Abstract
Problem statement: Chronic obstructive pulmonary disease (COPD) is characterized by not fully reversible progressing bronchial obstruction connected to abnormal inflammatory response to adverse particles or gases. The consequences are grave. Research Questions: Is there a connection between the perception of the quality of life and COPD determinants? Purpose of the Study: The purpose of this study was to determine the quality of life of patients with COPD in connection to the gravity of the disease, its length and treatment. Research methods: The data was acquired using standardized questionnaires: Medical Outcome Study Short Form-36 (SF-36) to assess the quality of life, Medical Research Council (MRC) – modified dyspnoea scale and the Nottingham screening questionnaire for malnutrition risk assessment. 120 respondents partook in this research at the Clinic of Pulmonary Diseases and Tuberculosis – 61 men/59 women with COPD aged 30–92 (64 on average). Findings: The respondents' physical and mental health was assessed in 8 dimensions. Patients with the 3rd–4th stage of COPD feel significantly limited in the physical health dimension. Patients diagnosed with COPD more than 6 years ago feel less vital than patients diagnosed one year ago. Undergoing rescue treatment has an impact on social activity. Conclusion: The quality of life rapidly worsens in the 3rd and 4th stages of COPD in the physical activity dimension, general health assessment, vitality and social activity. However, the results cannot be generalized and the study is in progress.
Keywords: Obstructive pulmonary diseasequality of life
Introduction
Chronic obstructive pulmonary disease (COPD) is one of the main causes in terms of global and also Czech morbidity and mortality. Approximately 500 to 600 million people are suffering from this disease, out of whom 2.74 million die of this disease each year. Around 8% of the total population in the Czech Republic are suffering from this disease (Zatloukal, 2007, p. 301; Kašák, 2013). COPD is a lifelong, progressing disease enormously worsening life quality of the patients, often leading to permanent disability and premature death. COPD also has severe psychosocial impact. People suffering from this disease may experience a change or even a loss of their role in the family, partnership, loss of job, social isolation, or lack of understanding (Skoupá, 2014, p. 12). It only affects adult population. It is one of the most frequent diseases of the lower respiratory tract in the Czech Republic. It lies in gradual and irreversible bronchial obstruction. It is usually accompanied by chronic inflammation affecting not only the respiratory tract but the whole organism. Both hereditary and environmental factors contribute to the occurrence of COPD (Neumannová, Kolek, 2012, p. 79; Kolek et al., 2014, p. 131).
Chronic obstructive pulmonary disease
COPD is a curable disease that can be prevented. Its pulmonary component is characterized by obstruction to the air flow in the bronchi (bronchial obstruction) that is not fully reversible. Bronchial obstruction progresses and is connected to an abnormal inflammatory response to adverse particles or gases. COPD has significant extrapulmonary effects that can contribute to its severity in individual patients (Neumannová, Kolek, 2012, p. 79). The classic trio of symptoms includes cough, production of sputum, and exertion dyspnoea. Advanced stages are characterized by gradually progressing dyspnoea, significant limitation of exertion tolerance, the onset of cyanosis and chronic respiratory insufficiency, and manifestations of right-hand side cardiac failure within chronic cor pulmonale. This disease is often associated with many comorbidities, such as cardiovascular disease, cachexia, osteoporosis, depressions, or diabetes. These associated diseases must be actively sought and adequately treated (GOLD 2017, p. 24-26).
Diagnostics of COPD
The basic pillar of COPD diagnostics is a functional pulmonary examination focused on proving fixed bronchial obstruction that is not fully reversible on the administration of bronchodilatancia. Only patients in whom there is a suspicion that they have this disease based on their symptoms are examined. The key value is FEV1/FVC, the so-called Tiffeneau index. Post bronchial dilatation value of <0.70 is required in order to meet the diagnostic criteria (Kolek et al., 2014, p. 135-142). Chest x-ray is performed primarily in order to exclude complications – pneumonia, pneumothorax, or tumor. Arterial blood gases examination is indicated in patients with a rest SpO2<93% (Kolek et al., 2014, p. 135-142).
COPD Classification
According to the traditional division GOLD, the scale of bronchial obstruction, i.e. the value of postbronchodilatational FEV1, is the primary lead to establishing the severity of the disease. COPD is divided based on the severity of bronchial obstruction established by means of spirometry into 4 stages (I – mild, II - moderate, III - severe, IV – extremely severe). In patients in clinical stages II, III, and IV we find a decreased postbronchodilatational value of forced expiratory volume (FEV1) below 80% of the expected relevant values (Table
Inflammation and its subsequent pathological changes affect the respiratory tract, especially peripheral bronchi, pulmonary parenchyma and pulmonary arteries.
