Abstract
Total knee arthroplasty is a chirurgical intervention that has increased in the last few years. The prevention and reduction of knee flexion contracture is crucial after these operations and it can be achieved by using dynamic splinting. The objective of this study is to describe the beneficial effects of using dynamic splinting as a complement in the physical rehabilitation program, leading to a reduction of contractures and the recovery of full knee extension after total knee arthroplasty operation. An integrative literature review was performed using the PI[C]OD method by searching the following databases: CINAHL, MedicLatina, Medline, Cochrane Database Syst Rev, CCRCT, Nursing & Allied Health Collection: Comprehensive, SciELO, whose studies were published in the period 2012-2017. This search yielded five articles that met the inclusion criteria. Professionals consider the dynamic splint an important tool to use during rehabilitation programs. The main benefits obtained are a greater range of motion without pain, a high tolerance of orthopedic use, since the tension force can be controlled, and a greater acceptance and satisfaction by patients. However, data supporting the systematic approach to appropriate selection of elastic traction are scarce. Dynamic splitting is a strategy frequently used in the rehabilitation of patients with deformities and physical injuries based on anatomical and biomechanical aspects and logical principles. Patient positioning and immobilization are crucial components of a rehabilitation program that emphasizes the prevention of contractures. The use of these devices in the different phases of the rehabilitation process, varies according to the injury and adjustment needed.
Keywords: Dynamic splittingtotal knee arthroplastyknee flexion contracturerehabilitation
Introduction
Stretching is a habitual activity used by athletes, older adults or rehabilitation patients (Page, 2012). It is commonly used for the treatment and prevention of contractures that are a frequent complication of several neurological conditions. Contractures are related to many musculoskeletal situations and pathologies, burns and surgery (Fergusson, Hutton & Drodge, 2007; Katalinic, Harvey, Herbert, Moseley, Lannin & Schurr, 2010). Nowadays, although the beneficial effects of stretching are recognized, the selection of the best type of stretching for a specific goal or outcome, remains controversial (Page, 2012).
Numerous authors have compared static and dynamic stretching on range of motion, strength, and performance. Many non-invasive assistive devices, including dynamic splints, employ the biomechanical adaptation of keeping the joint at end-range. This strategy of low-load and prolonged-duration stretch, that utilizes a dynamic tension constantly, reduces the contracture (Willis, 2008; Bonutti, McGrath, Ulrich, McKenzie, Seyler & Mont, 2008). Night splints are considered to stretch, as well as prevent the overnight tissue contracture, responsible probably for the morning pain present in many situations. A day-wear static progressive stretch brace is another option to consider and a substitute to night splint, and it takes full advantage of the viscoelastic nature of the soft tissue that could diverge on patients’ tolerance (Sharma & Loudon, 2010). These devices have been evaluated in several studies, regarding their capacity of stretch, by applying them in different ways and in specific pathologic situations.
Many authors have reported positive results using an adjustable orthosis to make available a static progressive stretch for the treatment of joint stiffness of the ankle, wrist, elbow, forearm and knee, due to immobilization or a limited range of motion. In the specific case of the knee, it could occur as a consequence of open reduction and internal fixation of fractures, ligament reconstruction, unicompartmental knee replacements or total knee arthroplasty (Bonutti, Marulanda, McGrath, Mont & Zywiel, 2010).
The range of motion presented in synovial joints can be restricted by joints and muscles. Muscle provides passive muscle tension that is reliant on its structural properties (viscoelastic) and surrounding fascia, even though dynamic muscle contraction provides active tension. This active tension is dependent on the neuroreflexive properties of muscle: explicitly, peripheral motor neuron innervation and reflexive activation (Page, 2012).
Muscles contain viscous and elastic properties which influence the time that a muscle can be stretched. The elements of a muscle with higher elastic properties will perform as a rubber band: it will lengthen and then, upon release, return to its original length. This phenomenon is independent of time. On the other hand, the movement of a viscous muscle is dependent on time. Consequently, the length of a muscle will rise with time, if it is held stretched to a specific length. The muscle will return gradually to its original length once this force is removed (Taylor, Dalton, Seaber & Garrett, 1990).
Numerous studies indicate that stretching increases joint range of motion and soft tissue extensibility. Normally, stretching emphasizes on increasing the length of a musculotendinous unit, by increasing the distance among a muscle's origin and insertion. Concerning this issue, muscle tension is habitually inversely associated to length. While a reduced muscular tension is associated to an increased muscle length, the improved muscular tension is related to reduced muscle length. However, the stretching of a muscle adds tension to additional structures, for example the joint capsule and fascia (Page, 2012).
