Abstract
Hemiplegia is a pure pyramidal syndrome affecting 30% of all cerebral palsy, the patients having asymmetric gait, which is easy to classify in a particular pattern. The assessment and treatment systems of hemiplegic gait have evolved very quickly in the last years, defending the need for “upgrading” to increase and improve the rehabilitation of children with hemiplegia gait. We start from the question: what are the actualities in the assessment and treatment of gait disorders in children with hemiplegia? The research strategy of the articles focused on using key points to cover the established criteria fixed at the beginning. The main sources were: databases, books and journals, reports, conference papers, official and legal publications and reviews. The collected data aimed at the rehabilitation of gait disorders including methods and concepts of assessment and treatment that could be implemented in the profile centres existing in Romania. Experience in the field and the assessment methodology are the key factors in recovering the child’s hemiplegic gait. The functional evaluation determines the diagnosis and severity of the disorders that prevent the child from acquiring a normal gait. A consistent number of studies and papers describe methods and concepts, but the literature is poor in demonstrating their efficacy.
Keywords: Gait disordersphysiotherapyhemiplegiarehabilitation
Introduction
Cerebral palsy (CP) “describes a group of permanent disorders of the development of movement and posture, causing activity limitations, which are attributed non-progressive disturbances that occurred in the developing foetal or infant brain. The motor disorders of cerebral palsy are often accompanied by disturbances of sensation, perception, cognition, communication and/or behaviour, all as seizures and secondary musculoskeletal problems” (Rosenbaum et al., 2007).
Classification of cerebral palsies can be performed according to the following criteria: type of motor deficiency (spastic – the most common, hypotonic, dyskinetic and ataxic), number of affected limbs (hemiplegia, diplegia and tetraplegia) and severity of dysfunction (Rethlefsen, Ryan, & Kay, 2010). We will only limit to the hemiplegic form.
Cerebral palsy has a prevalence of 2-3 per 1,000 births and, according to a study made in the US, in 2008, there were identified 77.4% children with spasticity, 11.3% walking with a mobility device, while 30.6% had limited or no walking ability (Centers for Disease Control and Prevention, 2016). Of the total cases, 30% had the motor deficit distribution on a hemibody, according to the Surveillance of Cerebral Palsy in Europe (SCPE).
Hemiplegia is the motor sequelae characteristic to focal cerebral infarction, which occurs in 20-30% of children suffering from this type (Cioni & Mercuri, 2007).
The risk factors are: in most cases (85-90%), they are congenital; low or increased birth weight; prematurity and/or multiple pregnancy; infections during pregnancy or after birth: meningitis, malaria; jaundice; maternal medical conditions: thyroid disorder, metabolic disorders; birth complications: hypoxia, haemorrhages, infections; assisted reproduction technology; road accidents involving the mother.
The most common causes are: periventricular abnormalities of the white matter, cervical-subcortical lesions, brain malformations or non-progressive postnatal lesions (Wiklund & Uvebrant, 1991; Cioni et al., 1999).
Gait “is an alternative bipedalism, which involves a complex implication of automatic and voluntary postural components” (Onose & Pădure, 2008).
From the first day of life, a normal child “walks”. It is the so-called archaic reflex, “automatic walking” representing the integrity and maturation of the nervous system, being achieved by placing the newborn with the soles in contact with a rough plane in an orthostatic position, imparting a forward pushing motion. The motor response is to perform steps in a regular rhythm and to turn correctly on the soles. This reflex disappears at the end of the first six weeks. Another archaic reflex is “crossing the obstacle”, the only reflex that is not present at birth (it appears after the tenth day of life and disappears at about 9-10 weeks). (Mureșan, 2004)
The acquisition of gait occurs over time, starting around the age of 9-10 months and consolidating at the age of 14-15 months, after the child has grown up and strengthened his/her recovery, balance, postural and defence reflexes.
Hemiplegia is a subtype of brain paralysis that affects a hemibody.
Hemiplegia has the following general characteristics: upper limb is more affected than the lower one; motor control deficit is more distal than proximal; distribution of anti-gravitational hypertension; muscle spasticity affects normal growth of muscle and bone, resulting in both a decrease in the range of motion and the phenomenon of discrepancy (different limb lengths). At the level of lower limb, there is often a pelvic retraction, hip flexion, femoral anteversion, tibial torsion and equine foot. (Tecklin, 2015)
Spasticity is the most common neurological disorder in hemiplegia, resulting in an increase in the tonic reflex activity, with exaggerated overloads on the pyramidal pathway of alpha motoneurons. Reflex stretching or stretch reflex is a feedback mechanism for controlling the length of the muscle. In the lower limb, there are the adductors, internal rotators and hip extensors, knee extensors, plantar flexors and finger flexors. The effects of spasticity are: voluntary movement restriction, improper static posture of the legs and, in serious cases, the development of contractures (retractions). The most common spasticity assessment scale is the Ashworth Scale Modified.
