Abstract
Brain tumour diagnosis affects the lives of many patients, and the burden can be overwhelming for patients with psychiatric disorders. The study aimed to determine the prevalence of major depressive disorder (MDD) and its severity among Malaysian brain disorder patients. The study also investigated on changes in functional and physical performance of patients and its relationship with macrophages inflammatory cells. This study was conducted at Hospital Kuala Lumpur (n=100) and Hospital Universiti Sains Malaysia (n=22). International Neuropsychiatric Interview MINI questionnaire, Patient Health Questionnaire PHQ-9, Karnofsky performance scale (KPS) and Barthel Index (BI) questionnaire were used in the study. The plasma CD68 macrophages measured by commercialized Elisa kit. Spearman rho correlation was used to examine the relationship among the variables. The prevalence of MDD among brain tumour or brain disorder patients was 30.0% (n=30) and severe depression was 6.67% %. The KPS score of the astrocytic glioma patients reduced after surgery and improved at the 6th month of post-surgery. The BI score was improved after the surgery. The KPS score correlated with BI score. However no significant correlation was found with CD68 macrophage level. Thus targeting these parameters might play an important role in the effective treatment of the patients.
Keywords: Major depressive disorderbrain disorderCD68 macrophagetumourBarthel IndexKarnofsky Performance Scale
Introduction
The brain and other nervous system cancer incidence was 3.3 per 100,000 population. The male account for 3.6 and female 3.1 per 100,000 population in peninsular Malaysia in the year of 2006
Major depressive disorder (MDD)
For affected patients, the burden of having brain tumour is compounded by the fact that these patients tend to develop psychiatric disorders. Major depressive disorder (MDD) includes symptoms such as depressed mood, loss of interest, weight loss or weight gain, insomnia, fatigue, feelings of worthlessness, poor concentration and frequent thoughts of death. To be diagnosed with MDD, patients should have at least five of the symptoms mentioned above, including depressed mood or loss of interest, for a duration of at least two weeks (
Assessment of the Functional and Physical Performance
Assessment of functional and physical performance among the astrocytic glioma patients were done using two well established validated questionnaires such as Karnofsky Performance Scale (KPS) (Crooks, 1991; de Haan R, 1993; Hollen PJ, 1994; Oxford Textbook of Palliative Medicine, Oxford University Press," 1993; Schag, 1984; Toole, 1991)and Barthel Index (BI) (Mahoney, 1965). Both BI and KPS scale scores varies from 0 to 100. The BI with the score 100 is regarded as independent and KPS score with 100 is regarded as no symptoms in the patients. The 0 score of BI represent being in the state of extremely dependent and KPS score with 0 represented as dead (Willems, Taphoorn, Burger, Berkelbach van der Sprenkel, & Tulleken, 2006).
CD68 macrophages
The bone marrow derived cells such as macrophages contribute towards the microglial brain population (Machein, Renninger, de Lima-Hahn, & Plate, 2003). The macrophage identified by using CD68 markers (Strik, Deininger, Frank, Schluesener, & Meyermann, 2001; Yi, et al., 2011).
Problem Statement
The central nervous system tumours, astrocytic glioma are typically classified into four stages according to WHO classification. The pilocytic (grade I), diffuse (grade II), anaplastic (grade III) and glioblastoma multiforme (GBM) (grade IV) (Okada, 2009). The medulloblastoma are malignant, invasive embryonal tumour of the cerebellum and classified with several subtypes such as (1) desmoplastic types, (2) medulloblastoma with extensive nodularity, (3) large-cell variant and (4) anaplastic medulloblastoma. The meningioma arises from a layer of tissue (the meninges) that covers the brain and spine. The tumour classified into 3 grades, grade (I) beningn meningioma, grade II Atypical meningioma and grade III malignant or anaplastic meningioma (Louis, et al., 2007).Dysregulation of the hypothalamic-pituitary-adrenal axis, especially diurnal variation in cortisol and melatonin were the mechanisms of psychophysiological linking the depression. The effected immune system by depression plausibly affects resistance to tumor progression in the patients (Spiegel & Giese-Davis, 2003).
Validation of BI score has been done with neurological disability patients. BI measure the activities of daily living functional performance score. Initially the BI was developed for patient with chronic neurological impairment especially the stroke patients. The study showed that the BI that was verbally administered are easy to use, reliable and sensitive to change and has its prognostic value. The questionnaire was also suitable to be used among the glioma patients to evaluate the treatment and functional performance. Patients classified under severe disability have either transient improvement or gradual declining in BI score. KPS questionnaire has its neurological elements and it is also suitable to be used among the glioma patients. Both questionnaires can be administered via telephone or general practitioner or carer to get an accurate result especially when the patients unable to attend a clinic or not mobile (Brazil, et al., 1997).
The macrophage known as immune cell types that function in indentifying the foreign particles and maintaining the tissue homeostasis. The macrophages react with injury responses and involved in repairing the injury (Pinto, Godwin, & Rosenthal, 2014). Glioma infiltrating marcrophages produces IL-12, a CD81 T-cell-stimulating cytokine. The macrophages of human gliomas act as a predominant immune subset. The macrophages secrete cytokines, up regulate costimulatory molecules and activate antitumor effectors T cells. The regulatory T cells might play role in suppressing effective immune activity against malignant human gliomas (Hussain, et al., 2006).
Research Questions
A review of the literature uncovered no studies on this topic in Malaysian patients with brain tumour diagnosis, however studies have been done among the other cancer diagnosis such as Malaysian breast cancer patients (Yusoff, Low, & Yip, 2009) and cancer patients who were undergoing chemotherapy treatment (Zainal, Hui, Hang, & Anita, 2007). Therefore, it is hoped that this study will provide a more concrete understanding about the depression, functional and physical performance of patients with brain tumour and help mental health professionals and hospital administrators consider how to best staff clinics to effectively treat the psychological problems of these patients.
