Preventive Measures Of Venous Thromboembolism In The Hospitalized Patient: An Integrative Literature Review
Abstract
Venous thromboembolism (VTE) includes two closely associated clinical conditions: deep vein thrombosis (DTV) and its main acute complication, pulmonary embolism (PE). In the hospital setting, venous thromboembolism is a concern because of its high prevalence rate. It is estimated that one in twenty inpatients is at risk of pulmonary embolism, if adequate preventive measures are not applied. These may or may not be pharmacological. In this context, the objective of this study is to identify the non-pharmacological measures recommended to prevent venous thromboembolism in inpatients. An integrative literature review was performed using the PI[C]OD method by searching the following databases: EBSCO host, PubMed, JBI, PEDro, Elsevier-ClinicalKey, Scielo and Google Academic studies published in the períod 2006-2016. From the research were included five articles that met the inclusion criteria. The results of the review found that effective mechanical methods comprised graduated compression stockings and intermittent pneumatic compression devices while for nursing care early mobilization and ambulation were identified as preventive measures of VTE. The studies suggest several benefits of using non-pharmacological measures to prevent venous thromboembolism. The differentiated intervention of the nurse specialist in rehabilitation integrated in the multidisciplinary team can be an added value in the adequacy of these measures.
Keywords: Venous thromboembolismDeep vein thrombosisPulmonary embolismPreventive measuresNursing careRehabilitation
Introduction
Venous thromboembolism (VTE) continues to be considered the third most common cardiovascular disease pathology (Gouveia, Pinheiro, Costa, & Borges, 2016) following acute myocardial infarction and stroke (Goldhaber, 2012). The term VTE is used to define two clinical manifestations that are closely associated: deep venous thrombosis (DVT) and its main acute complication, pulmonary thromboembolism (PTE) (Gharaibeh, Albsoul-Younes, & Younes, 2015). DVT is characterized by thrombus formation in the deep veins of the lower limbs, which may result in partial or total obstruction of blood flow (Miranda, Matielo, Porto, Marques, & Yoshida, 2015). When a thrombus moves from its site of formation and travels, or embolizes, to the arterial blood supply of one of the lungs can cause pulmonary artery blockage giving rise to PE (Barker, & Marval, 2011).
VTE is considered a serious public health problem due to its high morbidity and mortality rate (Heit, Spencer, & White, 2016). In 2007 this pathology was found to be responsible for about 12% of deaths in Europe (Amaral, & Tavares, 2013) and direct healthcare costs related to VTE in the European Union per year range from 1.5 to 13.2 (Behravesh, Hoang, Nanda, Wallace, Sheth, Deipolyi, & Oklu, 2017).
VTE is also a concern for its high prevalence rate in the hospital environment, estimating that one in every 20 hospitalized patients is at risk of developing PTE if they do not receive adequate thromboprophylaxis (França, Sousa, Felicíssimo, & Ferreira, 2011). In the long term complications of VTE such as post-thrombotic syndrome and chronic pulmonary hypertension may arise (Behravesh, Hoang, Nanda, Wallace, Sheth, Deipolyi, & Oklu, 2017) which may increase hospital admission days and future hospital admissions. Given the importance of this issue, VTE prophylaxis is one of the most cost-effective measures of clinical practice and is a priority strategy to improve the safety of hospitalized patients (Amaral & Tavares, 2013). It has been the subject of warnings from a number of agencies assessing global health quality such as the National Institute for Clinical Excellence, the Scottish Intercollegiate Guidelines Network, the American College of Chest Physicians, the European Society of Cardiology (Konstantinides, Torbicki, Agnelli, Danchin, Fitzmaurice, Galiè, N. Lang, I, & Collaborators, 2014), among others. The guidelines developed by these organizations recommend that all hospitalized patients be evaluated for VTE risk and that hospitals develop protocols for adequacy of prophylaxis . In this context, according to an adequate risk stratification, several preventive methods of VTE can be used in the hospitalized patient: pharmacological or non-pharmacological. Although pharmacological prophylaxis is already consecrated by clinical experience, non-pharmacological measures also play a prominent role in preventing VTE. Its use is suggested as an alternative for patients at high risk of bleeding where anticoagulant therapy is contraindicated or in conjunction with drug prophylaxis (Bang, Jang, Kim, Yim, Kim, Nam, & Kim, 2014).
