Abstract
Temporo-mandibular joint pathology is one of deficiencies quite common lately in prosthetics, oral and amxillo-facial service. Between 2012-2016 we assesed a wide range of patients who presented with temporo mandibular joint dysfuction level correlated with other pathologies, both local and general, order with a total of 42. In our study we chose patients experiencing TMJ pathology who needed prosthetic rehabilitation. The first element required was a anamnesis rigorously conducted after which it was examined the patient clinically by inspection palpation, percussion, finding the subjective and objective signs and the nature of dysfunction at the muscular or articular level indicated by the laboratory tests: OPG and tomography ATM after which Riketz Burlui balance was achieved - and a morphological analysis at the mandibular condyle. After this we determined the cranio-mandibular relationship of posture and relationship centric we make the personal ocluzogram and we checked the parameters of occlusion describing the static and dynamic occlusion. Following a positive diagnosis itself it follow the stage of treatment customized depending on the case consisting in miorelaxing drugs accompanied by mouthguards and interventions on occlusal areas completed with kinetoterapy exercises and balneophisioterapy finalizing with fixed and mobile prosthetic rehabilitation trying to obstain homeostasis of stomatoghnatic system.
Keywords: Social casesTMJ disordersclinical examinationprosthetic treatmenthomeostasis
Introduction
Temporomandibular disorders (TMD) are defined as ‘a collective’ term embracing a number of clinical problems that involve the masticatory muscles, the temporomandibular joint (TMJ) and associated structures, or both like said Miettinen, Lahti and Sipilä, (2012).The management of temporomandibular joint (TMJ) dysfunction may be a difficult challenge to the dentistry and medical professions,that often requires a multidisciplinary approach to diagnosis and treatment in the opinion of Sarlani, Balciunas & Grace (2005), so for this situation is it necessary a multidisciplinary team: neurologist, otolaryngologist, dentist and psychiatrist. Data from literature show that the prevalence of TMD symptoms and signs are common in the population the and TMJ dysfunction is more prevalent among female gender (1.5-2 times), possible because there are a summation of the pain from this area, but there is evidence that the central nociceptive processing is up regulated at women compared to men, the prevalence was significantly higher among younger women, among women of lower socio-economic status, like said Janal, Raphael, Nayak, and Klausner (2008) and also literature said that TMD are twice as common in the general population than among men, and in a TMD patient population the proportion of women is as much as 4-times higher than the proportion of men (Okeson, 2008). The maximum number of the patients occurring in female gender subjects aged 20-39 (of reproductive age) and the lowest among children, adolescents, and the elderly (Warren & Fried, 2001; Nekora-Azak, 2004). Because their etiologies and pathogenesis are poorly understood, temporomandibular joint (TMJ) diseases are difficult to diagnose and manage. All current approaches to treatments of TMJ diseases are largely palliative like said Sunil and Sunil (2008).
Problem Statement
Making in a wrong manner the prosthetic treatments by the insufficiency of occlusal echilibration - or the incomplete realisation of the prosthetic treatment (different reasons: economical, time) or the absence of it can lead to arrive on the great field of TMJ disorders or dysfunction.
Research Questions
It is possible that by doing occlusal prosthetics equilibration in association balneofisiokinetoterapy with miorelaxing medication and occlusal splints to obtain TMJ dysfunction treatment?
Purpose of the Study
The aim of this research was the evaluation of the patients with TMJ disorders, social cases, who presented at our groups of students in practical laboratory of fixed and amovible prosthesis, between 2012-2016.