Purpose of the Study
The significance of the study will show that the patients not only suffer from the disease, but are also at risk of developing psychiatric disorders. The patients should not be neglected because the disease seriously impacts their emotional and physical status ( Johnsen, Petersen, Pedersen, & Groenvold, 2009; Pamuk, et al., 2008).
Research Methods
Study location
The study conducted at Hospital Kuala Lumpur (HKL) (n=100) and Hospital Universiti Sains Malaysia (HUSM) (n=22). The HKL and HUSM hospital is a referral centre for brain tumour cases.
Study design
A cross sectional and prospective cohort study design.
Sample population
The study population consisted of all intracranial tumour or brain disorder patients who visits neurosurgery clinic during the sampling period of the study and fulfilled the inclusion criteria.
Inclusion criteria
The participants were selected based on four main inclusion criteria. First, the participants must be diagnosed with intracranial tumour or brain disorder. All stages of intracranial tumour or brain disorder patients with good conscious level were included in the study. Second, the age of the participant must be at least 18 years. Finally, the participants in the study should be able to understand Malay, English, Mandarin or Tamil.
Exclusion criteria
There are some exclusion criteria to be considered in this study in order to prevent biases. First, participants will be excluded from the study if the patient wants to withdraw from the study. Second, if participants who are mentally disabled such as mentally distorted will be eliminated from the study. Third, participants with pain and not able to respond and requires immediate treatment also will be excluded.
Ethics approval
Ethics approval sought from the Human Research Committee of Universiti Sains Malaysia (JEPeM) and Medical Research & Ethics Committee (MREC) at the Ministry of Health (MOH), Malaysia before starting the study. The study approved by Human Research Ethics Committee, Universiti Sains Malaysia (FWA Reg No: 00007718; IRB Reg. No: 00004494) (USM/JEPeM/16050178) and Medical Research & Ethics Committee (MREC) from the Ministry of Health (MOH) (NMRR-16-1134-29874 (IIR).
MINI questionnaires
MINI questionnaires assessed psychiatric disorders such as MDD (Sheehan, et al., 2009). Many previous studies used various sets of questionnaires to screen for psychiatric disorders such as depression; (Pamuk, et al., 2008) however, only few studies had implemented a strict systematic clinical interview based on criteria to make such diagnoses in cancer patients (Hosaka, et al., 1994; Prieto, et al., 2005). In the present study, module A of the MINI International Neuropsychiatric Interview (MINI), version 6.0.0, questionnaire (Sheehan, et al., 2009) was used to diagnose MDD.
Karnofsky Performance Scale Index
The KPS Index measures the functional impairment of the patients. This scale score that varies from 0 to 100 % can be used to compare the effectiveness of treatments and prognosis in the patients. The lower the Karnofsky score, the worse the survival for most serious illnesses (Crooks, 1991; de Haan R, 1993; Hollen, 1994; Oxford Textbook of Palliative Medicine, Oxford University Press," 1993; Schag, 1984; Toole, 1991).
Barthel Index
The activities of daily living of the patients were measured using BI that comprises of 10 domains. These domains were arranged in an ascending order of difficulty (Klein, et al., 2001). The BI assesses the person's daily functioning on daily living activities and mobility. This includes feeding, moving from wheelchair to bed and return, grooming, transferring to and from a toilet, bathing, walking on level surface, going up and down stairs, dressing, continence of bowels and bladder. The scale score varies from 0 to 100 (Mahoney, 1965). The BI questionnaire administered among the glioma patients to evaluate the palliative effectiveness of treatment in the patients. The BI is also a reliable assessment of physical function and sensitive to change and is of prognostic value. Repeated measurement can be done to evaluate the physical disabilities as well as effectiveness of the treatment. (Brazil, et al., 1997).In the current study, the glioma patients were followed up during the pre-surgery and (3rd and 6th month) post-surgery to assess their physical and functional performance. The telephone interview and review of .
ELISA CD68
Plasma concentration of CD68 was quantitatively determined by using CD68 Elisa kit (Cusabio Biotech Co., Ltd). The standard prepared with known concentration. The standard vial was centrifuged at 6000 rpm for 30 s. The standard reconstituted with 1.0 ml of sample diluents. This reconstitution produces a stock solution of 1000 pg/ml for CD68 marker. The standard was allowed to sit for a minimum of 15 minutes with gentle and uniform agitation by pipette with 1 ml measuring range prior to making serial dilutions. The serial dilutions were performed by 250 ul of sample diluents added to 1.5 ml microcentrifuge tubes and mixed with 250 ul of standard stock solution of CD68. The series of dilutions were prepared for the concentration of (1000 pg/ml, 500 pg/ml, 250 pg/ml, 125 pg/ml, 31.25 pg/ml, and 15.63 pg/ml) for CD68 marker. The blank sample added with sample diluents for 0 ng/ml concentration.
250 μl of Sample Diluent into each tube (S0-S7) was pipetted. The stock solution to produce a 2-fold dilution series (as shown below, Figure
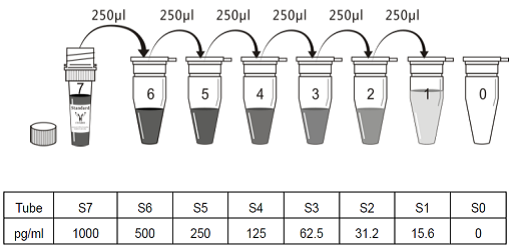
The undiluted standard serves as the high standard with 1000 pg/ml for CD68 concentration and the sample diluents serves as zero standard with 0 pg/ml concentration. The standard preparation was used within 4 hours and was discarded after use.