Problem Statement
Based on framework described above, an integrative review of the literature was carried out, based on evidence-based practice as an approach that leads to the development and / or use of research results in clinical practice. This is one of the research methods used in the foundation of an evidence-based practice that enables the integration of research results into clinical context, whose purpose is to gather and synthesize research results on a topic that is done in a systematic way (Mendes, Silveira, & Galvão, 2008). In this paper, we present the results of the study. Thus, the development of nursing, as a discipline and profession, has been a strong contribution to the expressive increase of knowledge production, a factor considered as a fundamental tool in suppressing the needs verified in clinical practice (International Council of Nurses, 2012). Yet, according to the same body, the conscious, explicit and judicious use of the best existing evidence helps to make health care decisions to patients. Evidence-based practice involves integrating individual clinical competence with what is best available in the scientific evidence resulting from the research and that aligns the patient's perspective in clinical decision-making.
Research Questions
Considering the contextualization of the subject under study, and considering the importance of the practice based on evidence for the professional practice in the area of rehabilitation nursing, the following research question arose:
- "What are the non-pharmacological measures recommended for the prevention of venous thromboembolism in hospitalized patients?”
Purpose of the Study
Taking into account the research question, this study aims to identify the non-pharmacological measures recommended for the prevention of venous thromboembolism in the hospitalized patient.
Research Methods
An integrative literature review was performed using the PI[C]OD method. As a strategy for the location and selection of studies, three steps were accomplished. Initially a simple search was conducted limited to MEDLINE and CINAHL, followed by an analysis of the words in the titles and abstracts, and the terms used to describe the studies. A search was then conducted on the National Center for Biotechnology Information website at http://www.ncbi.nlm.nih.gov/mesh to confirm if the preliminary terms were MeSH terms (Medical Subject Headings). Obtained positive response to:
- #1 MeSH descriptor “Venous Thromboembolism” (explore all trees);
- #2 MeSH descriptor “Deep Vein Thrombosis” (explore all trees);
- #3 MeSH descriptor “Pulmonary Embolism” (explore all trees);
- #4 MeSH descriptor “Nursing Care” (explore all trees);
- #5 MeSH descriptor “Rehabilitation” (explore all trees);
- #6 MeSH descriptor “Exercise Therapy” (explore all trees);
- #7 MeSH descriptor “Intermittent Pneumatic Compression devices” (explore all trees);
- #8 MeSH descriptor “Stockings, Compression” (explore all trees);
- #9 MeSH descriptor “Early Ambulation” (explore all trees);
- #10 MeSH descriptor “Inpatients” (explore all trees).
The following research was conducted between March and November 2016 and included electronic searches in the following databases: CINAHL Complete, MedicLatina, Medline Complete, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, and Nursing & Allied Health Collection: Comprehensive from the EBSCOhost platform supplemented by the PubMed, JBI Library of Systematic Reviews, PEDro, Elsevier-ClinicalKEY, SciELO-Scientific Electronic Library Online and Google Scholar through the Boolean conjugation of all Identified descriptors - # 11 [# 1 OR # 2 OR # 3 AND # 4 OR # 5 OR # 6 OR # 7 OR # 8 OR # 9 AND # 10] (title and subject).
For the databases that do not use the MeSH descriptors, the following Boolean formula was used:
- Venous Thromboembolism OR Deep Vein Thrombosis OR Pulmonary Embolism And Nursing Care OR Rehabilitation OR Exercise Therapy Intermittent Pneumatic Compression devices OR Compression Stockings OR Early Ambulation AND Inpatients.
In the PEDro (Physiotherapy Evidence Database) electronic database the search term was "Venous Thromboembolism" (title and abstract).
The last step consisted of analyzing the list of bibliographic references of all identified studies to extract additional studies if possible.