Research Methods
The principal research methods are the tipical and regular modalities used for investigation by our dental university from the last years that consist in the following procedure: starting with general part like patients history, family history and succeeding with the detailed, clinical examination of the patients. In the large aria of extraoral examination we have the interest in the TMJ examination with the inspection, palpation and auscultation, the examination of the facial muscles by inspection and palpation, the inducing and checking the landmarks of the posture relation , the centric relation, after this the elaborately intraoral examination with the identification of parameters of occlusion on the documentary cast in comparison with clinical observation of them, following with the Angle key and also the graphic representation of personal occlusograme inspired on the documentary casts in complicity with clinical examination using the articulation paper. In the ending of intraoral examination we took into observation the dynamic occlusion with the “position –test” and “moving- test” on the active part, and the desocclusion- phenomenon Christensen on the inactive part and in assessing and completing with objective interpretation of the laboratory tests. Each clinical examination is bilateral, symmetrical and comparative. After establishing a correct diagnostic we started doing the occlusal grinding using different kind of methods Barell, Yankelson etc. in association with adjuvants treatments physiokinetoterapy, miorelaxing drugs, applying occlusal splints ending the treatment with different, individuals manners for prosthetical rehabilitation.
Findings
This descriptive study included a number of 42 patients from Romania who came for TMJ disorders at our clinical laboratory as patients at students in scale practical work.
Selection criteria were: all the patients with TMJ disorders, TMJ and muscular affectation, deviation of mandible from the medial line during the mouth opening, paraclinical examination observation. Exclusion criteria were: presence of cancer, contagious lesions, pregnancy and third molar pathology. The gender distribution of the patients that are presented with TMJ dysfunction in this study included 24 female subjects (57.14%) and 18 male individuals (42.86%), aging between 16 and 83 years, which presented clinical signs of articular dysfunction, a decrease or an increase of muscular tonus, with a keen interest regarding the affliction of stomatognathic system and a heighten concern considering the recuperation of the already reduce functions of the system. They are, with a modest social position: students (9.52%), retirees (35.71%) and unemployed (54.76%).
Regarding the addressability of urban and rural population at dental treatment, we can note a preponderance of the urban than the rural environment. Maximum of addressability exists in the population group of 40-59 years (54.76%), without neglecting the other age groups, 20-39 (9.52%) and 60-79 years (11.90%).
The debut was a history rigorously conducted from where we concluded that the hypertension and cardiovascular pathology was most frequent pathology (19.05%) after this asthma (7.14%) and surgical intervention (9.52%), myocardial infarction (4.76%), chronic bronchitis (4.76%), hepatitis (7.14%), gastritis (14.29%), diabetes (11.90%), kidney failure (4.76%) and varicose (4.76%).
After this part we started with clinical examination of each patient:
Extra-oral examination, where we determined
The contour of the face: round (11.90%), oval (7.14%), triangle (21.43%), trapezoidal (23.81%), rectangular (26.19%) and square (9.52%);
The constitutional type: respirator (45.24%), digestive (26.19%) and cerebral (21.43%).
The symmetry of the face in transversal way static symmetry and dynamic symmetry and the facial symmetry in vertical direction:
The level of the face measured with anthropometric methods like (were obtained approximate values in mm making an average of measurements obtained from patients included in the study around the following values):
Leonardo da Vinci Sn–N = 56-58 mm; Sn-Gn = 51-56 mm;
Leonardo da Vinci modified Sn–Oph = 62-64 mm; Sn-Gn = 51-56 mm;
Boianov Ch-Ch= 60-64 mm; St-Gn= 58-62 mm;
Boianov modified St-Gn = 58-62 mm = bipupilar line= 60-62 mm;
Willis method Sn-Gn =58-62 mm = labial slot–slot eyelid 60-63 mm;
Golden Appendrodt compass methods Sn–Gn= 58-62 mm (open mouth)/Sn Gn (mouth close) 60 mm.
We continue with the examination of the TMJ with subjective symptoms like: pain (35.71%), noises (66.67%), joint looking (2.38%) and unable of mouth closing (2.38%). We are interested in:
Location: right (35.71%) or left (28.57%), bilateral (7.14%);
Starting moment: morning (9.52%), lunch (33.33%) or in the evening (11.90%);
Duration: permanent (4.76%), only creates a discomfort (35.71%);
Intensity: high (7.14%) or lower intensity (28.57%);
Frequency: frequent (28.57%) or rare (23.81%) cause of pain.