Besides chronic pulmonary inflammation structural changes resulting from repeated damage and repair are also present. The hypothesis of accelerated aging of the lung as a possible cause of COPD is considered. The disease is further assessed based on subjective problems of the patient, the frequency of exacerbations, and the phenotype (the scale of obstruction is characterized in the same way, only using an Arabic number). There are groups A to D based on the problems and risks (risk is given by the number of exacerbations per year), and two subscales of subjective problems of the patient – COPD Assessment Test (CAT) and mMRC (Koblížek, Chlumský, 2016, p. 2-4).
Phenotype classification is a bit simplifying as the phenotype does not necessarily be clearly expressed at the onset of the disease, or phenotypes may overlap. The key fact is that they can all develop to the stage of respiratory failure (GOLD 2017, p. 45).
COPD therapy
The goal of the COPD therapy is to remove the symptoms, improve tolerance to physical load, to prevent disease progression, to improve life quality, prevention and treatment of complications, prevention and treatment of exacerbations, and decreasing mortality (GOLD 2017, p. 45).
COPD therapy can be schemed into 4 basic steps – elimination of risks (giving up smoking immediately, anti-flu vaccination, etc.), causal treatment, phenotype treatment, chronic respiratory insufficiency treatment (GOLD 2017, p. 45). Less frequently mentioned but equally important is the treatment of all the present, especially cardiac comorbidities (cardiac failure, ischemic heart disease, atrial fibrillation, diabetes mellitus, etc.) (GOLD 2017, p. 45).
Causal treatment includes both pharmacological (mostly inhalation medication + vaccination) and nonpharmacological treatment (physical activity, pulmonary rehabilitation, education and training of inhalation techniques). In the treatment of COPD the basic medication is made up, according to the stage of the disease and the patient's symptoms, of inhalation ß2agonist with a long term to ultra long term effect (LABA, U-LABA) and inhalation antagonist of muscarinic receptors, also with a long term to ultra long term effect (LAMA, U-LAMA). Treatment must be modified in such a way so that it best responds to the health condition of the patient (Kašák, 2014, p. 406-407). Bronchodilatational and anti-inflammatory therapy is meant to improve the quality of life of the patient, decrease the frequency of COPD exacerbations, and limit the application of so-called rescue medication. In the treatment of COPD medication is gradually increased based on severity and the category of the disease (GOLD 2017). COPD with bronchiectases profits mainly from the administration of mucolytics, antibiotics, and physiotherapy. In patients with COPD who suffer from chronic respiratory insufficiency it is advisable to consider indications of so-called long term home oxygen therapy (Chlumský, 2016).
Even surgical therapy may be used in the treatment of COPD (e.g. LVRS - Lung Volume Reduction Surgery, bullectomy or BVR - bronchoscopic volume reduction. During the treatment of COPD with respiratory failure it is necessary to consider indicating lung transplant. If counter-indicated, it is time for end-of-life care with an emphasis on diminishing dyspnoea and the accompanying symptoms, ideally via hospice care (Kolek et al., 2014, p. 148-150; Fanta, Votruba and Neuwirth, 2004, p. 44-45).
Assessment of quality of life in case of bronchial obstruction
In COPD, the occurrence of which is strikingly higher than that of asthma, patients are relatively asymptomatic in early stages. They may not pay attention to chronic productive cough immediately from its onset. The main activities of daily life start to be limited only when FEV1 drops below 50% of its normal value. The fact that bronchial obstruction significantly affects the patient's life was verified using standardized questionnaires (Salajka, 2006, p. 60-61).
In practice there are a number of questions that are focused at life quality. Questionnaires can be divided into generic (general), and specific (focused on the given disease) (Němec, 2009). Generic questionnaires can be used to assess the differences between individual groups, or to assess their long term development. These include, for example, the Sickness Impact Profile (SIP) - 136 questions, the Nottingham Health Profile (NHP) – 45 questions, the Medical Outcomes Study Short Form (SF-36) – 36 questions, Quality of Well Being (QWB) – 50 questions focused on well-being SF-36 – 36 questions according to Ware.
The following questionnaires are considered as very good for assessing respiratory problems – the St. George Respiratory Questionnaire (SGRQ) – 76 questions, the Chronic Respiratory Disease Questionnaire (CRQ) – 20 questions, Breathing Problems Questionnaire (BPQ) – 33 questions and the Seattle Obstructive Lung Disease Questionnaire (SOLDQ) – 29 questions, etc.
