Abstract
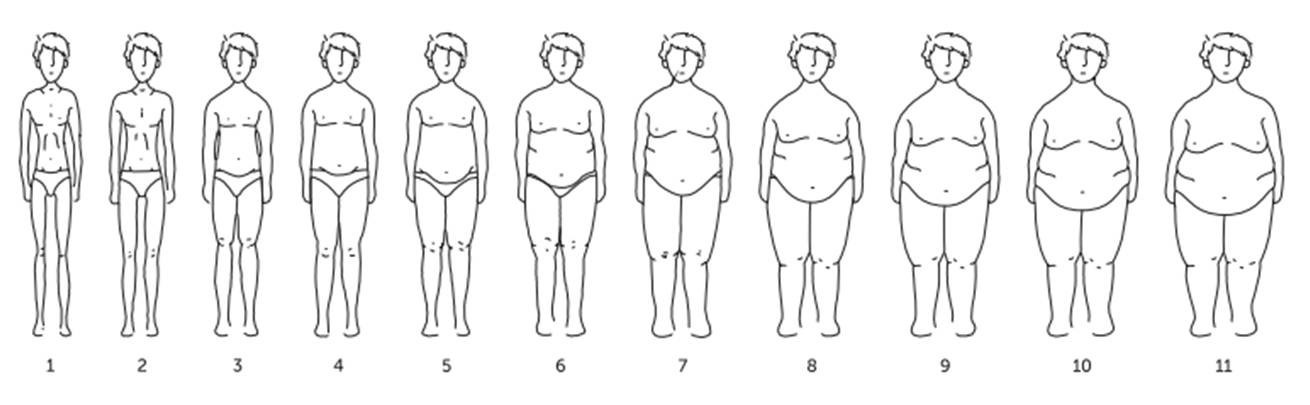
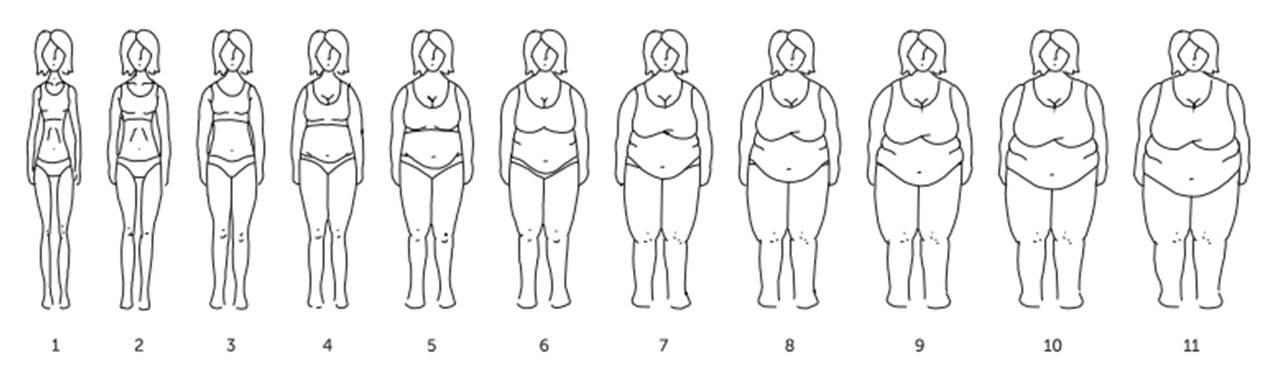
Obesity keeps spreading, leading to physical and psychological comorbidities, namely body image dissatisfaction (BID). Its treatment is difficult, especially of severe obesity, for which bariatric surgery has become the only effective treatment. It would be important to have an instrument to assess BID of bariatric patients. The present study main goals are to describe the construction of a new instrument (Obesity Surgery Silhouettes Scale – ESCO) to assess BID of bariatric patients, as well as to present data from a pre-test. ESCO consists of 11 male and 11 female silhouettes, distributed in ascending order across Body Mass Index (BMI) categories. It was administered to a clinical sample made by 20 obese patients, candidates to bariatric surgery and a community sample constituted of 10 subjects. ESCO reveals of very fast administration, with mean answer time of 55.9 seconds (clinical sample). A higher BID is verified on the clinical sample (BID=5.2), in comparison with the community sample (BID=1.5). There is a statistically significant positive correlation between BMI and BID, suggesting that body image dissatisfaction increases with higher BMI. Preliminary results suggest ESCO is a capable instrument to assess BID of bariatric patients. Data from ESCO will be useful to design psychological counseling, specific to each patient. Besides that, it will allow the use of BID indicators as a bariatric surgery results’ measure.