After the standard dilution steps, 100ul of these standards and samples were added into each of a pair of adjacent wells. The covered wells were incubated for 2 hours at 37 °C. Then, the liquid from each well was removed without washing. Then 100 ul of Biotin-antibody working solution of each well was added and incubated for 1 hour at 37 °C. After incubation, the wells were washed for three times. The 200 ul of wash buffer was added and let stand for 2 minutes, then the liquid was removed by flicking the plate on a paper towel. The HRP-avidin working solution (100 ul) was added to each well, the microtiter plate covered with new adhesive strip and incubated for 1 hour at 370C. The wells were washed again for five times. 90ul of TMB substrate was added to each well and incubated for 10-30 minutes at 370C. The plate was kept away from drafts and other temperature fluctuations in the dark. Finally 50 ul of stop solution was added to each well and the optical density of each well within 30 minutes was determined by using a microplate reader set to 450 nm.
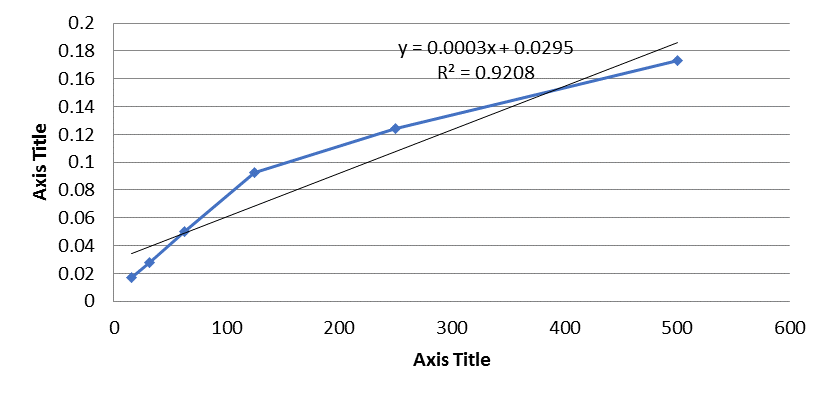
The duplicate reading for each standard, control and sample were averaged and subtracted with the average zero standard optical density. The standard curve was then plotted.
Findings
Neurological brain tumor or brain disorder patients
This study took place at Hospital Kuala Lumpur Malaysia (HKL) and Hospital Universiti Sains Malaysia (HUSM).
A total of 122 patients from HKL were approached in the study. However 22 patients were excluded from the study, this comprise of patient with age 12 years old (n=2), 13 years old (n=1), 15 years old (n=2), 16 years old (n=4), 17 years old (n=1), patients with other diagnosis (n=3) and patients who withdraw or incompleted the study (n=9). The calculated sample size was 107 patients therefore, the study had a response rate of 93.5% (n=100). The 100 patients in HKL who were identified with intracranial tumour or brain disorder by radiological appearance with subsequent histological confirmation based on WHO grade were included in the study. All the patients were recruited between (April 2016 to December 2016) for neurological brain tumor or brain disorder patients.
Table I shows the characteristics of the respondents. The mean age of the neurological disorder participants was 45.3 years (95% CI=42.6, 47.9). The mean age of men (43.6 years, 95% CI = 39.4, 47.8) not significantly different from mean age of women (46.1 years, 95% CI = 42.7, 49.5) who participated in this study (Z = -0.993, p=0.321) (Table
Clinical characteristics of neurological brain tumour or brain disorder patients in HKL
Table
Astrocytic glioma patients in HUSM
The study also took place at Hospital Universiti Sains Malaysia (HUSM), School of Health Sciences, USM and School of Medical Sciences, USM. All patients were admitted between (2012-2014) in the HUSM. The prospective cohort study includes a total of 22 patients who were identified with astrocytic gliomas by radiological appearance with subsequent histological confirmation based on WHO grade were included in the study. The patients were consented and assessed with KPS and BI questionnaires to measure the changes in functional and physical performance of patients over time (pre-surgery, 3 and 6 months post-surgery). The socio-demographic and clinical characteristics of respondents are displayed in Table III and IV. Twenty-one patients were Malay (95.45%) and one patient was Chinese (4.55%). The mean age of the patients that recruited in HUSM was 44.18 years (6 years-71 years). Of these, 16 patients were male (72.7%) and 6 patients were female (27.3%). The mean age of male patients was 43.81 years and the mean age of female patients was 45.17 years (Table
Clinical Characteristics of Astrocytic Glioma Patients in HUSM
The types of astrocytic glioma patient’s diagnosis that were included in the study were pilocytic astrocytoma, diffuse astrocytoma, anaplastic astrocytoma, anaplastic oligodendroglioma, anaplastic ependymoma, anaplastic gemistocytic astrocytoma, glioblastoma with oligodendroglioma component, gliosarcoma and glioblastoma multiformae. Among 22 patients diagnosed with astrocytic glioma, 9 patients (40.9%) were stage IV, 8 patients (36.4%) were stage III, 2 patients (9.1%) were stage II and 3 patients (13.6%) were stage I. The clinical characteristics of patients are displayed in Table IV. Their blood specimenwas obtained for CD68 macrophage analysis (Table
Prevalence of psychiatric disorders among the brain tumour or brain disorder patients in HKL
The prevalence of MDD in the neurological disorder patients was 30%. From the 100 respondents, 30% (n=30) were diagnosed with MDD. Of 30 respondents, 50% (n=15) were diagnosed with a current, past and recurrent episode of MDD and 30% each were determined to have a current and a past episode (n=9) and past episode, 10% (n=3), current episode 6.67 % (n=2) and past and recurrent 3.33% (n=1). The severities of MDD were shown in (Table
Additionally, this study found a slightly higher prevalence of MDD in female compared to male respondents at 56.7% and 43.3% respectively. Among the depressed respondents, there was a higher preponderance of Malays (80.0%), followed by Indians (16.7%) and other ethnic groups (3.3%). There was a high proportion of depressed respondents who were married (80.0%), achieved an educational level of SPM/SPMV/MCE or less (66.7%), were not working (53.3%) and had children (70.0%). However, no significant difference was found between depressed patients and gender, time since diagnosis, ethnicity, religion, marital status, children status, highest level of formal education, highest certificate obtained, occupational status, working sector or monthly income.