Another cause that reduces the length of muscle fibre is long immobilisation. Usually, this is caused by the vicious positions that children adopt or how they are hold by their owners.
In hemiplegics, associated reactions or synkinesis occur when performing a voluntary movement with the healthy limb. An increase in spasticity of the diseased part is recorded. (Robănescu, 1983)
Muscle hypotonia occurs in the agonist muscle that is not sufficiently stimulated or strong due to excessive increase in the antagonist muscle tone, which may lead to retraction over time.
Bone and joint deformity is very common in cerebral palsy. In hemiplegia, we find the type of varus equine or valgus equine foot, genu flexum, genu valgum, genu recurvatum, knee contracture, rectus femoris retraction, hip dislocation, basal imbalance, lower limb discrepancy, etc. Most children with hemiplegia do not have cognitive impairment and manage to acquire the stages of neuromotor development with a smaller gap. For example, they will walk around the age of 18-24 months with a characteristic pattern. (Tecklin, 2015; Scrutton, Damiano, & Mayston, 2004)
The loss of balance in orthostatism and gait is an indispensable feature of the clinical picture of the hemiplegic patient. Many patients have problems with balance because they do not have the perception of the body.
Hemiplegic gait is characterised by:
The large support base that may be the cause of any deformation, instability or fear of falling, or the small support base due to the damage of adductor muscles or genu varum.
The length of the steps is different. Usually, the affected part does not exceed the healthy limb in the oscillating phase, then the length is zero, and if it does not catch the other, the value is negative.
The short oscillatory phase reduces the pitch on the other side. Once the foot reaches the ground, the oscillation phase is completed and, at the same time, the length and speed.
The patient tends to support on the healthier limb, thus reducing both of the phases.
The rhythm disorder, where the synchronisation is altered and may be asymmetrical or irregular due to sensory and proprioception loss.
The transfer of weight from one limb to the other is asymmetrical.
The shoulder is in retraction, and the pelvis is rotated behind. The upper limb balancing is only visible on the unaffected side. (Bondar et al., 2017, pp. 146-184)
By locomotion, man can move from one point to another, giving him independence. Over time, the hemiplegic rehabilitation process has progressed with new concepts, approaches, intervention strategies, robotisation of the rehabilitation process. Physiotherapy is the main discipline in the management of this deficiency (Craig, 1999; Anttila et al., 2008), and the therapist’s training is crucial. The best treatment is the one that adapts to the patient’s particularities and circumstances (family, society, school).
Problem Statement
It is very important to understand the issue and design of individual rehabilitation strategies for gait disorders in children with cerebral palsy. Therefore, the assessment is the first step in identifying and creating a complete picture of the individual’s deficiency. The assessment should include data on medical history, physical examination, functional assessment, observational and computerised tracking with gait path identification.
There have been numerous controversies about the acceptance of old and new concepts and methods of treatment. Many therapists do not have full access to scientific papers, and therefore they are sometimes unaware of the actualities in the field.
Research Questions
What are the actualities in the assessment and treatment of gait disorders in children with hemiplegia?
Purpose of the Study
The goal is to upgrade the information on how to assess and treat gait disorders in hemiplegic children. Physical therapy, through its specific means, aims (among many others) at gaining the autonomy of movement as quickly as possible, but this depends on the continuity of the rehabilitation program, motivation, communication and the power of example.
Research Methods
The research strategy focused on the key points able to meet the previously set requirements. There were used keywords such as: hemiparesis or hemiplegia, physiotherapy or physical therapy, hemiplegic gait, gait disorders, cerebral palsy. In addition, words as treatment or rehabilitation were introduced. The main sources were: databases, specialty books and magazines, reports, conference papers, official and legal publications, reviews, sites.
Inclusion criteria:
Papers addressing the recovery/rehabilitation of gait in cerebral palsy;
Full-text papers;
There were accepted papers older than 10 years;
Papers targeting the lower limb.
Exclusion criteria:
Papers studying the effects of surgical treatment;
Case studies;
Papers that did not have full text;
Studies on therapies that are not found in Romania;
Papers targeting the upper limb.
There were extracted the most common data encountered in the foreign literature on the evaluation of gait disorders in hemiplegic patients and data on the therapies and concepts also used in Romania for treating these deficiencies.
Findings
Each patient diagnosed with cerebral palsy has his/her own way of executing the movements, hence the need for personalized rehabilitation programs. The non-processing of gait disorders results in the reduction of physical activity, the loss of independence and has a negative impact on personality and psyche. There is no standard program for the rehabilitation of hemiplegic gait, so it is necessary to make effective treatment decisions based on accurate and complete data.