Problem Statement
Quality of life can be divided based on objective and subjective standpoints. Subjective standpoint is more significant as it is the assessment made by the patient himself, as he perceives and feels his disease. Life quality is normally assessed using standardized life quality questionnaires. These map and assess the impact of the disease on the given individual, and the impact of the treatment itself on the patient's everyday life (Musil, Filip, 2011. p. 96-97). The main goal of this article was to determine life quality in patients with COPD in connection to the severity of the disease, its duration and treatment.
Research Question
Is there a connection between the perception of the quality of life and COPD determinants?
Purpose of the Study
Today's medicine can only inhibit the course of COPD, minimize the symptoms of the disease, prevent the onset of complications and COPD mortality, and/or delay them, and improve life quality of the patients (Kašák, 2006).
Research goals
The main goal of this article was to determine life quality in patients with COPD in connection to the severity of the disease, its duration and treatment. To this end, four partial goals were determined: 1) to find out whether it is women or men that suffer from COPD more frequently; 2) to find out whether it is patients with COPD stages III and IV or those with stages I and I that suffer from worse life quality; 3) to find a connection between the duration of the disease and life quality; 4) to find a connection between the application of rescue treatment and life quality. Four statistically verified zero hypotheses were set for the individual goals.
Pool of respondents and the organization of collecting data
120 respondents partook in this research at the Clinic of Pulmonary Diseases and Tuberculosis of Olomouc University Hospital – 61 men/59 women with COPD aged 30–92 (64 on average). The youngest respondent was 30 years old and the oldest 92. The average age of the respondents who partook in this research was 64.25 years of age. Data was collected using questionnaire research between November 2016 and January 2017. Participation in this research was conditioned by the patients' undertaking a spirometry examination in the course of the last month in order to determine the stage of COPD according to the FEV1 value, which can only be measured spirometrically.
The permission to carry out this research was granted prior to the beginning of the research. 120 properly filled out questionnaires were processed.
Research Methods
Three standardized questionnaires were used to collect the data: 1) the Medical Outcome Study Short From - 36 (SF-36); 2) the mMRC questionnaire; 3) the Nottingham Screening Questionnaire for the assessment of malnutrition risks.
The SF-36 Questionnaire
The SF-36 health survey is a 36-question abridged version that classifies life quality through age composition. This survey was published in 1992 by Ware and Sherbourne (Ware and Sherbourne, 1992; McHorney, Ware and Raczek, 1993). In its current form the SF-36 is a trademark of the Medical Outcomes Trust. The survey is divided into 8 subcategories and two main categories (physical and mental health). The 36-question survey includes an 8-dimension selection scale: A – Physical Functioning, B – Role-Physical, C –Bodily Pain, D – General Health (5 questions), E – Vitality (4 questions), F – Social Functioning (2 questions), G – Role Emotional (3 questions), H – Mental Health (5 questions). One question does not fall into any area/dimension. This question is focused on the current health condition compared to that one year ago (Kalantar-Zadeh et al., 2003; Musil- Filip, 2011; Kalantar-Zadeh et al., 2003; SF-36v2 Health Survey, © 2017).
Own assessment of the survey is realized as a scoring algorithm calculated for each dimension individually. These dimensions take up the values of 0 – 100, where the lowest value means a generally worse value of the given dimension, thus lowering overall life quality, and vice versa. The resulting values are calculated as the arithmetical mean of the individual answers. For easier interpretation, the individual dimensions of this survey were further divided into two scales specially assessing overall physical health (PCS-Physical Component Summary) and mental health (MCS - Mental Component Summary). The higher the score the better total physical/mental health (Kalantar-Zadeh et al., 2003; Ware J. E., 2004; SF-36v2 Health Survey, © 2017).
The mMRC scale
The mMRC (Medical Research Council) scale is a modified dyspnoea scale that assesses degrees of dyspnoea using 5 questions. It is a semi-quantitative assessment of dyspnoea symptoms for persons with COPD. Answers are given zero (no dyspnoea) to four points (I feel dyspnoea at minimum exertion) (Evans et al., 2009; Topinková, 2005).
The Nottingham Screening Questionnaire
The Nottingham screening questionnaire is the most frequently used system evaluating the state of nutrition while focused on the BMI, unwanted weight loss in the past three months, reduction of food intake in the past 3 months, reduction of food intake in the past one month, and the stress factor, which illustrates the patient's basic diseases (Nováková, 2012, s. 102 podle Sobotka, Basics in Clinical Nutrition, 2000).