Patients are prescribed stretches to increase their range of motion either in the short term or long term. The momentary effects of stretching have been widely studied and resulting outcomes demonstrated immediate increases in the length of soft tissue, with instantaneous rises in joint range of motion and decreases in resistance to passive joint movement. But, the effects of viscous deformation of tissues only last temporarily after the stretch is removed. However, the findings from the systematic review conducted by Katalinic, Harvey, Herbert, Moseley, Lannin & Schurr (2010) demonstrated that no important immediate effects of stretch on joint mobility exists in people with frailty, ankle fractures or total knee replacements.
For the treatment and prevention of contractures, the lasting effects of stretching are more significant than the previous transient effects. Existing knowledge is based on studies which indicate that soft tissue undergoes structural adaptations in response to regular and intensive stretch. But, in the systematic review previously mentioned, the long-term effects of stretch in people with ankle fractures or total knee replacement are small and clinically insignificant. Concerning the dosage of stretch administered, results from studies indicate that increasing dosages of stretch did not influence joint mobility. Additionally, comparing the effectiveness of different stretch interventions including serial casting, positioning, splinting, self-administered stretches and other stretches, data did not support that any particular intervention is superior to another (Katalinic, Harvey, Herbert, Moseley, Lannin & Schurr, 2010).
Several orthopedic patients may take advantage of both static and pre-contraction stretching, while patients with joint contractures do not appear to benefit from stretching. Page (2012) referring to the systematic review conducted by Katalinic, Harvey, Herbert, Moseley, Lannin & Schurr (2010), contended that it happens because that contractures result frequently from shortness in non-contractile tissues, for example capsuloligamentous structures, rather than muscle tightness.
As with other populations, although the efficacy of stretching on the treatment of orthopedic conditions or injury is well known, results must be based on the individual patients.
Problem Statement
Rehabilitation nurses are confronted with the challenge to provide excellence care, and seek to do so in accordance with evidence-based practice and not only in isolated and unsystematic experience, taking into account individual patients' needs and choices. The evidence-based practice is the use of the finest scientific evidence to support the clinical decision making (Santos, Pimenta & Nobre, 2007).
Stretching is included frequently in rehabilitation programs to increase muscle length and range of motion, to align collagen fibers during healing muscle, or is used, for example, for management of knee pain (Page, 2012). Regardless of positive results of numerous sorts of studies, it is difficult to separate the success of the stretching component of the entire treatment plan for the reason that protocols habitually comprise strengthening and interventions in addition to stretching. Thus, an integrative review of the literature was performed, based on evidence-based practice, as a strategy that will allow the use of research results in rehabilitation nurses’ clinical practice.
Research Questions
Taking into account the subject under study and considering that rehabilitation nurses are competent professionals, with technical and scientific skills, with the purpose of an evidence-based practice, the following research question arose: “What are the beneficial effects of the dynamic splint for patients undergoing total knee arthroplasty?”
Purpose of the Study
Considering the research question, the aim of this study is to identify the benefits of using dynamic splinting, as a complement in the physical rehabilitation program, leading to a reduction of contractures and recovering full knee extension after total knee arthroplasty operation.
Research Methods
An integrative literature review was achieved using the PI[C]OD method. With the purpose of selecting eligible studies, a simple search was performed initially, limited to MEDLINE and CINAHL, followed by an analysis of the words in the titles. At the second stage, our search was extended to abstracts that made possible the examination of the terms used to describe the studies, independently of these being present in the title. A search was conducted in the National Center for Biotechnology Information website with the intent of confirming if the preliminary terms were Medical Subject Headings (MeSH terms). We obtained a positive response to:
#1 MeSH descriptor “Dynamic splinting system” (explore all trees);
#2 MeSH descriptor “Total knee replacement” (explore all trees);
#3 MeSH descriptor “Total knee arthroplasty” (explore all trees);
#4 MeSH descriptor “Mecanoterapia” (explore all trees);
This research comprised electronic searches in the subsequent databases: CINAHL Complete, Medline Complete, MedicLatina, Nursing & Allied Health Collection: Comprehensive from the EBSCOhost platform supplemented by the PubMed, Database of Abstracts of Reviews of Effects, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Cochrane Metodology Register, Health Technology Assessments, NHS Economic Evaluation Database, SciELO-Scientific Electronic Library Online, B-on and Library, Information, Science and Technology Abstracts.