Keywords: Obesitybody imagebariatric surgerysilhouettes scaleself-perceptions
Introduction
Obesity is a multifactorial chronicle disease, which is growing all over the world (Alciati et al., 2007; WHO, 2000), and is considered as the 21st century epidemic by the World Health Organization (World Health Organization [WHO], 2000). Worldwide, the number of persons classified as having overweight or obesity evolved from 921 million in 1980, to 2.1 billion in 2013 (Ng et al., 2014).
In Portugal, data presented by Ng et al. (2014), revealed that 28.7% of boys (<20 years) and 63.8% of men (≥20 years) are overweight, as well as 27.1% of girls (<20 years) and 54.6% of women (≥20 years). In turn, obesity affects 8.9% of boys and 20.9% of men, as well as 10.6% of girls and 23.4% of women.
Given the lack of effectiveness of non-surgical treatment programs for severe obesity (Ray, Nickels, Sayeed & Sax, 2003), there has been a substantial increase in the number of severe obese patients looking for surgical treatment, (Davis, Slish, Chao & Cabana, 2006), and the numbers keep rising (Snyder, 2009).
Psychological assessment of patients candidates to bariatric surgery represents an invaluable piece of the more wide pre-surgical assessment, whether in short- or long-term (Snyder, 2009). In fact, it represents an essential component of the multiprofessional/multidisciplinary care in the obesity surgical treatment (Blackburn et al., 2009).
Medical and physical comorbidities are not the only ones associated with obesity. Obesity is also related to social and psychological problems, namely with lower quality of life (QoL) and compromised body image (Adami et al., 1998; Fabricatore, Wadden, Sarwer & Faith, 2005; Mathus-Vliegen, de Weerd & de Wit, 2004). There is evidence that psychological and/or psychiatric difficulties before bariatric surgery are common (Ferreira, Santos, Pegacho & Carvalho, 2010).
In the last decades body image has been receiving high attention by the scientific community. Nowadays it is considered as a multidimensional construct, highly influenced by many factors, including among others, psychological, social, cultural, biological, historical and individual factors (Cash & Smolak, 2011).
Body image may be defined as the set of thoughts, feelings and perceptions of a person about his or her own body. Linked to the body image construct, usually is body image dissatisfaction (BID), defined as the negative thoughts, feelings and perceptions of a person about his or her own body. Body image dissatisfaction may be obtained through the difference a person considers to be between his or her, actual and ideal body image.
The level of body image dissatisfaction seems to be positively associated with the Body Mass Index (BMI) level. That association was demonstrated in the study of Runfola and colleagues (2013), in which obese women, of all weight groups, had the highest score in body image dissatisfaction. In turn, in the study of Swami and colleagues (2010), which assessed body image dissatisfaction in 26 countries, was found that BMI and occidental media exposure predicted body dissatisfaction in women. In the specific context of bariatric surgery, Grilo and colleagues (2005), found that women who were candidates for bariatric surgery, reported significantly higher body dissatisfaction, comparing to men.
Body image may be assessed through self-report questionnaires, projective tests, structured interviews, as well as through body silhouettes selection, with this last method being widely used. Body silhouettes selection consists of selecting an image that contains body contours or silhouettes (figurative scale). Stunkard, Sorenson and Schlusinger (1983), developed the first silhouette scale, which is currently the most used one.
In the literature, many silhouettes scales are described that aim to assess body image in different contexts. A systematic literature review study from Ferreira and Pereira (2016), identified the silhouettes scales used to assess the body image of adults with severe obesity, and only six studies were analyzed, due to the fact that many of the studies did not clearly discriminate the obesity level on theirs samples. Within these six studies, four silhouettes scales were used, and only two of them refer specifically that theirs figures are associated with BMIs higher than 35 kg/m2 (severe obesity). These are the Body Image Assessment for Obesity (BIA-O) (Williamson et al., 2000), which the validation study suggests it can be used with BMIs up to 50 kg/m2 and, the Silhouettes Figures Scale (Escala de Figuras de Silhuetas – EFS) (Kakeshita, Silva, Zanatta & Almeida, 2009), in which adult’s silhouettes BMIs vary between 12.5 kg/m2 and 47.5 kg/m2.