The evaluation of the child with cerebral palsy creates a lot of controversy among specialists. First, there is a disagreement about the optimal age at which the neurologic child can be diagnosed. Burns, O’Callaghan and Tudehope (1989) believe that the 8-month age is the most relevant, but of course with the close supervision of the patient. It is also considered that the Movement Assessment of Infants (MAI) provides more truthful information than others, helping to diagnose (Harris, 1991; Rose-Jacobs et al., 2004). The scale includes items that can make the difference between normal and neurological child starting at 4-month old and assessing: muscle tone, primitive reactions, automatic reactions and volitional movements.
Within the “Dr. N. Robănescu” CNCRNC, there is a functional scale for patient evaluation proposed by Dr. Robănescu himself, which closely follows the child’s milestone stages.
The assessment scale is a common means of communication between professionals, regardless of their origin country. We chose to list the most used ones in the scientific papers.
Gross Motor Function Classification Scale (GMFCS) (Palisano et al., 1997) – used in the evaluation of neurological child, it helps clarify the differences that define the severity of the dysfunction and presents the development of diagnosis in relation to the applied therapies (Algra & Carlberg, 2008). It estimates the patient’s future locomotor potential and is used in all international research.
More detailed is the Gross Motor Function Measure (GMFM) in two versions, with 66 or 88 items. The scale is a clinical tool designed to evaluate changes in the motor function of the child with cerebral palsy; it passes through all neuromotor developmental stages and targets children between 5 months and 16 years of age (Russell et al., 2002).
Functional Mobility Scale (FMS) (Graham et al., 2004) describes the functional mobility of children with cerebral palsy aged 4-18 years in three different types of environments: home – 5 m, at school – 50 m, in shopping centres – 500 m. A unique feature of FMS is the ability to distinguish the levels between the assistance devices used by the child and the environment.
Functional Assessment Questionnaire (FAQ) or Gillette Scale (Novacheck, Stout, & Tervo, 2000) is a functional report regarding the degree of ambulation of the patient in the environment. It is a scale on 10 levels.
Physician Rating Scale (PRS) and Observational Gait Scale (OGS – the modified version of PRS) follow different stages of development and progress of the gait. PRS detects changes in gait after applying the botulinum toxin treatment (Hausdorff & Alexander, 2005).
Modified Ashworth Scale (MAS) or the scale that measures spasticity, with scores between 0-4, is designed to quantify the muscle tissue strength at passive stretch.
Tardieu is a spasticity test scale evaluating the muscle response to passive stretch applied at three specific velocities (as low as possible, of the limb segment falling and the fastest possible). Researchers conclude that this scale is the most reliable (Yam & Leung, 2006; Hodgkinson, Vadot, & Berard, 2003).
The Selective Motor Control Scale (SMCS) measures selective dorsiflexion and ankle dexterity, the authors (Boyd & Graham, 1999) arguing that good control of the anterior tibial muscle is reflected in the quality of gait.
Muscle contraction is altered in spastic hemiplegics due to the disruption of neurological mechanisms, but also the changes in muscle tissue. Isokinetic dynamometer provides information about muscle contraction and is used to measure the muscle power generated in a controlled movement; however, it is rather difficult to use it for small children (Bohannon, 1989; Pierce et al., 2006).
MAS, Tardieu Scale and isokinetic dynamometer, together with surface EMG probes, are methods used in the evaluation of severe hypertonia (Gage et al., 2009).
Impact of the range of motion leads to the occurrence of possible contractions or bone deformation, disturbing the factors of gait, hence the need for muscle evaluation. It is also necessary to distinguish between mono- or bi-articular muscles. There are different tests (Palmer & Epler, 1998; Gage et al., 2009; Hausdorff & Alexander, 2005; Palastanga & Soames, 2012; Buckup, 2004): the Silverskiöld test (determines the difference in tone between gastrocnemius and soleus muscles), the Ely test (determines whether there is a shortening of the rectus femoris), the Thomas test (determines the rigidity of hip flexors), the adductor muscle tests (to avoid confusion with the gracilis, semitendinosus and semimembranosus, it combines the flexion-extension of the thigh and knee in 3 ways), the Ober test (determines whether there is rigidity in the tensor fasciae latae muscle or the iliotibial band), the uni- and bilateral angle or popliteal angle (determines the degree of stiffness of the hamstrings), the Craig’s test or the Netter angle (measures the femoral anteversion), the Patella Alta (follows the abnormal position of the patella relative to the femur), tibial torsion (measured in three ways, the most common being the angle formed between the bimalleolar axis and the femoral epicondyle axis).