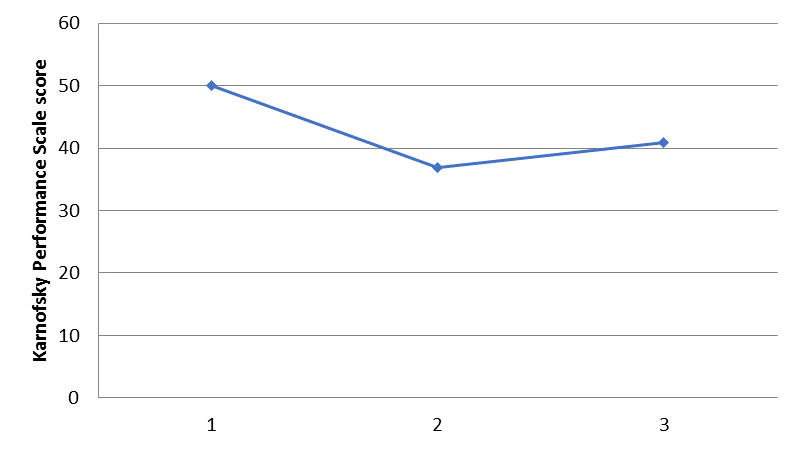
Karnofsky Performance Scale (KPS) score of the patients
During the follow up of 3rd month and 6th month after surgery it was found that 8 patients died and 14 patients survived. The mean KPS score of the patients before the surgery was 50 ± 9.76; at the third month of post surgery was 36.82 ± 30.14 and at 6th month of follow-up was 40.91 ± 33.51 (Figure
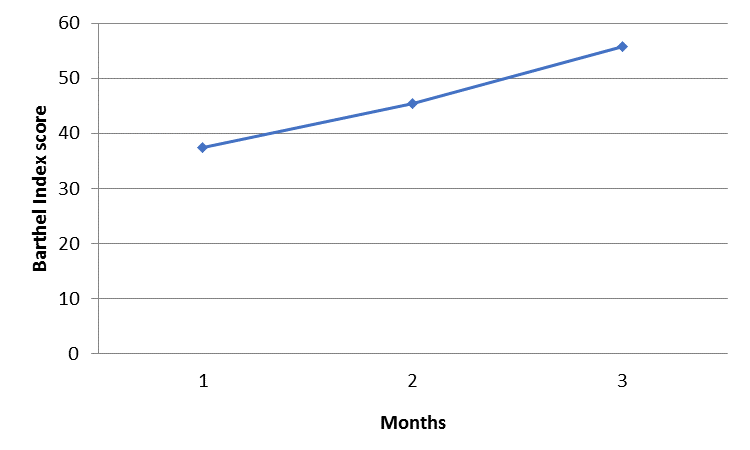
Barthel Index (BI) Score of the Patients
The overall mean BI score in the study was 37.5 ± 29.14 before the surgery, at the third month of post surgery was 45.36 ± 29.58 and at 6th month of follow-up was 55.71 ± 31.37 (Figure
Karnofsky Performance Scale score and Barthel Index Score of the Patients
The KPS score correlated with BI score that was measured before the surgery (Spearman’s rho, r = 0.605, p = 0.003) Figure
BI score before surgery correlated with 3rd month BI score (Spearman’s rho r = 0.631; p = 0.015) Figure


Inflammatory Cells (Macrophages) in Astrocytic Glioma#
The inflammatory cell (macrophages) in astrocytic glioma was investigated. The OD of each well was determined by using a microplate reader set to 450 nm wavelength. The duplicate reading for each standard, control and sample were averaged and subtracted with the average zero standard OD (Table
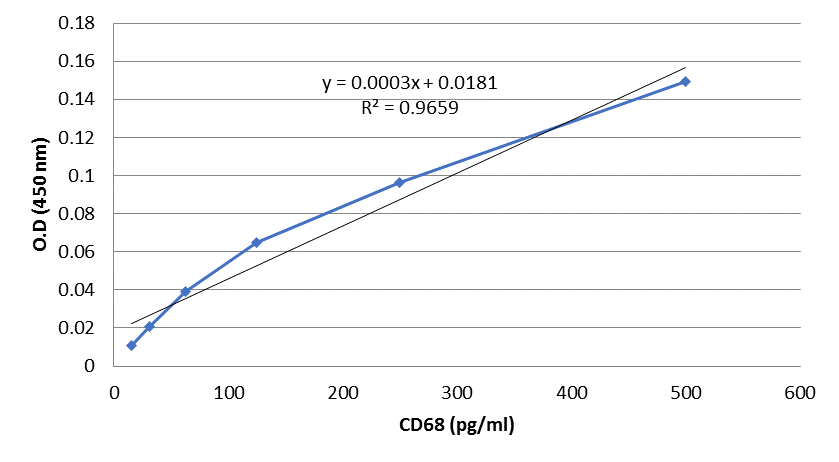
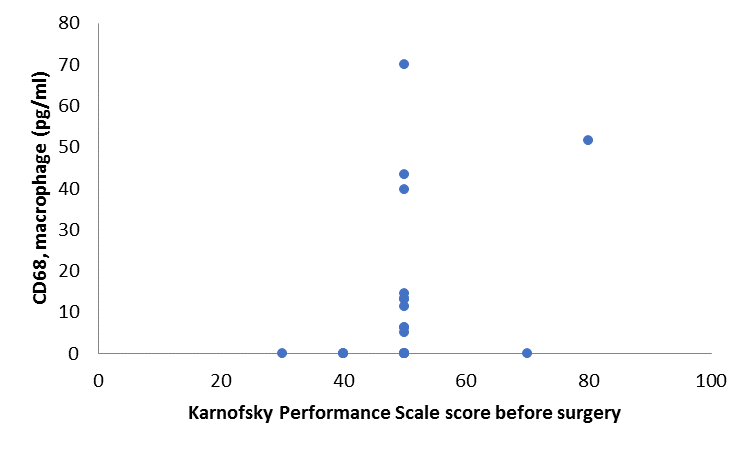
Karnofsky Performance Scale score relationship with CD68 macrophages, inflammatory cells of the Patients
The KPS score before the surgery is marginally correlated with CD68 with positive association but the result is not significant at p<0.005 (Spearman’s rho, r = 0.41, p = 0.061) Figure
Discussion
To our knowledge, this study is the first study which reports on MDD among Malaysian neurological brain disorder patients. The present study showed that the prevalence of MDD among neurological brain disorder patients was 30.0%. The prevalence that found in the current study was comparable with the study done by Wellisch et al., who found that the overall prevalence of MDD was 28.0% in the brain tumour patients (Wellisch, Kaleita, Freeman, Cloughesy, & Goldman, 2002). Of 30.0% respondents with MDD, 6.67% had severe MDD and the comparison of severity of depression is difficult because different severity scales were used in the previous studies.