Objectively we do the examination by inspection of pretragian zone and menton, in static and dynamic, asking the patient to do the opening of the mouth observing that are presenting pathological sings like: the pretragian zone must be covered by a normally tegument, symmetric, without deformation (78.57%), scarfs (11.90%) or moles (4.76%) and deviation of the mandible (menthon), in static (11.90%) and in dynamic (40.48%).
From lateral side we can see the modification of the arch in person in bayonet (52.38%).
From palpation point of view, in static we examine the centration of the condyle in the glenoide fossa, the cutaneous projection of external pole of condyle, and also the palpation with two fingers: the thumb on the tragus and the index in auditory meatus when we feel the asynergy at the beginning (11.90%) and the finality of the movement (21.43%) of TMJ and we observed at our cases that the right condyle precedes the movement of left condyle (33.33%) and the palpation with four fingers on the pretragian zone when we feel the complete trajectory with the left condyle precedes the movement of the right (35.71%).
The auscultation provides information regarding the articular noises. Their localization can be on the right (54.76%) and to the left (26.19%) and their moment of occurrence is the mouth opening (26.19%) and also in closing (50.00%) and during mandibular dynamic trajectories (26.19%). The noises can be unique of high intensity-clickings (33.33%), or can be multiple of low intensity called crepitation (52.38%).
The examination of articular mobility is performed by exploring the vertical mobility open close movements or the horizontal mobility: propulsory, retropulsory, laterality, latero-pulsory movements.
The opening of the mouth is performed at maximum amplitude and it is measured in millimetres using Boley gauge or the ruler and measuring the distance between the maxillary and mandibular incisor edges along the medio-sagittal line. Normally the mouth opening amplitude is 40 mm ± 5mm. Our patients (11.90%) have the 39 mm (30.95%) 38 mm and the rest 40 mm. The closing of the mouth must be examined in the some way like the trajectory followed by mandibular inter-incisive point the terminal position at maximum inter-cuspidation the accompanying articular salt and noises.
The propulsion movement of the mandible the forward movement of the mandible without dental contact allows testing the antero-posterior resilience of the TMJ the amplitude during maximum propulsion is measured on the middle line between the incisor edge of the mandibular incisors and the vestibular surface on the maxillary ones. The normal value of this amplitude must not be higher than 9-11 mm. We find (4.76% of cases) 1 mm, (11.90% of cases) 2 mm, (23.81% of cases) 5 mm, (28.57% of cases) 8 mm and (11.90% of cases) 9 mm. Apart from examining the movement amplitude the trajectory of the inferior inter-incisive point is also observed witch should normally be straight and on the middle line and pathologic it may be deviated left (28.57%) or right (26.19%) or it may present an alternative shape (11.90%).
Retropulsion, the posterior movement on the middle line of the mandible starting from a maximum inter-cuspidation towards the central relation the movement amplitude is moderate 0.2–1.7 mm, even null in some cases, (28.57% of cases) 0.2 mm, (30.95% of cases) 0.3 mm and (40.48% of cases) 1 mm.
Laterality right or left is made by moving the mandible to the maximum side with half open mouth, its measurement being performed between the maxillary and mandibular inter-incisal points, the reference will be made at the medio-sagittal plane. The normal value of this movement is around 9 mm; a value under 6 mm is pathologic. We examined at our cases (35.71% of cases) 7 mm, (7.14% of cases) 2 mm, (33.33% of cases) 6 mm and (23.81% of cases) 9 mm.
As far as the interpretation of the results is concerned we may conclude the following a mouth opening limitation with a normal propulsion and laterality has a muscular aetiology a mouth opening limitation with an alteration of the laterality movement has probable articular aetiology.