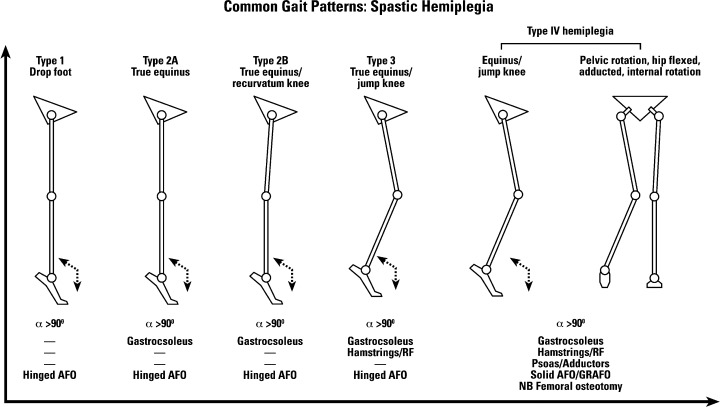
Rodda and Graham (2001) proposed a classification of spastic hemiplegia, which was later quoted in all books and complemented by researchers in the field. The classification refers only to the sagittal plane and fulfils the main objective in recovering these deficiencies, namely to determine the pattern of gait. The authors of the classification divided this pattern into 4 groups (pp. 98-108). (Figure
Group I:
The leg is in the equine in the oscillation phase, but in passive mobilisations, dorsiflexion is normal (Tecklin, 2015). The cause is the loss of selective motor control (Scrutton, Damiano, & Mayston, 2004).
The increased knee flexion in the last part of the oscillatory phase, the initial contact and leg loading.
Hyperflexion of the thigh in the oscillatory phase increases lumbar lordosis.
Group II (the most common one):
Plantar flexion throughout the entire gait cycle. The contraction of triceps surae prevents the tibia from moving anteriorly during the support phase. (Tecklin, 2015)
Genu recurvatum in the supporting phase.
The forward movement of the trunk is limited, so instead of keeping the centre of gravity above the legs, the child must hyper-flex the thigh with the increase of lumbar lordosis.
Group III:
A significant decrease in the knee joint movement, particularly during the swing phase, due to the co-contraction of the quadriceps or hamstrings.
Group IV:
Restricted thigh movement due to the iliopsoas and adductor hyperactivity defined by flexion-adduction and internal rotation of the thigh. For this reason, it does not extend completely at the end of the swing phase.
Usually, it develops the femur anteversion.
The equine of the foot and co-contraction of the knee.
Computerised gait analysis is the advanced form of gait measurement and analysis, using optoelectronic technology and giving detailed information about each patient’s gait patterns, but it cannot provide information about bone deformities; the final report should be correlated with medical history, clinical examination (Gage et al., 2009) or other investigations (radiographs, etc.). Such a laboratory uses rooms connected to software capable of detecting reflective markers, placed according to work protocols, on various anatomical markers rendering the three-dimensional image and numerous data on kinetics, kinematics, forces and EMG.
GAITRite® Systems is an electronic system used to measure the temporal and spatial parameters of gait, being a valid and reliable tool (McDonough et al., 2001).
In conclusion, each test and analysis provides critical and unique information that outlines the patient’s deficiency and from which individual treatment strategies can be formulated.
A recent study, which is a systematic review of physical therapy interventions in children of school age diagnosed with PC, concludes that, regardless of the number and quality of studies in recent years, there is still a need to improve methodological quality (Martin, Baker, & Harvey, 2012).
Physical therapy or manual therapy is the main discipline of the multidisciplinary team in the management of these disorders, according to studies analysing the management of children with PC (Craig, 1999; Anttila et al., 2008). Efficiency is higher if the patient is brought to the recovery lab as early as possible.
In the past, muscle strength training was considered as a determining factor to increase muscle spasticity, but it has been shown that training a spastic muscle with progressive resistance applied to a group of isolated muscles will increase muscle performance (Morton, Brownlee, & McFadyen, 2005; Eek et al., 2008). Closed kinematic chain exercises simulate normal gait movement, and the increase in muscle strength can improve the speed of gait and sensory power (Mockford & Caulton, 2008).
The literature is poor in demonstrating that passive mobilisation used to relax spastic muscles increases the range of motion and decreases spasticity (Pin, Dyke, & Chan, 2006), but it can only prevent subsequent bone deformities. Tardieu et al. (1988) stated that stretching the soleus muscle for 6 hours each day could prevent bone deformation.
The administration of proprioceptive neuromuscular facilitation exercises without the aid of the therapist or the stretching technique of Bob Anderson helps decontracting with awareness of the patient’s situation. The patient maintains at the end of the movement for 20-30 seconds. In most cases, they have a solid motivation. The technique can only be used if there is self-control. (Anderson, 2010)
The Bobath concept is the basis of treatment for the inhibition of exaggerated movements and the facilitation of normal volitional movements. It is believed that the emergence of compensatory strategies may block the rehabilitation potential (Cristea & Levin, 2000).