Depression among cancer patients were determined based on many research studies. The socio-demographic factors such as age (Johnsen, Tholstrup, Petersen, Pedersen, & Groenvold, 2009), gender (Deimling, Bowman, Sterns, Wagner, & Kahana, 2006; Prieto, et al., 2004) and education level (Deimling, et al., 2006) have significanteffect on depression. Clinical parameters such as type of cancer (Deimling, et al., 2006) and its treatment (Deimling, et al., 2006; Liu, et al., 2009; Waljee, et al., 2008; Yen, et al., 2006), severity of the diagnosis(Dodd, Cho, Cooper, & Miaskowski, 2010; Liu, et al., 2009; Marylin, Maria, Bruce, & Christine, 2010), disease stage (Yen, et al., 2006) and illness duration (Prieto, et al., 2004) were also found to be associated with the depression. Other factors such as psychosocial factors like physical (Fann, et al., 2009; A. T. Johnsen, et al., 2009; Pamuk, et al., 2008) functioning also found to be correlated with the depression. In this study, there was a preponderance of female respondents with MDD (56.7%) compared to male respondents. This finding shows similar results from a previous study which found that female patients have higher depression compared to male patients (Deimling, et al., 2006; Prieto, et al., 2004). However, our finding was in contrast with other study, which found that men scored higher in depression measures compared to women (Pandey, et al., 2006). The respondents of this study represent all three predominant ethnicities of the Malaysian population, and the proportion of each ethnicity was consistent with reported proportions in the national cancer registry in 2006 (Ariffin Omar Zainal, Mohd. Ali Zainudin, & Ibrahim Tamin Nor Saleha, 2006). Among the various ethnic groups in Malaysia, the prevalence of MDD was alarmingly high in the Malays (80.0%), followed by Indians (16.7%) and other ethnic groups (3.3%).
The current study also found that most of the patients with depression were married (80.0%) and had an education level of SPM/SPMV/MCE or less (66.7%). The higher rates of MDD in the married respondents were in contrast with the study by Staci et al., who found that the married patients were less depressed compared to the unmarried patients. The prevalence of MDD in respondents with low educational level was expected and similar to that in another study that found less educated patients were more depressed compared to others (Arnold, et al., 2008). There was a high preponderance of respondents who were not working (53.3%) who were diagnosed with MDD. This is consistent with a study that found that higher distress cancer patients were from lower income group (Carlson, et al., 2004). Patients with children (70.0%) were found to be more depressed in the present study. However the comparison with other studies is difficult because limited research has been done in order to investigate this factor.
However, MDD diagnosis with these certain clinical and socio-demographic factors did not yield any significant results. Moreover other studies among the cancer patients also found there is no significant association between depression and socio-demographic profiles (Mishra, Mohapatra, Bhattacharya, Gupta, & Agarwal, 2006). The reason for non-significant result might be due to the unequal number of sample size in each parameter of the studies.
The previous study proposed that BI scores of 0 - 20 indicate "total" dependency, 21 - 60 indicate "severe" dependency, 61 - 90 indicate "moderate" dependency, and 91 - 99 indicates "slight" dependency(Ploughman, et al., 2014). In this study it was found that 22.7% with total dependency, 50% with severe dependency, 22.7% with moderate dependency and 4.5% with slight dependency. The finding indicates that most of the patients are functionally dependent before the surgery; however the BI score improved over time at 3rd and 6th month of post surgery in this study. The patients with total dependency reduced to 14.3% at the 6th month of post surgery compared to 21.4% at 3rd month of post surgery and 22.7% before the surgery and KPS score correlated with BI score before the surgery, at third month of surgery and 6th month of surgery. Moreover the BI score before the surgery have positive correlation with 3rd month surgery BI score with 6th month of surgery BI score. The 3rd month of surgery KPS score correlated with 6th month of surgery KPS score. The finding indicates that both BI score and KPS score increased over time with significant associations. A study has been done among the high grade glioma patients that were treated in radiotherapy by administering BI questionnaire for the measurement of their functional status. The questionnaire has been validated among the neurological disability patients and about 504 occasions in 107 patients were included in the study. Among the 71 patients, 57.7% indicates functionally independent, 26.8% showed moderate disability and 15.5% patients with severe disability. The study found that BI score was associated with KPS score which measure the prognostic information score (KPS) R2 = 0.872 (Brazil, et al., 1997).