In the Portuguese context, it was not identified any silhouette scale specifically designed to assess body image of those with higher obesity levels or specifically dedicated to assess body image of bariatric surgery candidates to/who underwent surgery. Besides that, the only two scales found in the literature review by Ferreira and Pereira (2016), mentioned above don’t seem to be accurate enough for our bariatric patients. Although Body Image Assessment for Obesity (BIA-O) (Williamson et al., 2000) can be used with BMIs up to 50 kg/m2, the scale has 18 figures for each gender. The high number of figures could be seen has an advantage, but Gardner, Friedman and Jackson (1998), refer that data suggests most subjects tend to select from only three silhouettes within eight to twelve possibilities. So, there really seems to be no advantage in accuracy by using so many silhouettes. Furthermore the figures themselves don’t seem simple enough to facilitate the subjects’ perception. As for the Silhouettes Figures Scale (Escala de Figuras de Silhuetas – EFS) (Kakeshita, Silva, Zanatta & Almeida, 2009), its silhouettes don’t seem to be suitable for subjects with super obesity (BMI from 50 to 59.9 kg/m2) and super-super obesity (BMI higher than 60 kg/m2), once their highest BMI is 47.5 kg/m2.
Thus, this paper main goal is to evaluate the applicability of Obesity Surgery Silhouettes Scale (Escala de Silhuetas para Cirurgia da Obesidade – ESCO), specifically created to assess body image of patients candidates to/who underwent, bariatric surgery in the Portuguese population and, to describe the procedures involved in its development.
Then, we present the results of the administration of ESCO at a pre-test situation, in a small sample of candidates to bariatric surgery and community subjects.
Problem Statement
In Portugal, there are no silhouettes scales specifically designed to assess body image of bariatric surgery candidates, who have higher BMIs than most community subjects.
Research Questions
Is ESCO (Escala de Silhuetas para Cirurgia da Obesidade) capable of obtaining body image dissatisfaction indicators from candidates to bariatric surgery?
Purpose of the Study
This study main goal is to evaluate the applicability of Obesity Surgery Silhouettes Scale (Escala de Silhuetas para Cirurgia da Obesidade – ESCO), specifically created to assess body image of patients candidates to/who underwent, bariatric surgery in the Portuguese population and, to describe the procedures involved in its development.
Research Methods
Mixed methods were used, qualitative and quantitative methods.
Participants
The clinical sample had 20 obese subjects, candidates to bariatric surgery (17 women, 3 men,
The higher number of female subjects in the community sample was due to the replication of gender distribution in the population of patients candidates to/who underwent, bariatric surgery which consist mostly of women, as can be seen in this convenience clinical sample. This tendency can also be seen in the study of Ferreira and colleagues (2010), in which they accessed 162 candidates to bariatric surgery and only 32 of them where men.
Materials
Socio-demographic Questionnaire, to collect data, such as gender, age, schooling, profession, marital status, number of children, weight and height.
Body Mass Index (BMI), calculated taking the weight in kilograms, divided by height in square meters (weight/height2) (Seidell & Rissanen, 2004).
Obesity Surgery Silhouettes Scale (ESCO), is constituted by eleven black and white figures, distributed in ascending order across BMI categories, according to Mechanick and colleagues (2009) and the World Health Organization (WHO, 2000): Underweight <18.5 kg/m2; Normal from 18.5 to 24.9 kg/m2; Preobesity from 25.0 to 29.9 kg/m2; Class I obesity from 30.0 to 34.9 kg/m2; Class II obesity from 35.0 to 39.9 kg/m2; Class III obesity 40.0 to 49.9 kg/m2; Class IV obesity (super obesity) 50 to 59.9 kg/m2; Class V obesity (super-super obesity) ≥60 kg/m2. ESCO is constituted by representative figures of body volumes, which BMI lies among the following ranges: Figure
ESCO Administration Record Grid, to collect data, such as answering time, figures that raise doubts and, drawing style and color preferences. On this grid were also registered verbalized reflections by the subjects and their non-verbal behavior, while answering to the scale.