The principle of spiral dynamics or the three-dimensional dynamic twist of the body is characterised by the contraction and relaxation of the diagonal muscle chains. The concept defines three-dimensionally and systematically how motricity works. The same principle is adopted in the Kabat method (Zoltan, 2004).
Stimulating the proprioceptive and exteroceptive sensitivity with the role of modulating the motor response is performed by the following manoeuvres: stretching, brushing, Margaret Rood’s joint pressure stabilisation, steady plate gait. Muscle training aims to stimulate the type of specific agonist-antagonist inhibition-activation type of Margaret Rood’s concept. According to the author, rehabilitation is done following the sequence of ontogenetic sensory-motor development. (Drăgan & Pădure, 2014)
Even though the Frankel method is a form of treatment for patients with extrapyramidal system affection, one can use elements to practice proprioception through techniques and exercises with the visual supervision of the patient. Patients must maintain a certain line or direction without deviations (Robănescu, 2001).
A new concept that consists in applying of a series of therapeutic exercises aimed at re-educating postural control and engaging with anticipatory and compensatory postural adjustments is the Dolce method. The argument is that re-education and the quality of gait depends on the stability of the trunk (Mircea, 2010).
The concept of motor patterns was invented by Doman and Delacato in 1960 (DDPT) and is considered to be the hardest therapy in the world. The proposed theories are in fact an extension of the older concept related to the stages of ontogenetic development. In fact, the originality of the concept is the way of stimulating the appropriate development of these stages. The authors believe that passive mobilisations can influence the development and structure of the brain. Another principle is to cause the child to exceed his/her limits daily. Repeated exercises are used to promote the transport of oxygen to the brain (Hines, 2001).
Feldenkrais therapy is a form of somatic education through the use of certain movements, along with their awareness. This therapy promotes the idea of motor experience based on self-correction of mistakes, the idea of the one who works the best. The patient is free to perform the movements at his/her own pace. Feldenkrais states that “the only perfection of humanity is imperfection” (James et al., 1998; Connors et al., 2010).
Craniosacral therapy is a therapy that improves the physiological system through the special technique of releasing the somatic-emotional components. Research is poor in demonstrating the effectiveness of this therapy (Wyatt et al., 2011).
Therasuit therapy uses specific exercises and a device consisting of a porous, soft and dynamic orthosis, in order to improve the range of motion, posture, balance, flexibility, coordination, body alignment and function. The basic principle is dynamic proprioceptive correction, the costume being initially designed for cosmonauts. The literature is still poor in demonstrating the efficacy of this therapy (Bailes et al., 2011).
Essentis therapy for the treatment of locomotor disorders in cerebral palsy is applied after patient testing, resulting in a multi-therapy treatment strategy. There is no evidence of its effectiveness. It is a new therapy that is wanted to be promoted and implemented.
The therapies used are:
Test and osteopathic treatment (musculoskeletal, craniosacral, visceral)
Physiotherapy for motor and/or neurological problems
Test and acupuncture treatment
Theratog
Therasuit
Spider Therapy (active verticalisation)
Re-education of the archaic vestibular reflexes
Robotic therapy has become more and more present in the recovery centres in the world. Besides the main purpose of gait training, it provides a precise and objective assessment to the detriment of the classical one. This type of therapy outlines the future of a new generation (Magioni et al., 2016). But there is little evidence to show the superiority of this therapy. The only advantage is the low effort of the therapist, minimal costs, the time gained and the precise measurement of some parameters.
Assisted therapy (Lokomat) is particularly beneficial to patients who have balance disorders, who are more unable to maintain it compared to those who have already acquired this function (Kim et al., 2016).
Some researchers have found convincing evidence to suggest the use of certain interventions that increase the functional and structural efficacy of the body of children with cerebral palsy (Novak et al., 2013). They systematically describe the best interventions for children diagnosed with cerebral palsy based on a study that critically assesses:
All publications studying interventions on the child with PC, only in the medical field.
All levels of evidence 1-4 (levels 2-4 were studied if there was no level 1 study in that category).
The purpose of this systematic review is to create a link between research and practice by comparing more interventions, being helpful to take decisions. The researchers urge long-term learning, as this is the only way to optimise and calculate the results for these children.
Conclusion of the study:
Therapies considered most effective: botulinum toxin infiltration, orthosis, task-focused therapy, occupational therapy, fitness.
Therapies with an average level of effectiveness: acupuncture, animal-assisted therapy, assisted robotic therapy, hydrotherapy, strength-training therapies, therasuit, treadmill training, Vojta, manual stretching.
Therapies considered ineffective: craniosacral therapy, neuro-developmental therapy.
AFO (ankle-foot orthosis) maintains the correct position of the lower limb, especially the foot that may be in the equine, by reducing spasticity, and encourages its proper functioning (Blackmore et al., 2007; Teplicky, Law, & Russell, 2002). It increases independence by providing support (Petrușcă, 2012), lowering oxygen consumption, improving coordination and the ability to make weight transfer. Studies have shown that dynamic orthosis is more effective in postural control than the restrictive one (Algra & Carlberg, 2008).