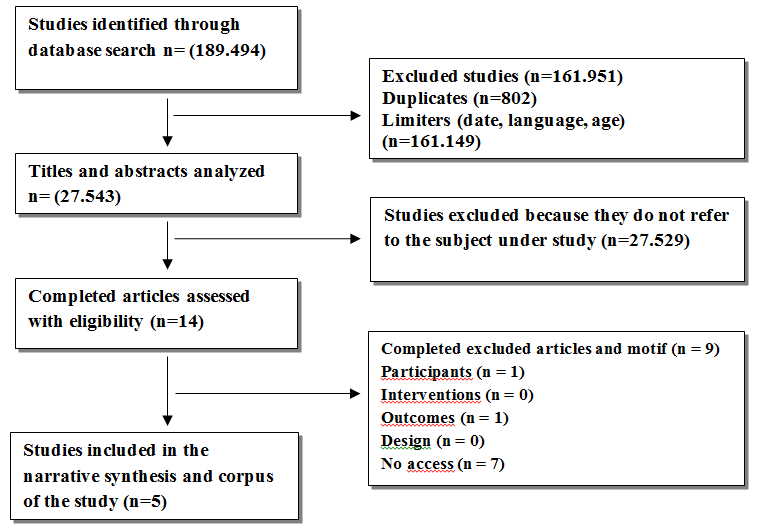
The first selected sample consisted of 189.494 studies. However, because of the size of the sample, research limiters were applied, and only those studies that had the following requirements were considered: published in Portuguese, English or Spanish; Full text, date of publication in the period from January 2006 to November 2016, participants classified as adults and studies in humans. After its application and after the extraction of duplicates (802), 161.951 were excluded. The detailed and specified search strategy process for each database can be found in Table
After reading the titles and summaries of the remaining 27.543 studies, it was reduced to 14 because they did not refer to the topic under study (referring only to pharmacological measures). It is important to point out that the entire strategy of research and selection of studies was carried out by two researchers independently. We then analyzed the full text articles (n = 14), based on the application of more rigorous criteria, which were established based on the PI[C]OD methodology (Ramalho, 2005) and are presented in Table
Data were then collected, involving two steps: extraction and synthesis of the data. To that end, the data were extracted from studies that had previously composed the corpus by two reviewers alone, using the instrument "The Joanna Briggs Institute data extraction form for systematic review of experimental / observational studies" JBI (2011). Data extracted included details of interventions, population, study methods, outcomes relevant to the issue under study, and specific objectives. These data were synthesized in a "framework of evidence" (Craig & Smyth, 2004). Tables with the critical evaluation of studies 4 and 5 were also drawn up (studies 1,2 and 3 are of a qualitative nature. The whole process of selection of the corpus of the study was synthesized in the following flowchart (Figure
Findings
Of the studies identified through the types of research mentioned and the use of the methodology mentioned above, through which a critical evaluation was located, selected and performed based on the selection criteria adopted, only 5 articles were selected for the study corpus.
Following are the main results of the analysis of the selected studies, which were grouped and organized in a table, in order to answer the research question previously stated. Table
In order to answer the research question "What are the non-pharmacological measures recommended for the prevention of venous thromboembolism in the hospitalized patient?" Studies were used, according to the methodology adopted, by four types: a case study With a qualitative approach (Pinho, Viegas & Caregnato, 2016), a literature review (Vitor, Daou & Góis, 2016; Gusmão, Silva & Azevedo, 2014), a systematic review of the literature (Penha, Damiano, Carvalho , Lain & Serafim, 2009) and a quantitative-randomized clinical trial (Labarere, Bosson, Sevestre, Sellier, Richaud, & Legagneux, 2007).