Procedure
For the procedures described next, were taken into account the National Data Protection Commission (Comissão Nacional de Protecção de Dados – CNPD) norms, ethical principles of the Helsinki Declaration (World Medical Association, 2013) and those that guide Psychology’s activity. Thus, all participants in this study were asked to sign an informed consent, attesting their voluntary cooperation, always safeguarding the confidentiality of obtained data. In order to collect data it was also requested an authorization from HESE – EPE’s Board of Directors.
The first ESCO figures were hand-drawn by a student of the Design course from Visual Arts and Design Department of Évora’s University. In a second moment, based on the three nutritionists' evaluation of ESCO, initial figures were digitally manipulated by a professional, until a consensual version between the nutritionists was obtained for each figure of each gender, male and female. There was concordance among the nutritionists, more than 90%, amid this panel of judges indicated an adequate validity, as referred by Krippendorf (2014). In a second moment, initial figures were digitally manipulated
Initially both ESCO’s genders scales were supposed to be constituted by 10 figures each, but when the nutritionists were trying to reach an agreement/consensus, the need to include an additional figure on both genders’ scales emerged. Thus, a figure was added to the higher BMI limit on each gender scale, to increase the instrument capability to assess body image dissatisfaction, also of patients with higher obesity classes (≥60 kg/m2).
ESCO was designed to assess body image of adults (≥18 years) of both genders, candidates to/submitted to bariatric surgery. This scale allows subjects to self-evaluate their current body size, as also their desired body size. Based on these two indicators, ESCO allows to measure the level of body image dissatisfaction (BID). This is obtained though the difference between current body image (CBI) and desired body image (DBI). The difference between CBI and DBI was validated as a measure of body dissatisfaction by Williamson, Gleaves, Watkins and Schlundt (1993) and is commonly accepted in the scientific community. Developing a silhouette scale requires some particular caution, besides those to be taken into account while developing any assessment instrument (Gardner, Friedman & Jackson, 1998). For example, special attention must be given to the absence of body details that may act as distractors (Thompson, 1996). Taking that into account, the ESCO’s figures have neutral expression faces and, simple hair and clothes. It is also important to maintain proportionality of body parts and to maintain a constant height among all the figures of the scale (Gardner et al., 1998). During the development of ESCO it was attempted, as far as it was possible, to increase each one of the figures in the same proportion, task that was facilitated by their digital manipulation. Besides that, all female figures have the same height amongst them, just like male figures. However, male figures are slightly higher than female figures, according to the difference between heights of Portuguese men and women. Once a consensual version of ESCO was obtained, the scale was administered to the clinical and community samples, to verify its applicability. In the clinical sample there were used two procedures of cognitive interviewing, verbal probing and thinking aloud (Priede & Farrall, 2011), in order to access more easily to the subjects’ subjective perception about ESCO. Verbal probing was used with ten out of twenty clinical sample subjects, in order to collect specific information about patients’ answering process, such as figures that raised doubts, drawing style preferences, preferences on colored figures, among others. The collected data was registered on the ESCO Administration Record Grid created for this purpose. Then, thinking aloud was used on the other ten subjects. The procedure involved the training of subjects with a sample image non-related to obesity, before the administration of ESCO and the transcription of the subject’s speech, on which they actively verbalized their thoughts through the answering process. Thinking aloud was not used within the whole sample, because we needed part of it to answer to the instructions as fast as possible (in order to measure the ESCO’s answering time) and this method didn’t allow that. In the community sample was used verbal probing, in the same way as described with the clinical sample.
Findings
In which concerns the bariatric candidates, ESCO was administered to 3 men (15%) and 17 women (85%). Participants mean age was 44.6 years, with a minimum 29 years and maximum age of 65 years. The schooling of the majority of the subjects was High School (30%), College (30%) and Elementary School (25%). The majority was employed (70%), while 15% were unemployed and 10% were retired. The rate of patients married or cohabiting was 75%. The majority had one (45%) or two (40%) children.