After the survey described above, research limiters were applied, because of the magnitude of the sample obtained. Only the studies with the following requirements were considered: full text articles, published in Portuguese or English language, date of publication between January 2012 and December 2017, and using quantitative research methods.
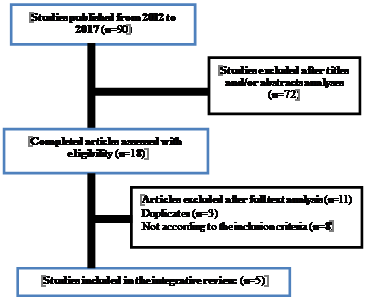
This search yielded 90 studies (published from 2012 to 2017), and once we read the titles and abstracts it was reduced to 72, because the excluded ones did not mention the subject under study. When we analyzed the full text articles (n = 18), by applying additional criteria, which were established based on the PI[C]OD methodology presented in Table
Once the research was performed on EBSCOhost database we found 64 results and 26 on B-on database. Extracted data comprised details of population, specific objectives, methodology of study, interventions and pertinent conclusions related to the subject under study. The method of selection of the corpus of this study was summarized in the subsequent flowchart (Figure
Findings
As described above, based on the request for more rigorous selection criteria, only 5 articles were carefully chosen for the study corpus.
With the intent to answer the research question “What are the beneficial effects of dynamic splint for patients undergoing total knee arthroplasty?”, the main results from the selected studies were grouped and organized in a table presented below. In this table we summarized the dimension and characteristics of the studies, specifically the methods, participants, objectives and principal outcomes/conclusions, thus simplifying the comparison among them.
Studies were separated, according to the methodology implemented, in two categories: two case reports (Finger & Willis, 2008; Hwang, Moon, Kim & Park, 2016) and three retrospective studies (Pace, Nasreddine, Simoni, Zurakowsky & Kocher, 2016; Vulcano, Markowitz, Fragomen & Rozbruch, 2016; Bhave, Shabtai, Ong, Standard, Paley & Herzenberg, 2015).
Table
Conclusion
Flexion contractures can be a consequence of long-term progression of certain pathologies, as osteoarthritis or rheumatoid arthritis, or a result of chirurgical interventions, for example, following a total knee arthroplasty (TKA). It causes severe pain and damages knee joint function, with subsequent inability to walk and restriction to daily activities. Different treatment methods are available to correct flexion contracture and TKA can be a therapeutic option. Postoperatively physical therapy, supplemented by serial castings or the use of a dynamic splint are additional strategies used to correct the remaining flexion contracture. The analysis of the 5 articles selected allowed us to answer the research question that guided this study.
In the case report stated by Finger and Willis (2008), a 61-year-old male presented with knee flexion contracture after TKA and his preoperative maximal active range of motion (AROM) was -5º from complete extension. This patient had a 30 year history of earlier knee injuries, osteoarthritis and four previous knee chirurgical interventions. Physical therapy on its own did not fully reduced the contracture and dynamic splinting was prescribed for daily low-load, prolonged-duration stretch. After 28 physical therapy sessions the active range of motion improved from -20º to -12º and following eight added weeks with nightly wear of dynamic splint, the patient regained full AROM in knee extension (from -12º to 0º).
The dynamic splint provides a constant tension to tissue in flexion and extension, depending on patients’ needs, while with the use of static splint this is provided in regular intervals. Some authors recommend that dynamic splints must be used for long periods to activate the biological responses which produce plastic deformity of the tissues. If a tissue is stretched outside its limits of elasticity, a tissular lesion will occur and when this happens repetitively, the tissue stops stretching and it is more easily damaged. So, it is crucial that elongation and the consequently applied tension, can be tolerated by the patient. Good stretching can be accomplished at night, as the tissues are more relaxed (Davalos, Galluci, Alfie, Carli & Thomas, 2010).
A study conducted by Pace, Nasreddine, Simoni, Zurakowsky and Kocher (2016), verified the benefits of using the dynamic splint in the paediatric and adolescent patients with arthrofibrosis following an index knee surgery. Patients with flexion deficits presented median improvement of 30º in flexion and the use of this device increased knee ROM (84%) and reduced the need for subsequent surgery in 58% of all participants included in the study.