Findings
Among the respondents that took part in the research there were 30 (25.00%) nonsmokers, 41 (34.20%) smokers, 4 (3.30%) passive smokers, and 45 (37.50%) former smokers.
Only 4 of them had their BMI below 18 (3.33%), 26 had their BMI 18-20 (21.66%), and the majority of respondents – 90 (75.00%) had their BMI value higher than 20.
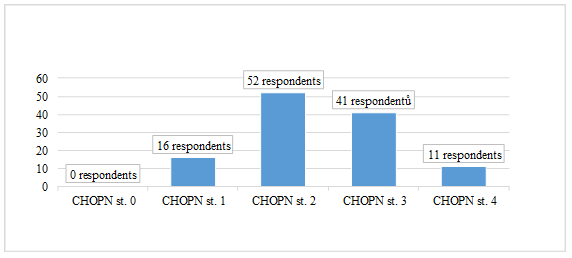
The most respondents were in the COPD stages 2 (52) and 3 (41) – for more see Figure
While asked what kind of treatment they were using for COPD, most respondents answered that they were taking long-term treatment to battle COPD together with rescue treatment – 63 (52.40%) respondents, 28 (23.40%) respondents were only taking rescue treatment.
Assessment of mMRC
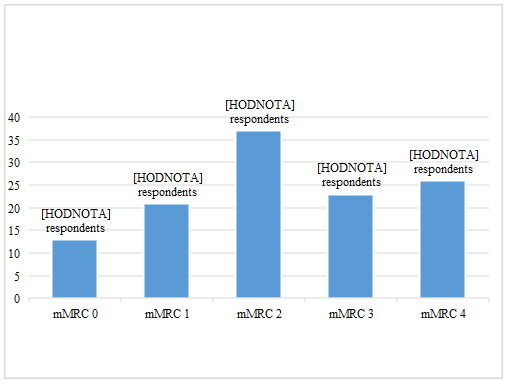
The results have shown (Figure

Assessment of the Nottingham Screening Questionnaire
The score of 5 and more points suggests life threatening malnutrition. A total of 24 respondents achieved this score. The score of 3 to 4 points signals the risk of malnutrition. A total of 15 students achieved this score. Scoring 0-2 points (the standard) the respondent does not need a nutritional therapist or special support. A total of 81 respondents achieved the normal number of points – see Table
Assessment of SF-36
Statistically significant differences between patients undergoing and not undergoing rescue treatment were found in all the dimensions except for the perception of pain. In all the items where a statistically significant difference was proven, the patients undergoing rescue treatment achieved a lower score of life quality assessment.
Then using
Using the
Using the
Conclusion
In the selected group of respondents (gender, duration of disease, COPD stage, last value of FEV1 from the last spirometry in %, way of treatment, BMI), physical and mental health were assessed in 8 dimensions. We managed to prove that patients with a severe or extremely severe stage (III or IV) of COPD felt statistically significantly limited in the physical health dimension. In the vitality dimension, patients with COPD diagnosed for more than 6 years felt less vital than those diagnosed with it one year ago. Undergoing rescue treatment has an influence on life quality. That is why early diagnostics and adequate treatment are important in these patients. The most important are giving up smoking permanently, regular monitoring of the patient, and ceaseless education including the family. Multidisciplinary approach of all fields of expertise caring for the patient and his comorbidities is inevitable. With the patient's active approach and using the full potential of health care a full-fledged life of the patient can be ensured.
References
- Evans, R. A. et al., 2009. Pulmonary rehabilitation is successful for COPD irrespective of MRC dyspnoea grade. Respiratory Medicine [online]. Vol. 103, No. 7, s. 1070-1075 [cit. 2017-04-26]. Dostupné z:
- Fanta J., Votruba J., Neuwirth J., 2004. Lvrs Chirurgická léčba emfyzému plic. Praha: Grada. ISBN 8024703696.
- Gold, 2017. Global Strategy For The Diagnosis, Management, And Prevention Of Chronic Obstructive Pulmonary Disease (2017 Report) [online]. [cit. 2017-03-12]. Dostupné z: http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/
- Kalantar-Zadeh, K. et al., 2003. Quality of life in patients with chonic renal failure. In: CIN´2003: 3th Congress of Nephrology in Internet [online]. [cit. 2017-04-12]. Dostupné z: http://www.uninet.edu/cin2003/conf/kalantar/kalantar.html
- Kašák, Viktor, c2006. Chronická obstrukční plicní nemoc: průvodce ošetřujícího lékaře. Praha: Maxdorf. Farmakoterapie pro praxi. ISBN 80-7345-082-8.