In a study among the low grade gliomas young patients showed that the BI score was lower than normal score before the treatment of radiotherapy. The lower BI score might be because of tumour and surgery related factors. However during follow up at second and third year showed that the mean score of BI does not decrease. Mean BI score at 6 months was 97.7, 2 years (97.1) and 3 years (99). The mean individual BI scores were improved up to 2 years and not reduced at second and third year of follow-up and the entities includes in personal hygiene, self bathing, feeding, toilet, stair climbing, dressing, bowel control, bladder control, ambulation, and chair–bed transfer. This improvement was noticed in chair bed transfer ambulation (0.66), and stair climbing (0.75) feeding score (1.25), bathing score (0.75) and dressing score (1.08)(Jalali, et al., 2008). This finding in consistence with current finding that showed similar result in which BI score does not decrease but improved at follow-up of 3rd and 6th month as the mean BI score was [37.5(29.14)] before the surgery, at the third month of post surgery was [45.36(29.58)] and at 6th month of follow-up was [55.71(31.37)].
In the previous study it has been shown a significant improvement in the BI score that was observed in visually handicapped patients, patients with poor performance status, and younger patients. That patient who had relapse of tumour showed significant lower BI score at baseline compared to other patients. The patients total BI mean score at pre- radiotherapy at baseline was 94.5 (SD 14.8, range 45–100) while individual BI mean scores at baseline in personal hygiene was (4.6), self bathing (4.7), feeding (9.4), toilet (9.3), stair climbing (9.3), dressing (9.4), bowel control (9.7), bladder control (9.7), ambulation (14.2), and chair bed transfer (14.1) in low grade glioma patients . BI score at baseline was significantly low in patients with low performance status. The selfbathing, personal hygiene, dressing, and stair climbing were also affected but the bladder and bowel functions were maintained in most patients (Jalali, et al., 2008). However, in the current study it was found that the mean BI score was much lower as [37.5(29.14)] scores was found before the surgery that might be because of higher grade glioma patients who are facing functional disability were included in the study. In term of BI mean scores in feeding was (4.32), self bathing (1.14), grooming (2.05), dressing (3.18), bowels control (6.36), bladder control (6.14), toilet use (4.55), transfers (6.36), mobility (5.23), and stairs (2.27) were found before the surgery. The BI mean scores at third month of follow up in feeding was (4.29), self bathing (1.43), grooming (2.14), dressing (4.64), bowels control (6.43), bladder control (6.07), toilet use (5.00), transfers (6.79), mobility (6.43), and stairs (2.14). The BI mean scores at sixth month of follow up in feeding was (4.64), self bathing (2.14), grooming (3.93), dressing (5.36), bowels control (7.14), bladder control (6.79), toilet use (6.07), transfers (7.86), mobility (8.21), and stairs (3.57). In this study, it was found that self bathing, grooming, bowel control, toilet use, transfer and mobility are improved over time in the glioma patients.The previous study suggests that radiotherapy treatment or surgical intervention or both may play a role in poor scores of BI (Jalali, et al., 2008).
In the current study the mean KPS score of the patients before the surgery was 50±9.76; at the third month of post surgery [36.82(30.14)] and at 6th month [40.91(33.51)] were found in this study. The KPS score of the patients reduced after the surgery however the KPS improved at the 6th month of post-surgery in this study. In the previous study among the high grade glioma and non small lung cancer patients, the functional status of the individual patients were evaluated using KPS score which measure the level of physical functioning that range from 0, the lowest level to the highest level of 100 score. The study indicates the importance of evaluating the patient with cancer impact and their treatment by considering their functional status. The result showed that the KPS score and BI score of glioma patients were much reduced compared to patient with non small lung cancer. The score of KPS for glioma patients was [76.7(17.1)] and BI was [16.9(2.4)] vs non small lung cancer patients with KPS score of [82.4(17.3)] and BI with [17.8(2.1)] score (Klein, et al., 2001).
In a study among 195 low grade glioma patients it has been found that the BI score after diagnosis at mean of 6 years was [19.6(1.5)], and KPS score was 88.0± 14.7 (n=130). Among 65 patients, after 12 years the BI score was 19.9±0.4 and KPS score was [88.3(13.2)] at 6 years and at 12 years the BI score was [19.2(3.0)] with KPS score was [85.3 (17.6)]. The study also found that the patients who undergone radiotherapy treatment have reduced BI and KPS score compared to patients without the treatments. Therefore the treatment of glioma should be considered the risk of long term effect of radiotherapy when the treatment is planned (Douw, et al., 2009). In another study, the patients with glioma were evaluated for their KPS score and BI score before the surgery and 3 months after the surgery by comparing two different types of surgery which are standard surgery and surgery with the aid of neuronavigation. At the time of inclusion of the study the patient in the group of standard surgery showed KPS [78.6(15.5)] with median 80 and BI [18.1(4.1)] with median 20 score and patient in the group of neuronavigation showed KPS [77.4(19.4)] with median 80 and BI [17.4(5.0)] with 20 median score. During the 3 months of postsurgery about 77.4% patients were still alive showed that patient who undergone neuronavigation surgery showed better score in both KPS and BI score compared to patient who undergone standard surgery (Willems, et al., 2006).
The macrophages involved in the inflammation to eradicate the brain tumour (Farzana, 2006; Strojnik, et al., 2009; Thomas Wirth, 2012). The current study found marginal non significant positive association between KPS score and macrophage before the surgery. The results predict more recruitment of macrophages associates with the better KPS score in these astrocytic glioma patients. Therefore the treatment by considering patient’s BI and KPS score in relation to macrophage level will be an alternative approach in treating the patients with astrocytic glioma. This will contribute to cost-effective treatment in the brain tumour oncology setting
Conclusion
The depression among the brain tumor or brain disorder patients was high. BI score was significantly increased with KPS score. BI score showed improvement during the 3rd and 6th month follow-up.Therefore targeting these parameters might improve the overall treatment of the patients.