The summary of included studies is shown in Table
After applying the inclusion and exclusion criteria, we found 30 papers about assessment and 22 about treatment. There were 11 randomized controlled trials, 8 reviews, 8 case series, 21 books, 1 case study and 1 validation study.
Conclusion
An important number of studies and papers describing methods of assessment have provided us with consistent support in creating an overall picture of what is effective and what is not, and what is expected to be investigated.
Each test and analysis provides critical and unique information that outlines the patient’s deficiency and from which individual treatment strategies can be formulated. Computerised biomechanical analysis or integrated motion analysis systems is currently the most advanced form of gait assessment.
The literature is poor in demonstrating the efficacy of many therapies and concepts..
References
- Algra, M. H., & Carlberg, E. B. (2008). Postural Control: A key issue in developmental disorders (pp. 270-295). Mac Keith Press.
- Anderson, B. (2010). Stretching (pp. 69-78). Shelter Publications.
- Anttila, H., Autti-Ramo, I., Suoranta, J., Makela, M., & Malmivaara, A. (2008). Effectiveness of physical therapy interventions for children with cerebral palsy: A systematic review. BMC Pediatrics, 8(14), 1471-2431. doi: 10.1186/1471-2431-8-14
- Bailes, A. F., Greve, K., Burch, C. K., Reder, R., Lin, L., & Huth, M. M. (2011). The effect of suit wear during an intensive therapy programme in children with cerebral palsy. Pediatric Physical Therapy, 23(2), 136-142. doi: 10.1097/PEP.0b013e318218ef58
- Blackmore, A. M., Boettcher-Hunt, E., Jordan, M., & Chan, M. D. (2007). A systematic review of the effects of casting on equinus in children with cerebral palsy: An evidence report of the AACPDM. Developmental Medicine & Child Neurology, 49(10), 781-790. doi: 10.1111/j.1469-8749.2007.00781.x
- Buckup, K. (2004). Clinical tests for the musculoskeletal system. Examination – Signs – Phenomena (pp. 143-225). Thieme.
- Burns, Y. R., O ҆Callaghan, M., & Tudehope, D. I. (1989). Early identification of cerebral palsy in high risk infants. Australian Pediatric Journal, 25(4), 215-219.
- Bohannon, R. W. (1989). Is the measurement of muscle strength appropriate in patients with brain lesions? A special communication. Physical Therapy, 69(3), 225-236.
- Bondar, E., Bulz, A., Popescu, E. C., & Tulvan Szteklacs, I. V. (2017). Exercițiul fizic – miracol necesar în viața omului de zi cu zi (Studii și cercetări) (pp. 146-184). București: StudIS.
- Boyd, R., & Graham, H. (1999). Objective measures of clinical findings in the use of botulinum toxin A for the management of children with cerebral palsy. European Journal of Neurology, 6(4), 523-535. Doi: 10.1111/j.1468-1331.1999.tb00031.x
- Centers for Disease Control and Prevention. (2016). Data and statistics for cerebral palsy. Retrieved from https://www.cdc.gov/ncbddd/cp/data.html
- Cioni, G., & Mercuri, E. (2007). Neurological assessment in the first two years of life. Instruments for the follow-up of high-risk newborns (pp. 38-48). Mac Keith Press.
- Cioni, G., Sale, B., Paolicelli, P. B., Petacchi, E., Scusa, M. F., & Canapicchi, R. (1999). MRI and clinical characteristics of children with hemiplegic cerebral palsy. Neuropediatrics, 30(5), 249-255. doi: 10.1055/s-2007-973499
- Craig, M. (1999). Physiotherapy management of cerebral palsy: Current evidence and pilot analysis. Physical Therapy Reviews, 4(4), 215-228.
- Cristea, M. C., & Levin, M. F. (2000). Compensatory strategies for reaching in stroke. Brain, 123(5), 940-953.
- Connors, L. A., Galea, M. P., Said, C. M., & Remedios, L. J. (2010). Feldenkrais Method balance classes are based on principles of motor learning and postural control retraining: A qualitative research study. Physiotherapy, 96(4), 324-336. doi: 10.1016/j.physio.2010.01.004
- Drăgan, C. F., & Pădure, L. (2014). Metodologie și tehnici de kinetoterapie (pp. 52-55). București: Național.
- Eek, M. N., Tranberg, R., Zugner, R., Alkema, K., & Beckung, E. (2008). Muscle strength training to improve gait function in children with cerebral palsy. Developmental Medicine & Child Neurology, 50(10), 759-764. doi: 10.1111/j.1469-8749.2008.03045.x
- Gage, J., Schwartz, M. H., Koop, S. E., & Novacheck, T. F. (2009). The identification and treatment of gait problems in cerebral palsy (pp. 31-64, 181-204). Mac Keith Press.