Table
Conclusion
The prevention of venous thromboembolism in hospitalized patients is particularly important because of the high prevalence of this pathology in this context. There is evidence that prevention is the safest, most effective and cost-effective strategy for reducing VTE morbidity and mortality. Through an adequate risk stratification it is possible to categorize the level of risk for each patient and to adapt prophylactic measures that may be pharmacological and non-pharmacological. The analysis of the 5 articles selected allowed us to answer the research question that guided this study. The mechanical methods were as follows: non-pharmacological measures recommended for the prevention of VTE in the hospitalized patient: mechanical compression stockings and intermittent pneumatic compression devices; Nursing care: early mobilization and ambulation.
Evidence of the results revealed that:
•mechanical methods: -increase the velocity of venous flow of the lower limbs, reducing venous stasis; -Have a fibrinolytic effect on the vascular endothelium; -are more effective in patients with low / medium risk in the impossibility of using anticoagulants; -do not benefit high-risk patients, but reduce DVT by 65% when compared to no prophylaxis;
•early mobilization may contribute to the reduction of thrombus progression;
•ambulation aids systemic circulation, improves self-esteem, autonomy, pressure ulcer prevention and minimizes the risk of DVT development;
•ambulation in combination with anti-coagulation and leg compression in patients with acute DVT leads to a more rapid regression of clinical signs and symptoms such as pain, edema, hyperemia and temperature rise;
•physical exercise accentuates fibrinolytic activity.
These measures corroborate and provide scientific evidence to the guidelines issued by various bodies assessing the quality of health worldwide. This allows us to defend the implementation of a rehabilitation program whose objectives are: improve the safety of the hospitalized patient; minimize the inabilities and limitations of survivors; contribute to the autonomy and quality of life; gain health gains.
Thus, a rehabilitation program is presented, which includes a set of preventive measures that should be applied to clinical practice after the evaluation of each patient's risk profile (Table
However, despite the evidence of the results of this RIL we are aware that it has some limitations. In this sense, other databases could have been used but limitations in access to them conditioned this restriction; Only free access articles were studied in Portuguese, English and Spanish and we found that there are few studies that refer only to non-pharmacological measures.
Aware of the limitations, we consider that the development of this study was very positive because of the pertinence of the theme and because it is necessary to have more investment by the rehabilitation nursing to show its role in the prevention of this pathology.
As future research, we suggest longitudinal studies that attest to the efficacy of nursing care: early mobilization, ambulation and therapeutic exercises for the prevention of VTE in the hospitalized patient.
This study has implications for the practice:
•Raise the awareness of health professionals at the institution level through training actions in order to provide reflection and understanding of the importance of optimizing VTE preventive measures;
•Disseminate the results of this research at the level of the scientific community through the elaboration of posters, oral communications, publication of an article;
•Develop an action protocol that contributes to the adequacy of preventive measures;
•Sensitize / educate patients and caregivers:
-Establish an intervention plan directed at combating and / or modifying risk factors,
-encourage the promotion of healthy lifestyles in which regular exercise is encouraged and a balanced and varied diet in order to prevent and reduce the risk of these events,
-to plan together with them an appropriate care program, enabling them to continue their care in the post-discharge period;
•Present the proposal for a Follow-up Rehabilitation Nursing Consultation.
Thus, the rehabilitation nurse as well as the rehabilitator assumes the role of educator of the patient and caregivers in a practice not only curative, also acting in the modification and / or combat of risk factors.
Ultimately, VTE prevention should be multidisciplinary, and each institution must develop a strategy that guarantees a successful preventive approach, thus contributing to the improvement and safety of health care provided.
Acknowledgments
We would like to show our gratitude to Librarians of the Library of the Superior School of Health of Viseu for their contribution in the research. Financing CI&DETS, Health School /Polytechic Institute of Viseu
References
- Amaral, C., & Tavares, J. (2013). Profilaxia do tromboembolismo venoso no doente cirúrgico. Revista da Sociedade Portuguesa de Anestesiologia, 22(1), 12-19.
- Bang, S. M., Jang, M. J., Kim, K. H., Yhim, H. Y., Kim, Y. K., Nam, S. H., & Kim, Y. K. (2014). Prevention of venous thromboembolism: korean society of thrombosis and hemostasis evidence-based clinical practice guidelines. Journal of Korean Medical Science, 29 (2), 164-171.