Various non-surgical treatment methods, as dynamic splints, have been recommended for correction of mild to moderate contractures. Surgical treatment options, including the stretching of iliotibial band are followed by the application of dynamic splints.
Knee flexion contracture is an incapacitating disorder that may affect patients with neurogenic conditions, posttraumatic deformities, congenital abnormalities and after total knee replacement. In a study for assessing the clinical results of patients with knee flexion contractures (KFC) and associated ankle equinus using gradual correction with a circular external fixator (CEF) to match the remaining deformity after the minimal incision soft-tissue release, conducted by Vulcano, Markowitz, Fragomen and Rozbruch (2016), the mean ROM at final follow-up (13 months) was -10º extension, 64º flexion, 9º ankle dorsiflexion and 29º ankle plantar flexion. The difference among preoperative and postoperative ROMS was statistically significant (
In the case report stated by Hwang, Moon, Kim and Park (2016), a 26-year-old female patient diagnosed with rheumatoid arthritis underwent a TKA and serial casting and physical therapy postoperatively to correct the remaining flexion contracture. Complete knee extension was achieved. Concerning to flexion contractures changes during the postoperative follow-up period, some authors recommended a complete intraoperative correction of all flexion contracture abnormalities, since the residual knee joint deformity does not improve over time. Conversely, other authors state that complete surgical correction of flexion contracture is unnecessary as the remaining flexion contracture would improve in time after TKA. In this case report, the remaining flexion contracture after TKA has been treated successfully with serial casting and physical therapy.
Few studies have reported complications associated with loss of joint motion, regardless of the current knowledge about the effect of knee extension on outcome and function. Most of the available studies had small or mixed sample sizes and stated mixed outcomes.
In a study conducted by Bhave, Shabtai, Ong, Standard, Paley and Herzenberg (2015), that included 23 patients (27 limbs) who underwent femoral lengthening with an internal device for the correction of limb length discrepancy, all participants had a knee flexion contracture range from 10º to 90º during the lengthening course and were treated with a custom knee device splint and specific physical therapy. The mean amount of lengthening was 5.4 cm. Only 2 of 27 knees did not achieved full resolution of flexion contracture, after a regular use (3.8 weeks) of the custom knee device. The average final extension was 1.4º. Only 27% of limbs also required a soft tissue release to correct the knee flexion contracture. The use of a custom knee device associated with specialized physical therapy is an inexpensive, a non-invasive strategy and is effective for patients that underwent femoral lengthening.
Evidence of the results discussed previously revealed that professionals consider the dynamic splint a crucial device that can be use in the rehabilitation process of a diverse range of patients.
Dynamic splitting is a strategy commonly used in the rehabilitation of patients with deformities and physical injuries based on anatomical and biomechanical aspects and logical principles. The regular use of these devices allows restoring, for example, of part or all the gripping force or mobility of the limbs (knee, shoulder or ankle joints), required in the performance of daily life activities.
Patient positioning and immobilization are crucial components of a rehabilitation program that emphasizes the prevention of contractures. The use of these devices in the different phases of the rehabilitation process, varies according to the injury and adjustment needed.
Dynamic splint allows the patient to adjust the tension force gradually, causing small changes in the length of the tissues. The ideal orthotic design permits small changes in joint motion, every time there is a report of improvements associated with the range of motion.
The main benefits obtained by using a dynamic splint are a greater range of motion without pain, a high tolerance of orthopedic use, since the tension force can be controlled, and a greater acceptance and satisfaction by patients. However, data supporting the systematic selection approach of elastic traction according to the patients’ needs are scarce. As rehabilitation nurses need to have an in-depth knowledge about these devices, in order to use them effectively in the rehabilitation process of the patients and obtain the best possible outcomes, the findings of this study will be useful in providing more in-depth knowledge to achieve this aim.
Acknowledgments
We would like to thank the librarians of the School of Health of Viseu. We acknowledge the financing for this study by FCT and CI&DETS, Health School /Polytechic Institute of Viseu.
References
- Bhave, A., Shabtai, L., Ong, P.H., Standard, S.C., Paley, D., & Herzenberg, J.E. (2015). Custom Knee Device for Knee Contractures after Internal Femoral Lengthening. Orthopedics; 38(7):e567-72. Retrieved from DOI 10.3928/01477447-20150701-53
- Bonutti, P.M., Marulanda, G.A., McGrath, M.S., Mont, M.A., & Zywiel, M.G. (2010). Static progressive stretch improves range of motion in arthrofibrosis following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc, 18, 194-199. Retrieved from DOI 10.1007/s00167-009-0947-1
- Bonutti, P.M., McGrath, M.S., Ulrich, S.D., McKenzie, S.A., Seyler, T.M., & Mont, M.A. (2008). Static progressive stretch for the treatment of knee stiffness. Knee, 15, 272-276.