- Graham, H. K., Harvey, A., Rodda, J., Nattrass, G. R., & Pirpiris, M. (2004). The Functional Mobility Scale (FMS). Journal Pediatrics Orthopedics, 24(5), 514-520.
- Harris, S. R. (1991). Movement analysis – an aid to diagnosis of cerebral palsy. Physical Therapy, 71(3), 215-221. https://doi.org/10.1093/ptj/71.3.215
- Hausdorff, J. M., & Alexander, N. B. (2005). Gait disorders. Evaluation and management (pp. 247-267). Taylor & Francis Group.
- Hines, T. M. (2001). The Doman-Delacato patterning treatment for brain damage. The Scientific Review of Alternative Medicine, 5(2), 80-89.
- Hodgkinson, I., Vadot, J. P., & Berard, C. (2003). Évaluation clinique de l’enfant spastique. Neurochirurgie, 49(2-3), 199-204. doi: NCHIR-05-2003-49-2-3C2-0028-3770-101019-ART08
- James, M., Kolt, G., McConville, J., & Bate, P. (1998). The effects of Feldenkrais program and relaxation procedures on hamstring length. Australian Physiotherapy, 44(1), 49-54.
- Kim, S. J., Lee, H. J., Hwang, S. W., Pyo, H., Yang, S. P., Lim, M. H., … Kim, E. J. (2016). Clinical characteristics of proper robot-assisted gait training group in non-ambulatory subacute stroke patients. Annals of Rehabilitation Medicine, 40(2), 183-189. doi: 10.5535/arm.2016.40.2.183
- Magioni, S., Melendez-Calderon, A., van Asseldonk, E., Klamroth-Marganska, V., Lünenburger, L., Riener, R., & van der Kooij, H. (2016). Robot-aided assessment of lower extremity functions: A review. Journal of NeuroEngineering and Rehabilitation, 13(72). Doi: 10.1186/s12984-016-0180-3
- Martin, L., Baker, R., & Harvey, A. (2010). A systematic review of common physiotherapy interventions in school-aged children with cerebral palsy. Physical Occupational Therapy Pediatrics, 30(4), 294-312. doi: 10.3109/01942638.2010.500581
- McDonough, A. L., Batavia, M., Chen, F. C., Kwon, S., & Ziai, J. (2001). The validity and reliability of the GAITRite system’s measurements: A preliminary evaluation. Arch Phys Med Rehabil., 82(3), 419-425. doi: 10.1053/apmr.2001.19778
- Mircea, I. (2010). Corelații privind controlul trunchiului și eficacitatea unei noi metode kinetice pentru recuperarea ortostatismului și mersului în hemiplegie. Jurnalul Medical Brașovean, 2, 29-32.
- Mockford, M., & Caulton, J. (2008). Systematic review of progressive strength training in children and adolescents with cerebral palsy who are ambulatory. Pediatric Physical Therapy, 20(4), 318-333.
- Morton, J. F., Brownlee, M., & McFadyen, A. K. (2005). The effects of progressive resistance training for children with cerebral palsy. Clinical Rehabilitation, 19(3), 283-289. doi: 10.1191/0269215505cr804oa
- Mureșan, D. (2008). Kinetoterapia în afecțiunile pediatrice (pp. 36-50). București: Ed. Fundației România de Mâine.
- Novacheck, T. F., Stout, J. L., & Tervo, R. (2000). Reliability and validity of Gillette Functional Assessment Questionnaire as an outcome measure in children with walking disabilities. Journal Pediatrics Orthopedics, 20(1), 75-81. DOI: 10.1097/01241398-200001000-00017
- Novak, I., Mcintyre, S., Morgan, C., Campbell, L., Dark, L., Morton, N., … Goldsmith, S. (2013). A systematic review of interventions for children with cerebral palsy: State of the evidence. Developmental Medicine & Child Neurology, 55(10), 885-910. doi: 10.1111/dmcn.12246
- Onose, G., & Pădure, L. (2008). Compediu de neurorebilitare la adulți, copii și vârstnici (pp. 23-60). București: Editura Universitară “Carol Davila”.
- Palastanga, N., & Soames, R. (2012) Anatomy and human movement. Structure and function (pp. 223-384). Elsevier.
- Palisano, R., Rosenbaum, P., Walter, S., Russell, D., Wood, E., & Galuppi, B. (1997). Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine & Child Neurology, 39(4), 214-223. doi: 10.1111/j.1469-8749.1997.tb07414.x
- Palmer, L. M., & Epler, M. E. (1998). Fundamentals of musculoskeletal assessment techniques (pp. 281-364). Lippincott Williams & Wilkins.