Mean answering time to the first ESCO’s instruction was 30.1 seconds, with a minimum of 10 seconds and a maximum of 114 seconds. Nine, out of the 10 subjects, answered within 10 to 37 seconds, and only one subject took 114 seconds. In turn, mean answering time to the second ESCO’s instruction was 25.8 seconds, with a minimum of 8 seconds and a maximum of 138 seconds. Nine subjects answered within 8 to 29 seconds and, only one subject took 138 seconds (the same subject that took more time in the previously instruction).
Participants mean BMI was 41.6 kg/m2, corresponding to the ESCO’s figure 7 (40 to 49.9 kg/m2), ranging between a minimum 35.8 kg/m2 and maximum 50.5 kg/m2.
Subjects mean self-evaluation of current body image, corresponded approximately to the ESCO’s figure 9 (8.9), indicating a BMI between 50 and 55.9 kg/m2. On the other hand, participants mean answers revealed they would like to have a body image corresponding approximately, to the ESCO’s figure 4 (3.8), corresponding to a BMI between 25 and 29.9 kg/m2.
The clinical sample mean body image dissatisfaction (BID) was 5.2, ranging from 3 to 8.
Body image dissatisfaction was correlated with age, BMI and education level. Pearson correlation coefficient was used to relate age and body image dissatisfaction, and the results did not show a statistically significant correlation (.143;
Besides the results presented above, given the exploratory and preliminary nature of this study, description of the subjects’ behavior during the administration of ESCO will be presented next.
As for the questions that arise during the administration of ESCO, two subjects (out of twenty) had doubts about the first instruction. One of them asked if he was supposed to place an X, although instructions clearly referred that a circle should be drawn around the figure’s number that matched the answer of the subject. Another subject only wanted to confirm if he was to draw a circle around the figure’s number.
During the answer to the first instruction, only one subject (out of twenty) expressed doubts, saying the figures should have their correspondent weight associated, this was the same subject that took more time to answer the instruction.
The facial expression of fifteen subjects while they were answering the first instruction was neutral and the facial expression of five subjects indicated indecision.
None of the subjects expressed doubts while answering the second instruction of ESCO, but when he was answering the second ESCO’s instruction, the same subject that expressed the need to have the correspondent weight associated to each figure, expressed the same need.
The facial expression of seventeen subjects during the second instruction was neutral, one of the subjects indicated indecision and two indicated amusement.
At the end of the scale administration, three questions were addressed to all subjects. When the following question was presented to the subjects
During the ESCO’s administration once we used the thinking aloud method, it became very clear that in order to make a choice, the first thing subjects noticed was the increasing size of the ESCO’s figures, representing an increasing weight. Then, very quickly they went from that macro analysis to a much more detailed analysis, once they had identified one or two figures within their weight range. In response to the ESCO’s first instruction, nine out of ten subjects identified a more or less sagging belly on the figures as a fundamental element for decision. Most of them, also focused on fat level of other body parts like the legs, arms and the more or less sagging breasts. A similar pattern of speech was registered during the response to the second ESCO’s instruction, although the subjects focused almost exclusively on the figures’ belly.
Regarding the community subjects, ESCO was administered to two men and eight women. Participants mean age was 41.7 years, ranging from 30 to 60.
Mean answering time to the first ESCO’s instruction was 13.2 seconds, with a minimum of 8 seconds and a maximum of 20 seconds. In turn, mean answering time to the second ESCO’s instruction was 8.2 seconds, with a minimum of 4 seconds and maximum of 14 seconds.
Participants mean BMI was 26.7 kg/m2, corresponding to the ESCO’s figure 4 (25 to 29.9 kg/m2), ranging between a minimum 20.1 kg/m2 and maximum 35.4 kg/m2. The subjects mean self-evaluation of current body image, corresponded to the ESCO’s figure 4 (4.4), which correspond to a BMI between 25 and 29.9 kg/m2. On the other hand, participants mean answers revealed they would like to have a body image corresponding to the ESCO’s figure 3 (2.9), which correspond to a BMI between 21 and 24.9 kg/m2. The community sample mean body image dissatisfaction (BID) was 1.5, ranging from 0 to 3.