- Davalos, M.A., Galluci, G., Alfie, V., Carli, P., & Thomas, M.G. (2010). Dynamic Splint for the Treatment of Stiff Elbow. Journal of Hand Therapy, 23, e14-e15. Retrieved from DOI https://doi.org/10.1016/j.jht.2010.09.032
- Finger, E., & Willis, F.B. (2008). Dynamic splinting for knee flexion contracture following total knee arthroplasty: a case report. BioMed Central: Cases Journal, I, 421. Retrieved from DOI 10.1186/1757-1626-1-421
- Fergusson, D., Hutton, B., & Drodge, A. (2007). The epidemiology of major joint contractures: a systematic review of the literature. Clinical Orthopaedics and Related Research; 456(3), 22–9.
- Hwang, Y.S., Moon, K.P., Kim, K.T., & Park, W.S. (2016). Total Knee Arthroplasty for Severe Flexion Contracture in Rheumatoid Arthritis Knees. Knee Surg Relat Res., 28(4):325-329. Retrieved from https://doi.org/10.5792/ksrr.16.020
- Katalinic, O.M., Harvey, L.A., Herbert, R.D., Moseley, A.M., Lannin, N.A., & Schurr, K. (2010). Stretch for the treatment and prevention of contractures. Cochrane Database Syst Rev., 9, CD007455.
- Mendes, K. D. S., Silveira, R. C. D. C. P., & Galvão, C. M. (2008). Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto & Contexto-Enfermagem, 17(4), 758-764.
- Pace, J.L., Nasreddine, A.Y., Simoni, M., Zurakowsky, D., & Kocher, M.S. (2018). Dynamic Splinting in Children and Adolescents with Stiffness After Knee Surgery. J Pediatr Orthop, 38(1), 38-43. Retrieved from DOI 10.1097/BPO.0000000000000730
- Page, P. (2012). Current Concepts in Muscle Stretching for Exercise and Rehabilitation. Int J Sports Phys Ther., 7(1), 109–119. PMID: 22319684
- Santos, C.M., Pimenta, C.A., & Nobre, M.R. (2007). The PICO Strategy for the Research Question Construction and Evidence Search. Rev Latino-am Enfermagem, 15(3), Retrieved from 508-11. DOI 10.1590/S0104-11692007000300023
- Sharma, N.K., & Loudon J.K. (2010). Static progressive stretch brace as a treatment of pain and functional limitations associated with plantar fasciitis: a pilot study. Foot Ankle Spec., 3, 117-124. Retrieved from DOI 10.1177/1938640010365183
- Taylor, C.D., Dalton, J.D.Jr., Seaber, V.Jr., Garrett, A., & William. (1990). Viscoelastic properties of muscle-tendon units. The biomechanical effects of stretching. The American journal of sports medicine, 18, 300-9. Retrieved from DOI 10.1177/036354659001800314.
- Vulcano, E., Markowitz, J.S., Fragomen, A.T., & Rozbruch, S.R. (2016). Gradual correction of knee flexion contracture using external fixation. Journal of Limb Lengthening & Reconstruction, 2, 102-107.
- Willis, F.B. (2008). Dancer restores knee flexion through dynamic splinting. BioMechanics, 15(1), 49-54.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
19 November 2018
Article Doi
eBook ISBN
978-1-80296-047-1
Publisher
Future Academy
Volume
48
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-286
Subjects
Health, psychology, health psychology, health systems, health services, social issues, teenager, children's health, teenager health
Cite this article as:
Albuquerque, C., Oliveira, J., Rodrigues, C., & Martins, R. (2018). Beneficial Effects Of Dynamic Splint After Total Knee Arthroplasty. In Z. Bekirogullari, M. Y. Minas, R. X. Thambusamy, & C. Albuquerque (Eds.), Health and Health Psychology - icH&Hpsy 2018, vol 48. European Proceedings of Social and Behavioural Sciences (pp. 200-209). Future Academy. https://doi.org/10.15405/epsbs.2018.11.21