The clinical examination of the oro-facial muscles follows the some steps, respectively a subjective and objective examination.
The objective examination is made by inspection and palpation statically and dynamically in rest position, centric and during active muscular contraction. Our patients report the either spontaneous appearance of muscular pain (11.90%) or provoked by mandible movement (23.81%) or by touching the muscle mass of the muscle insertion (14.28%). Another subjective complaint of the patients may is the increase of the muscular mass consistency- hypertonia (9.52%), also the patients complained about the presence of the muscular spasm (4.76%), always accompanied by intense pain. The interested muscular mass and by functional disability, patients observed a muscular hypertrophy level masseter (11.90%) and the temporal (16.67%).
Also we can observe the patients with muscular fatigue (11.90%), the limitation of mandibular movement (7.14%) and the modification of the mandibular dynamic trajectories (35.71%).
The objective examination is done by inspection and palpation of the system muscle, the muscular insertion and the muscular mass will be examined bilateral and symmetric. The elevator muscle of the mandible like the temporal normal tonicity (23.81% of cases) hipercontraction, the masseter muscle (26.19% of cases) hipercontraction, the internal pterigoid muscle (4.76% of cases) hipercontraction, the propulsory muscle of the mandible the external pterigoid muscle (4.76% of cases), hipercontraction the depressor muscle the mylohyoid muscle normal tonicity, the geniohyoid normal tonicity, the digastric muscle normal tonicity. The indirect depressor muscle of the mandible, the posterior belly of the digastric muscle,has normal tonicity, and also the styloid muscle has hipercontraction (4.76% of cases), the sternohyoid omohyoid and tyrohyoid muscles are normal tonicity. The retropulsor muscle of the mandible sternocleidomastoid has also hipercontraction (4.76% of cases).
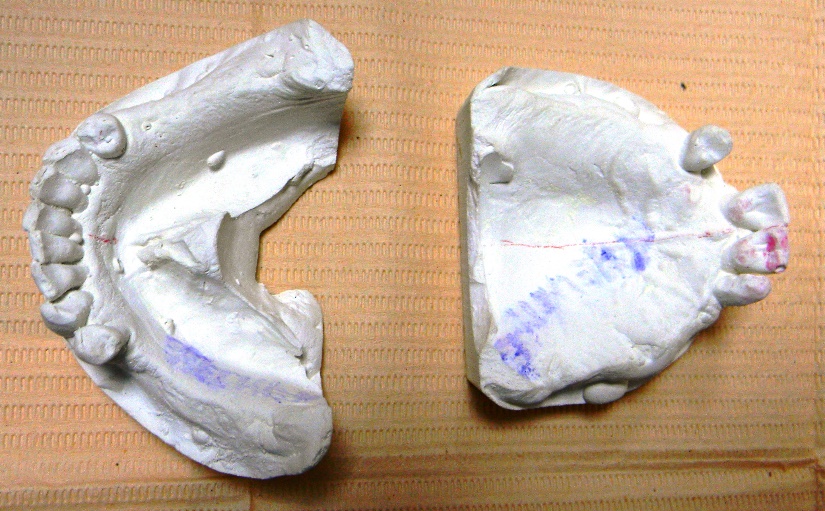
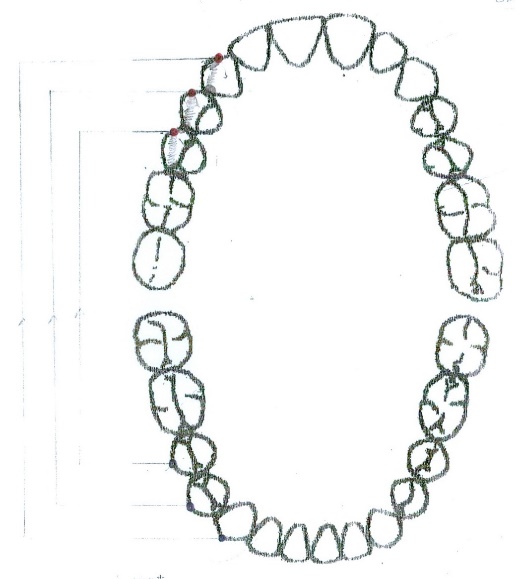
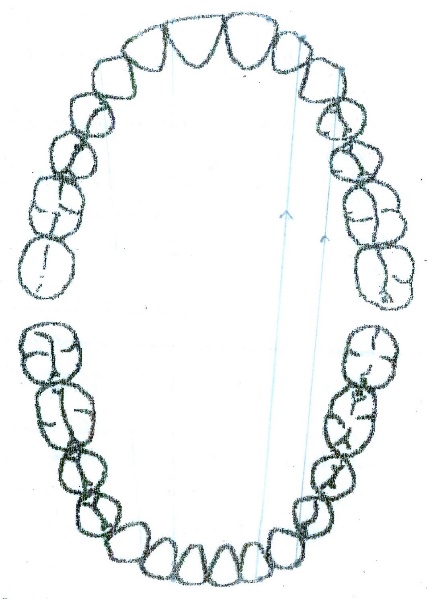
The situation at the first visit of our patient is illustrated on the documentary casts (figure
01 ), the OPG( ortopantomography) (figure02 ), and the clinical situation of maxillary and mandibular arch with and without ancient prosthesis.
On ATM tomography (figure