As for the questions that arise during the administration of ESCO, only one subject expressed a question about the first instruction, seeking to confirm if a circle should be drawn around the answer’s number.
The facial expression of nine subjects while they were answering the first instruction was neutral and the facial expression of one subject indicated amusement. None of the subjects expressed doubts during the second ESCO’s instruction.
The facial expression of eight subjects during the second instruction was neutral, two subjects indicated indecision and one indicated amusement.
At the end of the administration of the scale, when the following question was addressed to the subjects
Conclusion
The subjects from the clinical sample revealed high discrepancy between their current body image evaluation (ESCO’s figure 9, corresponding to a BMI of 50 to 55.9 kg/m2), and their current BMI (mean of 42 kg/m2, corresponding to the ESCO’s figure 7), indicating a mean body size two figures above their current BMI. On the contrary, the subjects from the community sample evaluated their current body image (ESCO’s figure 4, corresponding to a BMI of 25 to 29.9 kg/m2), approximately to their current BMI (mean of 26.7 kg/m2, corresponding to the ESCO’ figure 4), indicating on average, a body volume consonant with the correspondent figure to their current BMI.
The fact that it was the clinical sample, that registered the greatest body image distortion, contradicts the tendency reported by some studies, in which overweight and obese subjects frequently underestimate their body size (Chang & Christakis, 2003; Truesdale, 2008). Perhaps the overestimation observed in our study would be explained by the high BMI of our clinical sample, which often leads to the subjects experiencing daily difficulties and stigmatization related to their appearance, reinforcing their image as extremely obese. Another possible explanation, may be related to the distribution of fat (Rhodes & O’Neil, 1997), because people with severe obesity have frequent abdominal obesity and upper body fat is more exposed.
On average, the subjects from the community sample would like to be one figure below their current body image evaluation, while the subjects from the clinical sample would like, on average, to be five figures below on ESCO. Thus, it was registered a higher body image dissatisfaction in the clinical sample subjects (BID=5.2), as the difference between the evaluation of the current body image (CBI) and the desired body image (DBI) was substantially superior on these, compared to the subjects in the community sample (BID=1.5). The greater body image dissatisfaction registered in the clinical sample, is aligned with the results from other studies available in the literature (e.g. Runfola et al., 2013; Swami et al., 2010). As expected, body image dissatisfaction increases with higher BMI, showing a statistically significant positive and elevated correlation, aligned with the speech of most bariatric patients at the psychological consultations before surgery. These patients often refer to their dissatisfaction with their body image and patients with higher BMIs frequently use very unpleasant adjectives about themselves and their bodies.
Globally, ESCO revealed to be an instrument of easy understanding and of extremely fast administration, as it was indicated by answering times, less than one minute on both instructions, for most subjects.
In turn, comparing the results obtained between the clinical sample and the community sample, considering the major discrepancy of results between the two samples, ESCO seems to be capable to assess body image dissatisfaction of obese patients, being sensitive to very high BMIs.
Using verbal probing and thinking aloud procedures, it became very useful to evaluate the impact of the ESCO’s figures on subjects from both samples, by recording their subjective perceptions.
Nevertheless, it is important to refer to the study’s limitations, inherent to its exploratory characteristics. One of them is the small and convenience sample size, justified by the pre-test nature of the study. Also, the reduced number of male subjects makes any gender comparison impossible.
Since the presented results, are drawn from a preliminary administration of the scale, for future research it is of most importance to verify how ESCO behaves in a bigger sample, representative of the population of bariatric surgery candidates, in order to validate the scale for the Portuguese population.
However, our findings suggest that ESCO seems capable of obtaining body image dissatisfaction indicators, that may be very useful to design specific psychological counseling programs for each patient candidate to/who underwent bariatric surgery. Furthermore, it will allow the use of body image dissatisfaction indicators as a result’s measure for bariatric surgery, other than weight loss or quality of life improvement. Thus, ESCO, as an instrument available to the health professionals working with these patients, may constitute an added value on the defiant task of counseling bariatric surgery patients.
Acknowledgments
We would like to thank Catarina Damas from Évora’s University, who hand-drawn the initial sketches of the figures, from which we started building ESCO. We would also like to thank David Prazeres from Hospital do Espírito Santo de Évora – EPE, who with great expertise was able to digitally manipulate the initial sketches to create the current ESCO.