Acknowledgments
The study supported by Universiti Sains Malaysia short term grant 304/PPSK/61312016 , 304/PPSP/6315007 and Priscilla Das is a holder of MyBrain15-MyPhd scholarship.
References
- Psychiatric, American. (2000). Association: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edditon, Text Revision.: Washington, Dc, American Psychiatric Association,
- Arnold, S D.Forman, L M.Brigidi, B D.Carter, K E.Schweitzer, H A.Quinn, H E. (2008). Evaluation and characterization of generalized anxiety and depression in patients with primary brain tumors.. NEURO ONCOL,, 40(2), 171-181
- Brazil, L.Thomas, R.Laing, R.Hines, F.Guerrero, D.Ashley, S. (1997). Verbally administered Barthel Index as functional assessment in brain tumour patients.. J Neurooncol,, 40(2), 187-192
- Carlson, L E.Angen, M.Cullum, J.Goodey, E.Koopmans, J.Lamont, L. (2004). High levels of untreated distress and fatigue in cancer patients.. Br J Cancer,, 40(12), 2297-2304
- Crooks, V.Waller, S. (1991). The use of the Karnofsky Performance Scale in determining outcomes and risk in geriatric outpatients., 144-
- Haan, R de.A, . (1993). Measuring quality of life in stroke.. Stroke,, 40, 320-327
- Deimling, G T.Bowman, K F.Sterns, S.Wagner, L J.Kahana, B. (2006). Cancer-related health worries and psychological distress among older adult, long-term cancer survivors.. Psycho-Oncology,, 40(4), 306-320
- Dodd, M J.Cho, M H.Cooper, B A.Miaskowski, C. (2010). The effect of symptom clusters on functional status and quality of life in women with breast cancer. European journal of oncology nursing : the official journal of European Oncology Nursing Society,, 40(2), 101-110
- Douw, L.Klein, M.Fagel, S S.Heuvel, J van den.Taphoorn, M J.Aaronson, N K. (2009). Cognitive and radiological effects of radiotherapy in patients with low-grade glioma: long-term follow-up.. Lancet Neurol,, 40(9), 810-818
- Fann, J R.Berry, D L.Wolpin, S.Austin-Seymour, M.Bush, N.Halpenny, B. (2009). Depression screening using the Patient Health Questionnaire-9 administered on a touch screen computer.. Psycho-Oncology,, 40(1), 14-22
- Farzana, H S.Yang, David.Suki, Dima.Aldape, Kenneth.Grimm, Elizabeth.Heimberger, Amy B. (2006). The role of human glioma-infiltrating microglia/macrophages in mediating
- (2006). antitumor immune responses.. Neuro-oncol., 40(3), 261-279
- PJ, Hollen.R, G. (1994). Measurement of quality of life in patients with lung cancer in multicenter trials of new therapies.. Cancer.,, 40, 2087-2098
- Hussain, S F.Yang, D.Suki, D.Aldape, K.Grimm, E.Heimberger, A B. (2006). The role of human glioma-infiltrating microglia/macrophages in mediating antitumor immune responses.. Neuro-Oncology,, 40(3), 261-279
- Jalali, R.Dutta, D.Kamble, R.Gupta, T.Munshi, A.Sarin, R. (2008). Prospective assessment of activities of daily living using modified Barthel's Index in children and young adults with low-grade gliomas treated with stereotactic conformal radiotherapy.. J Neurooncol,, 40(3), 321-328
- Johnsen, A.Petersen, M.Pedersen, L.Groenvold, M. (2009). Symptoms and problems in a nationally representative sample of advanced cancer patients.. Palliative Medicine,, 40(6), 491-501
- Johnsen, A T.Tholstrup, D.Petersen, M A.Pedersen, L.Groenvold, M. (2009). Health related quality of life in a nationally representative sample of haematological patients.. European Journal of Haematology,, 40(2), 139-148
- Klein, M.Taphoorn, M J.Heimans, J J.Ploeg, H M van der.Vandertop, W P.Smit, E F. (2001). Neurobehavioral status and health-related quality of life in newly diagnosed high-grade glioma patients. J Clin Oncol,, 4037-4047
- Lim, G.Rampal, S.Halimah, Y. (2008). Cancer incidence in Penisular Malaysia,
- Liu, L.Fiorentino, L.Natarajan, L.Parker, B A.Mills, P J.Sadler, G R. (2009). Pre-treatment symptom cluster in breast cancer patients is associated with worse sleep, fatigue and depression during chemotherapy.. Psycho-Oncology,, 40(2), 187-194
- Louis, D N.Ohgaki, H.Wiestler, O D.Cavenee, W K.Burger, P C.Jouvet, A. (2007). WHO classification of tumours of the central nervous system., 40(2), 97-109
- Machein, M R.Renninger, S.Lima-Hahn, E de.Plate, K H. (2003). Minor contribution of bone marrow-derived endothelial progenitors to the vascularization of murine gliomas.. Brain Pathol,, 40(4), 582-597
- FI, Mahoney.D, B. (1965). Functional evaluation: the Barthel Index. Maryland State Med Journal, 40, 56-61
- Marylin, J D.Maria, H C.Bruce, A C.Christine, M. (2010). The effect of symptom clusters on functional status and quality of life in women with breast cancer. European journal of oncology nursing : the official journal of European Oncology Nursing Society,, 40(2), 101-110
- Mishra, S K.Mohapatra, P K.Bhattacharya, K.Gupta, T.Agarwal, J P. (2006). Prevalence of psychiatric disorder in asymptomatic or minimally symptomatic cancer patients on treatment.. Journal Of Cancer Research And Therapeutics,, 40(3), 136-139