![ATM tomography – selective clinical cases from Dental clinic Based “M. Kogalniceanu” Iași]](https://www.europeanproceedings.com/files/data/article/58/2151/MEPDEV2016FA086.fig.003.jpg)
At our patients we can find the right condyle modified form (30.95% of cases) and left (28.57% of cases); modification of the interlinium spaces right (26.19% of cases) and left (19.05% of cases).
The method of inducing and checking the RP (posture relation) is relaxing the patient in order to make him aware of the relaxation position, they must reach with a little exercise like test of counting from 60 to 70, or another fonetical test Robinson, Silvermann and a good relaxation induced by medication the patient may enter more or spontaneous in rest position, than we are ensure that the following benchmarks are respected:
Articular must be condyles centrated in the glenoid fossae at the patients with point centric (2.38%) or towards the front at the patients with long centric (97.62%), the condyle is palpable at both sides;
Muscular antigravific tonic muscular balance (42.86% hypercontraction);
Bones corresponding median lines correct vertical dimension:
Sn-Gn = 50 mm (23.81%), 52 mm (23.81%), 53 mm (23.81%), 54 mm (16.67%), 56 mm (11.90%);
Sn-N = 51.8 (4.76% of cases), 54.5 mm (40.48% of cases), 56 mm (23.81% of cases), 57 mm (11.90% of cases), 59 mm (11.90% of cases).
Dental free space of phonetic articulation present in 4.76% of cases the normal value, 2-4 mm (1.8); in 40.48% of cases, 2.5 mm and in 47.62% of cases, 3 mm.
Labial lips in unforced contact (in 80.95% of cases),
Lingual space between the back side of the tongue and the palatal arch space of Donders.
Centric relation (RC) is induced by different methods like: Lauritzen Barelle (7.14%), Dowson (38.10%) and also Ramfjord methods (33.33%) the rest with occlusion models.
After, we are thinking that we obtain a centric relation we checking the benchmarks:
Articular: condyles centred in glenoid fossa, condyle is palpable;
Muscular: the muscle is in balanced contraction (42.86% of cases hypercontraction);
Bones: Sn-Gn = 50 mm (23.81% of cases), 52 mm (23.81% of cases), 53 mm (23.81% of cases), 54 mm (16.67% of cases), 56 mm (11.90% of cases); Sn-N = 48 mm (14.29% of cases), 49 mm (9.52% of cases), 51 mm (21.43% of cases), 52 mm (2.38% of cases), 53 mm (23.81% of cases), 53 mm (14.29% of cases) 54 mm (2.38% of cases), 56 mm (11.90% of cases).