References
- Adami, G. F., Gandolfo, P., Campostano, A., Meneghelli, A., Ravera, G., & Scopinaro, N. (1998). Body image and body weight in obese patients. International Journal of Eating Disorders, 24(3), 299-306.
- Alciati, A., D'Ambrosio, A., Foschi, D., Corsi, F., Mellado, C., & Angst, J. (2007). Bipolar spectrum disorders in severely obese patients seeking surgical treatment.Journal of Affective Disorders, 101(1-3), 131-138.
- Blackburn, G. L., Hutter, M. M., Harvey, A. M., Apovian, C. M., Boulton, H. R., Cummings, S., … Annas, C. L. (2009). Expert panel on weight loss surgery: Executive report update. Obesity (Silver Spring), 17(5), 842-862.
- Cash, T. F., & Smolak, L. (2011). Understanding body images: Historical and contemporary perspectives. In T. F. Cash & L. Smolak (Eds.), Body image: A handbook of science, practice, and prevention (pp. 3-11). New York, NY: Guilford Press.
- Chang, V. W., & Cristakis, N. A. (2003). Self-perception of weight appropriateness in the United States. American Journal of Preventive Medicine, 24, 332-339.
- Davis, M. M., Slish, K., Chao, C., & Cabana, M. D. (2006).National trends in bariatric surgery, 1996-2002. Archives of Surgery, 141(1), 71-74. doi:
- Fabricatore, A. N., Wadden, T. A., Sarwer, D. B., & Faith, M. S. (2005). Health-related quality of life and symptoms of depression in extremely obese persons seeking bariatric surgery. Obesity Surgery, 15(3), 304-309.
- Ferreira, A., & Pereira, A. (2016). Escalas de silhuetas para avaliar imagem corporal na obesidade grave: revisão sistemática [Silhouettes scales to assess body image on severe obesity: Systematic review]. In I. Leal, C. Godinho, S. Marques, P. Vitória, & J. L. Pais Ribeiro (Eds.) Livro de actas do 11º Congresso Nacional de Psicologia da Saúde [Proceedings of the 11th National Congress of Health Psychology] (pp. 803-809). Lisbon, Portugal: Sociedade Portuguesa de Psicologia da Saúde. Retrieved from http://www.sp-ps.pt/site/livros/141
- Ferreira, A., Santos, O., Pegacho, M., & Carvalho, M. (2010). Caracterização psicológica dos doentes candidatos a cirurgia bariátrica no Hospital do Espírito Santo de Évora [Psychological characterization of patients candidates to bariatric surgery at Hospital do Espírito Santo de Évora]. Endocrinologia, Diabetes & Obesidade, 4(4), 181-189. Retrieved from https://bibliotecadigital.ipb.pt/bitstream/10198/5415/3/endo-novembro%20final.pdf
- Gardner, R. M., Friedman, B. N., & Jackson, N. A. (1998). Methodological concerns when using silhouettes to measure body image. Perceptual and Motor Skills, 86(2), 387-395.
- Grilo, C. M., Masheb, R. M., Brody, M., Burke-Martindale, C. H., & Rothshild, B. S. (2005). Binge eating and self-esteem predict body image dissatisfaction among obese men and women seeking bariatric surgery. International Journal of Eating Disorders, 37, 347–351.
- Kakeshita, I. S., Silva, A. I., Zanatta, D. P., & Almeida, S. S. (2009). Construção e fidedignidade teste-reteste de escala de figuras brasileiras para adultos e crianças [Construction and test-retest reliability of the Brazilin figures scale for adults and children]. Psicologia: Teoria e Pesquisa, 25, 263-70.
- Krippendorff, K. (2014). Content Analysis: an introduction to its methodology. London, UK: Sage.
- Mathus-Vliegen, E. M., de Weerd, S., & de Wit, L. T. (2004). Health related quality-of-life in patients with morbid obesity after gastric banding for surgically induced weight loss. Surgery, 135(5), 489-497.
- Mechanick, J. I., Kushner, R. F., Sugerman, H. J., Gonzalez-Campoy, J. M., Collazo-Clavell, M. L., Spitz, A. F., … Dixon, J. (2009). American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery Medical Guidelines for Clinical Practice for the Perioperative Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery Patient. Obesity, 17(Suppl. 1), S1-S70.
