaysia: a baseline study. Complementary Therapies in Medicine, 17(5-6), 292-299.
- Tam, K. & Banh, H.L. (2014) Attitudes of Alberta Pharmacists pertaining to Traditional Chinese Medicine practice and Complementary Alternative Medicine. Journal Pharma Care Health Sys, 1(108), 2.
- Tiralongo, E. & Wallis, M. (2008). Integrating Complementary and Alternative Medicine Education Into the Pharmacy Curriculum. American Journal of Pharmaceutical Education, 72(4), 74.
- Tiralongo, E. (2013). Inclusion of complementary and alternative medicine (CAM) teaching into pharmacy curricula – a cross-sectional survey of Australian and New Zealand Schools/Department of pharmacy. Presented at the INTED2013, Valencia, Spain (2013).
- Ventola, C. L. (2010). Current issues regarding complementary and alternative medicine (CAM) in the United States: part 1: the widespread use of CAM and the need for better-informed health care professionals to provide patient counseling. Pharmacy and Therapeutics, 35(8), 461.
- Wahab, M.S.A., Ali, A.A., Zulkifly, H.H. & Aziz, N.A. (2014). The need for evidence-based complementary and alternative medicine (CAM) information in Malaysian pharmacy curricula based on pharmacy students’ attitudes and perceptions towards CAM. Currents in Pharmacy Teaching and Learning, 6(1), 114-121.
- Wolever, R.Q., Webber, D.M., Meunier, J.P., Greeson, J.M., Lausier, E.R. & Gaudet, T.W. (2011). Modifiable Disease Risk, Readiness to Change, and Psychosocial Functioning Improve with Integrative Medicine Immersion Model. Alternative Therapies in Health & Medicine, 17(4), 38-47.
- Xue, C.C., Zhang, A.L., Lin, V., Da Costa, C. & Story, D.F. (2007). Complementary and alternative medicine use in Australia: a national population-based survey. Journal of Alternative and Complementary Medicine, 13(6), 643-650.
- Yamashita, H., Tsukayama, H. & Sugishita, C. (2002). Popularity of complementary and alternative medicine in Japan: a telephone survey. Complementary Therapies in Medicine, 10(2), 84-93.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
14 January 2019
Article Doi
eBook ISBN
978-1-80296-052-5
Publisher
Future Academy
Volume
53
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-812
Subjects
Education, educational psychology, counselling psychology
Cite this article as:
Chew, S., Aziz, Z., & Huin, W. (2019). Need For Complementary And Alternative Medicine (Cam) Education Among Pharmacists. In Z. Bekirogullari, M. Y. Minas, & R. X. Thambusamy (Eds.), ICEEPSY 2018: Education and Educational Psychology, vol 53. European Proceedings of Social and Behavioural Sciences (pp. 603-614). Future Academy. https://doi.org/10.15405/epsbs.2019.01.58