- Kašák, V., 2014. Farmakoterapie chronických nemocí s bronchiální obstrukcí. Farmakoterapie, 2014; 4: 406–407.
- Kašák, Viktor, 2013. Chopn v České republice v roce 2013. Postgraduální medicína [online]. 03/2013 [cit. 2016-11-18]. Dostupné z: http://zdravi.euro.cz/clanek/postgradualni-medicina/chopn-v-ceske-republice-v-roce-2013-469569
- Koblížek V., Chlumský J., 2016. Doporučený postup ČPFS pro diagnostiku a léčbu stabilní CHOPN [online]. [cit. 2017-01-20]. Dostupné z: http://www.pneumologie.cz/guidelines/
- Kolek V. et al., 2014. Pneumologie, 2. vydání. Praha: Maxdorf. ISBN 978-80-7345-387-9.
- Mchorney, Colleen A., WARE, John E., Jr. a Anastasia E. RACZEK, 1993. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical test of validity in measuring psychical and mental health constructs. Medical Care. Vol. 31, No. 3, s. 247-263. ISSN 0025-7079.
- Musil, David A Libor Filip, 2011. Hodnocení kvality života pacientů jeden rok po implantaci TEP kyčelního kloubu (z MIS-AL přístupu pomocí dotazníku SF-36). KONTAKT: Časopis pro ošetřovatelství a sociální vědy ve zdraví a nemoc. Roč. 2011, č. 1, s. 95-103. ISSN 1212-4117.
- Němec, F. et al., 2009. Hodnocení kvality života pacientů s degenerativním onemocněním bederní páteře. Acta chirurgiae orthopaedicae et traumatologiae čechoslovaca [online]. Roč. 76, č. 1, s. 20-24 [cit. 2017-02-19]. Dostupné z: http://www.achot.cz/dwnld/0901_020_024.pdf
- NEUMANNOVÁ, Kateřina A Vítězslav KOLEK, 2012. Asthma bronchiale a chronická obstrukční plicní nemoc: možnosti komplexní léčby z pohledu fyzioterapeuta. Praha: Mladá fronta. Aeskulap. ISBN 978-80-204-2617-8.
- Nováková, Martina, 2012. Fragilita geriatrického pacienta– možnosti řešení. Interní medicína pro praxi [online]. Roč. 14, č. 3, s. 101-103 [cit. 2017-02-02]. Dostupné z: https://www.internimedicina.cz/pdfs/int/2012/03/03.pdf
- Salajka, František, 2006. Hodnocení kvality života u nemocných s bronchiální obstrukcí. Praha: Grada. ISBN 80-247-1306-3.
- SF-36v2 Health Survey, © 2017. In: Optum [online]. [cit. 2017-04-20]. Dostupné z: https://campaign.optum.com/optum-outcomes/what-we-do/health-surveys/sf-36v2-health-survey.html
- Zatloukal, J. 2007. Novinky v terapii CHOPN. Medicína pro praxi: časopis praktických lékařů [online]. Roč. 4, č. 7–8, s. 301-304 [cit. 2016-11-25]. ISSN 1214-8687. Dostupné z: http://www.medicinapropraxi.cz/pdfs/med/2007/07/05.pdf
- Ware, John. E., Jr. A Sherbourne, Cathy Donald, 1992. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Medical Care. Vol. 30, No. 6, s. 473-483. ISSN 0025-7079.
- Ware, E. J., 2004. SF-36 Health Survey Update. In: The Use of Psychological Testing for
- Treatment Planning and Outcome Assessment [online]. New Jersey: Lawrence Erlbaum
- Associates, vol. 3, s. 693-718. [cit. 2017-04-12]. Dostupné z:
- http://www.sf-36.org/announcements/Updated_SF36_bookChapter_Sept04.pdf
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
14 September 2017
Article Doi
eBook ISBN
978-1-80296-029-7
Publisher
Future Academy
Volume
30
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-376
Subjects
Health, public health, preventive healthcare, preventive care, preventive medicine
Cite this article as:
Kudlová, P., & Brozová, Z. (2017). Quality Of Life Of Patients With Chronic Obstructive Pulmonary Disease. In Z. Bekirogullari, M. Y. Minas, & R. X. Thambusamy (Eds.), Health and Health Psychology - icH&Hpsy 2017, vol 30. European Proceedings of Social and Behavioural Sciences (pp. 134-145). Future Academy. https://doi.org/10.15405/epsbs.2017.09.13