- Petrușcă, I. (2012). Dispozitive ajutătoare de mers. Balneo-Research Journal, 3(1), 18-21.
- Pierce, S. R., Lauer, R. T., Shewokis, P. A., Rubertone, J. A., & Orlin, M. N. (2006). Test-retest reliability of isokinetic dynamometry for the assessment of spasticity of the knee flexors and knee extensors in children with cerebral palsy. Archives of Physical Medicine and Rehabilitation, 87(5), 697-702. doi: http://dx.doi.org/10.1016/j.apmr.2006.01.020
- Pin, T., Dyke, P., & Chan, M. (2006). The effectiveness of passive stretching in children with cerebral palsy. Developmental Medicine & Child Neurology, 48(10). 855-862. doi: 10.1017/S0012162206001836
- Rethlefsen, S., Ryan, D., & Kay, R. (2010). Classification systems in cerebral palsy. Orthop Clin North Am., 41(4), 457-467. doi: 10.1016/j.ocl.2010.06.005
- Robănescu, N. (2001). Reeducarea neuro-motorie. Recuperare funcțională și readaptare (pp. 261-265). București: Ed. Medicală.
- Robănescu, N. (1983). Tratamentul sechelelor motorii ale encefalopatiilor infantile (Paralizia spastică cerebrală) (pp. 33-43). București: Ed. Medicală.
- Rodda, J., & Graham, H. K. (2001). Classification of gait patterns in spastic hemiplegia and spastic diplegia: A basis for a management algorithm. European Journal of Neurology, 8(5), 98-108.
- Rosenbaum, P., Paneth, N., Leviton, A., Goldstein, M., Bax, M., Damiano, D., … Jacobson, B. (2007). A report: The definition and classification of cerebral palsy. Developmental Medicine & Child Neurology, 109, 8-14.
- Rose-Jacobs, R., Cabral, H., Beeghly, M., Brown, E. R., & Frank, D. A. (2004). The Movement Assessment of Infants (MAI) as a predictor of two year neurodevelopmental outcome for infants born at term who are at social risk. Pediatrics Physical Therapy, 16(4), 212-221. DOI: 10.1097/01.PEP.0000145931.87152.CO
- Russell, D., Rosenbaum, P. L., Avery, L. M., & Lane, M. (2002). Gross Motor Function Measure (GMFM66 & GMFM 88). User ҆s Manual (pp. 1-9). Cambridge: Mac Keith.
- Scrutton, D., Damiano, D., & Mayston, M. (2004). Management of motor disorders of children with cerebral palsy (pp. 9-31, 105-127). Cambridge: Cambridge University Press.
- Tardieu, C., Lespargot, A., Tabary, C., & Brett, M. D. (1988). For how long must the soleus muscle be stretched each day to prevent contractures? Developmental Medicine & Child Neurology, 30(1), 3-10. doi: 10.1111/j.1469-8749.1988.tb04720.x
- Tecklin, J. S. (2015). Pediatric physical therapy (pp. 187-243). Lippincott Williams & Wilkins.
- Teplicky, R., Law, M., & Russell, D. (2002). The effectiveness of casts, orthoses and splints for children with neurological disorders. Infants Young Child, 15(1), 42-50.
- Zoltan, P. (2004). Kinetoterapie în neuropediatrie (pp. 248-258). Arionda.
- Wiklund, L., & Uvebrant, P. (1991). Hemiplegic cerebral palsy: Correlation between CT morphology and clinical findings. Developmental Medicine & Child Neurology, 33(6), 512-523.
- Wyatt, K., Edwards, V., Franck, L., Britten, N., Creanor, S., Maddick, A., & Logan, S. (2011). Cranial osteopathy for children with cerebral palsy: A randomised controlled trial. Archives of Disease in Childhood, 96(6), 505-512. doi: 10.1136/adc.2010.199877
- Yam, W. K., & Leung, M. S. (2006). Interrater reliability of Modified Ashworth Scale and Modified Tardieu Scale in children with spastic cerebral palsy. Journal Children Neurology, 21(12), 1031-1035. doi: 10.1177/7010.2006.00222
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
05 March 2018
Article Doi
eBook ISBN
978-1-80296-035-8
Publisher
Future Academy
Volume
36
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-484
Subjects
Sports, sport science, physical education, health psychology
Cite this article as:
Popescu, C. E., Bondar, E., Tulvan, I. V., & Bulz, A. (2018). Actualities in Treatment of Gait Disorders in Children with Hemiplegia. In V. Grigore, M. Stanescu, & M. Paunescu (Eds.), Physical Education, Sport and Kinetotherapy - ICPESK 2017, vol 36. European Proceedings of Social and Behavioural Sciences (pp. 283-297). Future Academy. https://doi.org/10.15405/epsbs.2018.03.38