- Okada, H.G, K.Zhu, X.Kastenhuber, E R.Hoji, A.Ueda, R.Fujita, M. (2009). Immunotherapeutic approaches for glioma. Critical Reviews in. Immunology, 40(1), 1-42
- Oxford, . (1993). Textbook of Palliative Medicine,, 109-
- Pamuk, G E.Harmandar, F.Ermantaş, N.Harmandar, O.Turgut, B.Demir, M. (2008). EORTC QLQ-C30 assessment in Turkish patients with hematological malignancies: association with anxiety and depression.. Annals of Hematology,, 40(4), 305-310
- Pandey, M.Sarita, G.Devi, N.Thomas, B.Hussain, B.Krishnan, R. (2006). Distress, anxiety, and depression in cancer patients undergoing chemotherapy.. World Journal of Surgical Oncology,, 40(1), 68-
- Pinto, A R.Godwin, J W.Rosenthal, N A. (2014). Macrophages in cardiac homeostasis, injury responses and progenitor cell mobilisation.. Stem Cell Research, 13(3, Part B),, 705-714
- Ploughman, M.Beaulieu, S.Harris, C.Hogan, S.Manning, O J.Alderdice, P W. (2014). The Canadian survey of health, lifestyle and ageing with multiple sclerosis: methodology and initial results.. BMJ Open,, 40(7)
- Prieto, J M.Atala, J.Blanch, J.Carreras, E.Rovira, M.Cirera, E. (2004). Patient-rated emotional and physical functioning among hematologic cancer patients during hospitalization for stem-cell transplantation.. Bone Marrow Transplant,, 40(3), 307-314
- CC, Schag.R, H.PA, Ganz. (1984). Karnofsky performance status revisited: Reliability, validity, and guidelines.. J Clin Oncology. ,, 40, 187-193
- Schlag, P M.J, S H. (2009). Gliomas. . Cancer Research, 1-259
- Harnett-Sheehan, K J.Sheehan, M.Gray, C.Leucrubier, Y. (2009). M.I.N.I Mini International Neuropsychiatric Interview Version, 40, DSM-IV.-
- Spiegel, D.Giese-Davis, J. (2003). Depression and cancer: mechanisms and disease progression.. Biol Psychiatry,, 40(3), 269-282
- Strik, H.Deininger, M.Frank, B.Schluesener, H.Meyermann, R. (2001). Galectin-3: Cellular Distribution and Correlation with WHO-grade in Human Gliomas.. Journal of Neuro-Oncology,, 40(1), 13-20
- Strojnik, T.Kavalar, R.Zajc, I.Diamandis, E P.Oikomomopoulou, K.Lah, T T. (2009). Prognostic Impact of CD68 and Kallikrein 6 in Human Glioma. Anticancer Research,, 40(8), 3269-3279
- Wirth, Thomas.A, F. (2012). Agnieszka Pacholska, aritha Samaranayake and Seppo Ylä- erttuala.
- DM, Toole.A, G. (1991). Evaluating cancer patients for rehabilitation potential., 155-384
- Waljee, J F.Hu, E S.Ubel, P A.Smith, D M.Newman, L A.Alderman, A K. (2008). Effect of esthetic outcome after breast-conserving surgery on psychosocial functioning and quality of life.. Journal of Clinical Oncology,, 40(20), 3331-3337
- Wellisch, D K.Kaleita, T A.Freeman, D.Cloughesy, T.Goldman, J. (2002). Predicting major depression in brain tumor patients.. Psychooncology,, 40(3), 230-238
- Willems, P W.Taphoorn, M J.Burger, H.Sprenkel, Berkelbach van der.W, J.Tulleken, C A. (2006). Effectiveness of neuronavigation in resecting solitary intracerebral contrast-enhancing tumors: a randomized controlled trial.. J Neurosurg,, 40(3), 360-368
- Yen, J-Y.KO, C-H.YEN, C-F.YANG, M-J.WU, C-Y.JUAN, C-H. (2006). Quality of life, depression, and stress in breast cancer women outpatients receiving active therapy in Taiwan. Psychiatry and Clinical Neurosciences,, 40(2), 147-153
- Yi, L.Xiao, H.Xu, M.Ye, X.Hu, J.Li, F. (2011). Glioma-initiating cells: a predominant role in microglia/macrophages tropism to glioma.. J Neuroimmunol,, 40(1), 75-82
- Yusoff, N.Low, W.Yip, C. (2009). Reliability and validity of the malay version of brief cope scale: a study on malaysian women treated with adjuvant chemotherapy for breast cancer.. Malaysian Journal of Psychiatry,, 40
- Zainal, A O.Zainudin, M A.Saleha, Nor.T, I. (2006). Malaysian cancer statistics data and figure peninsular Malaysia.
- Zainal, A O.Zainudin, M A.Saleha, Nor.T, I. (2006). Malaysian cancer statistics data and figure peninsular Malaysia.
- Zainal, N.Hui, K.Hang, T.Anita, B. (2007). Prevalence of distress in cancer patients undergoing chemotherapy.. Asia-Pacific Journal of Clinical Oncology,, 40(4), 219-223
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
01 May 2018
Article Doi
eBook ISBN
978-1-80296-039-6
Publisher
Future Academy
Volume
40
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-1231
Subjects
Business, innovation, sustainability, environment, green business, environmental issues
Cite this article as:
Das, P., Naing, N. N., Wan-Arfah, N., Noorjan, K., Kueh, Y. C., & Rasalingam, K. (2018). Major Depressive Disorder, Functional And Physical Performances Of Malaysian Brain Tumour Patients. In M. Imran Qureshi (Ed.), Technology & Society: A Multidisciplinary Pathway for Sustainable Development, vol 40. European Proceedings of Social and Behavioural Sciences (pp. 501-524). Future Academy. https://doi.org/10.15405/epsbs.2018.05.40