- Barker RC, Marval (2011) .Venous Thromboembolism: risks and prevention. Critic Care Pain. 11(1):18-23.
- Behravesh, S., Hoang, P., Nanda, A., Wallace, A., Sheth, R. A., Deipolyi, A. R., & Oklu, R. (2017). Pathogenesis of Thromboembolism and Endovascular Management. London: Press.
- França, A., Sousa, J., Felicíssimo, P., & Ferreira, D. (2011). Avaliação do risco de tromboembolismo venoso. Acta Médica Portuguesa, 24, 575-582.
- Gharaibeh, L., Albsoul-Younes, A., & Younes, N. (2015). Evaluation of venous thromboembolism prophylaxis after the introduction of an institutional guideline: Extent of application and implementation of its recommendations. Journal of Vascular Nursing, 33(2), 72-78.
- Goldhaber, S. Z. (2012). Venous thromboembolism: epidemiology and magnitude of the problem. Best Practice & Research Clinical Haematology, 25(3), 235-242.
- Gouveia, M., Pinheiro, L., Costa, J., & Borges, M. (2016). Embolia pulmonar em Portugal: Epidemiologia e mortalidade intra-hospitalar. Acta Médica Portuguesa, 29(7-8), 432-440.
- Gusmão, G.L., Silva, L.X., & Azevedo, A.S. (2014). Assistência de enfermagem no tratamento da trombose venosa profunda em pacientes críticos. Biologia & Saúde, 15 (4), 50-60
- Guyatt, G. H., Akl, E. A., Crowther, M., Gutterman, D. D., & Schuünemann, H. J. (2012). Executive summary: antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. CHEST Journal, 141 (2_suppl), 7S-47S
- Heit, J.A., Spencer,F.A.& White, R.H.(2016). The epidemiology of venous thromboembolism. Journal of Thrombosis and Thrombolysis, 41:3-14.
- Konstantinides, S., Torbicki, A., Agnelli, G., Danchin, N., Fitzmaurice, D., Galiè, N., Lang, I. & Collaborators (2014). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J, 35(43):3033-69
- Labarere, J., Bosson, J. L., Sevestre, M. A., Sellier, E., Richaud, C., & Legagneux, A. (2007). Intervention targeted at nurses to improve venous thrombo-prophylaxis. International Journal for Quality in Health Care, 19(5), 301-308.
- Mendes, K. D. S., Silveira, R. C. D. C. P., & Galvão, C. M. (2008). Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto & Contexto-Enfermagem, 17(4), 758-764.
- Penha, G.S., Damiano, A.P., Carvalho, T., Lain, V., & Serafim, J.D. (2009). Early mobilization in acute stage of deep venous thrombosis of the lower limbs. J. Vasc Bras, Vol. 8, 1, 77-85.
- Pinho, N.G., Viegas, K., & Caregnato, R.C.A. (2016). Papel do enfermeiro no período peri-operatório para prevenção da trombose venosa profunda. Rev. Sobecc, 21(1): 28-36.
- Vitor, S.K.S., Daou, J.P., & Góis, A.F.T. (2016). Prevenção de tromboembolismo venoso (trombose venosa profunda e embolia pulmonar) em pacientes clínicos e cirúrgicos. Diagnóstico & Tratamento, 21(2), 9-64.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
14 September 2017
Article Doi
eBook ISBN
978-1-80296-029-7
Publisher
Future Academy
Volume
30
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-376
Subjects
Health, public health, preventive healthcare, preventive care, preventive medicine
Cite this article as:
Albuquerque, C., Costa, C., Martins, R., & Madureira, A. (2017). Preventive Measures Of Venous Thromboembolism In The Hospitalized Patient: An Integrative Literature Review. In Z. Bekirogullari, M. Y. Minas, & R. X. Thambusamy (Eds.), Health and Health Psychology - icH&Hpsy 2017, vol 30. European Proceedings of Social and Behavioural Sciences (pp. 24-34). Future Academy. https://doi.org/10.15405/epsbs.2017.09.3