- Ng, M., Fleming, T., Robinson, M., Thomson, B., Graetz, N., Margono, C., … Gakidou, E. (2014). Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet, 384(9945), 766-781.
- Priede, C., & Farrall, S. (2011). Comparing results from different styles of cognitive interviewing: ‘verbal probing’ vs. ‘thinking aloud’. International Journal of Social Research Methodology, 14(4), 271-287.
- Ray, E. C., Nickels, M. W., Sayeed, S., & Sax, H. C. (2003).Predicting success after gastric bypass: the role of psychosocial and behavioral factors. Surgery, 134(4), 555-563.
- Rhodes, S. K. & O’Neil, P. M. (1997). Effects of body fat distribution on body size estimation accuracy among obese women. International Journal of Obesity, 21, 250-253.
- Runfola C. D., Holle, A. V., Trace, S. E., Brownley, K. A., Hofmeier, S. M., Gagne, D. A., & Bulik, C. M. (2013). Body dissatisfaction in women across the lifespan: Results of the UNC-SELF and Gender and Body Image (GABI) studies. European Eating Disorders Review, 21(1), 52-9.
- Seidell, J. C., & Rissanen, A. M. (2004). Prevalence of obesity in adults: the global epidemic. In G. A. Bray& C. Bouchard (Eds.) Handbook of obesity: Etiology and pathophysiology (2nd ed., pp. 1005-1022). New York, NY: Marcel Dekker, Inc.
- Snyder, A. G. (2009). Psychological assessment of the patient undergoing bariatric surgery. Ochsner Journal, 9(3), 144-148.
- Stunkard, A. J., Sorenson, T., & Schlusinger, F. (1983). Use of the Danish adoption register for the study of obesity and thinness. In S. Kety, L. P. Rowland, R. L. Sidman, & S. W. Matthysse (Eds). The genetics of neurological and psychiatric disorders (pp. 115-20). New York, NY: Raven.
- Swami, F. D, Aavik, T., Alcalay, L., Allik, J., Anderson, D., Andrianto, S., … Zivcic-Becirevic, I. (2010) The attractive female body weight and female body dissatisfaction in 26 countries across 10 world regions: Results of the international body project I. Personality and Social Psychology Bulletin, 36(3), 309-25.
- Thompson, J. K. (1996). Body image, eating disorders, and obesity: An integrative guide for assessment and treatment. Washington DC: American Psychological Association.
- Truesdale, K. P. (2008). Do obese know they are obese? North Carolina Medical Journal, 69(3), 188-194. . Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3234679/
- Williamson, D. A., Gleaves, D. H., Watkins, P. C., & Schlundt D. G. (1993). Validation of self-ideal body size discrepancy as a measure of body dissatisfaction. Journal of Psychopathology and Behavioral Assessment, 15, 57-68.
- Williamson, D. A., Womble, L. G., Zucker, N. L., Reas, D. L., White, M. A., Blouin, D. C., & Greenway, F. (2000). Body image assessment for obesity (BIA-O): Development of a new procedure. International Journal of Obesity, 24(10), 1326-1332.
- World Health Organization (2000). Obesity: preventing and managing the global epidemic. WHO Obesity Technical Report Series, 894. Geneva, Switzerland: World Health Organization. Retrieved from http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/
- World Medical Association. (2013). World medical declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA, 310(20), 2191-2194
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
14 September 2017
Article Doi
eBook ISBN
978-1-80296-029-7
Publisher
Future Academy
Volume
30
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-376
Subjects
Health, public health, preventive healthcare, preventive care, preventive medicine
Cite this article as:
Ferreira, A. P., & Pereira, A. S. (2017). Development Of A Silhouette Scale For Bariatric Surgery (Esco): Preliminary Study. In Z. Bekirogullari, M. Y. Minas, & R. X. Thambusamy (Eds.), Health and Health Psychology - icH&Hpsy 2017, vol 30. European Proceedings of Social and Behavioural Sciences (pp. 12-23). Future Academy. https://doi.org/10.15405/epsbs.2017.09.2