Dental contacts type long centric or points centric are: long centric (97.62% cases) and point centric (2.38% of cases).
The occlusion relationship is especially complex and it must be approached in a tridimensional static and dynamic manner interfering and intervening with all the systemic functions and define the occlusion relationship.
The following elements are considered to be important the parameters of occlusion the static occlusal relation, the dynamic occlusal relations.
The parameters of occlusion are reprezented by:
The occlusion areas: naturals (4.76% of cases), artificial (7.14% of cases), mixed (88.10% of cases); short (88.10% of cases), interrupted (59.52% of cases), continuous (9.52% of cases), discontinuous (4.76% of cases);
The sagittal curve of occlusion: naturals (4.76% of cases), artificial (7.14% of cases), mixed (88.10% of cases), irregular (11.90% of cases), short (88.10% of cases), interrupted (59.52% of cases), accentuate concave (4.76% of cases), oblate (11.90% of cases), inverse (2.38% of cases);
The transverse curve of occlusion: naturals (4.76% of cases), artificial (7.14% of cases), mixed (59.52% of cases), irregulars (7.14% of cases), lingualized (16.67% of cases), normal (19.05% of cases), vestibularized (11.90% of cases);
The supporting cusps: naturals (4.76% of cases), artificial (7.14% of cases), mixed (54.76% of cases) medium dimension;
The guiding cusps: naturals (4.76% of cases), artificial (7.14% of cases), mixed (52.38% of cases), medium dimension;
The anterior guidance, morphological point of view: natural (4.76% of cases), artificial (7.14% of cases), mixed (50.00% of cases), continuous (16.67% of cases), discontinuous (4.76% of cases), interrupted (11.90% of cases); functional point of view trajectory is deviated to the right (33.33% of cases), left (28.57% of cases) and normally the rest;
The front curve: natural (4.76% of cases), artificial (7.14% of cases), mixed (50.00% of cases), continuous (16.67% of cases), discontinuous (4.76% of cases), interrupted (11.90% of cases). Convex (16.67% of cases), accentuated convex (19.05% of cases), oblate (2.38% of cases), irregular (2.38% of cases, maxillary; 14.29% of cases, mandibular);
The occlusion plane, virtual plane that has 17 degrees with the floor plane.
The static relations: the Angle key:
In sagittal plane:
The molar reference we have: normal- class 1 Angle at 11.90% of cases, right side 7.14% of cases 2 mm mezialization, 11.90% of cases distalization 2 mm, 16.67% of cases left side, 11.90% of cases mezialization 1 mm, 9.52% of cases distalization 3 mm;
The premolar reference classe 1 Angle at 16.67% of cases, right side 7.14% of cases mezialization 2 mm, 11.90% of cases distalization 2 mm / 19.05% of cases left side, 9.52% of cases mezialization 1 mm, 9.52% of cases distalization 3 mm;
The canin 23.81% of cases classe 1 Angle right side / 23.81% of cases classe 1 Angle left side;
The incisal reference overjet normal 57.14% of cases, 4.76% of cases 0 mm, 16.67% of cases sagittal innoclusion, 7.14% of cases, 5 mm;
In transversal plane: the molar premolar and canine reference point the corresponding maxillary odonto-periodontal units must circumscribe the mandibular ones with one cusp, 33.33% of cases normality and in 16.67% of cases, reverse oclusion; the incisal reference point the maxillary and mandibular interincisal lines must be one after the other 33.33% of cases lateral deviation, right or left (28.57% of cases);
In vertical direction:
The molar, premolar ,canine reference points we must verify if between the occlusal surfaces of the 6 year molars the premolars respectively the palatine surfaces of the canines there are contacts with the antagonists and if they are align at the level of the occlusion planes and curves: infraocclusion (11.90% of cases) and supraoclussion (11.90% of cases).
The incisal reference joint the mandibular incisor are covered by the maxillary ones in proportion that varies from 0-1/3 from the height of the vestibular surfaces parameter a coverage larger than 1/3 suppraocclusion its values reaching to 1/1. Negative values open occlusion the dynamic occlusion. We find normality of 21 patients, 16.67% of cases more than 1/3 of the vestibular face of inferior incisors. We have also the total over of inferior incisor - overbite 1/1 to 4.76% of cases.
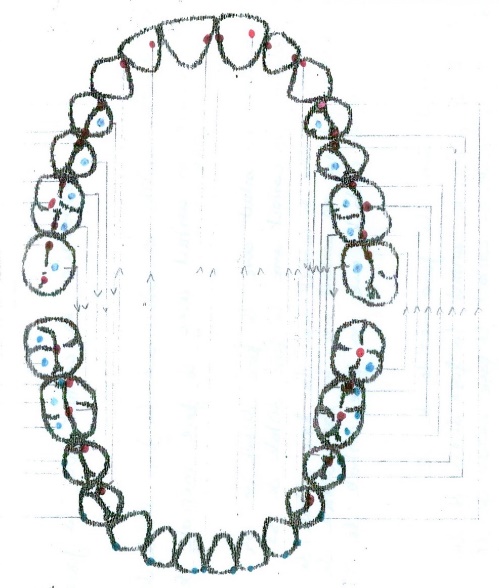
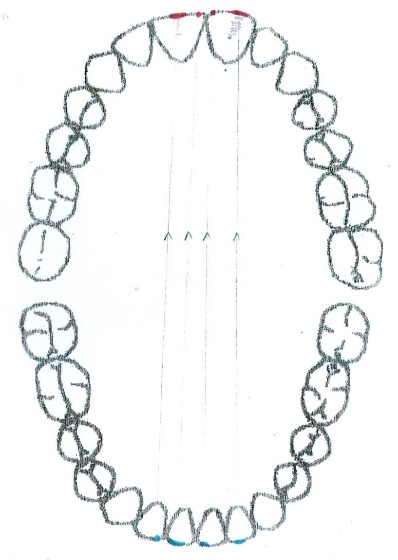
After this, every patient must have the graphic reprezention of personal occlusograme (figure
04 ), (the typology of contacts in intercuspidal relation point centric) (2.38% of cases) in centric relation long centric (figure05 ) (97.62 of cases) and the occlusogram in dynamic relation: protrusion (figure06 ) and laterality right (figure07 ) and left (figure08 ).
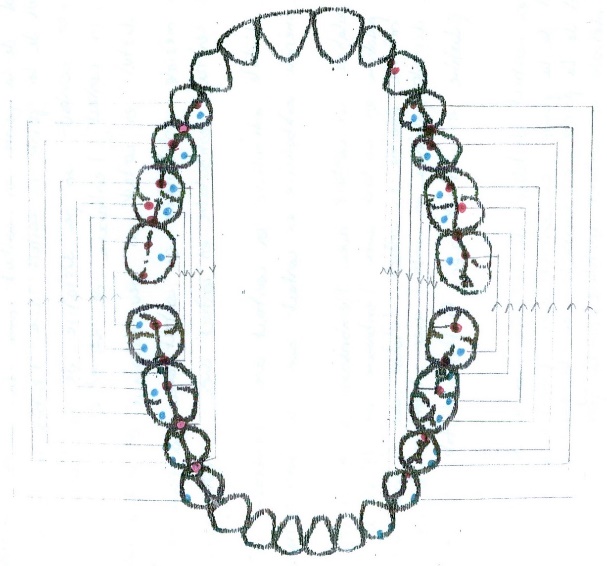
The dynamic occlusion represents the sum of the interarch contacts at the moment when the mandibular movements (with dental contact) are performed. The static occlusal relation is strongly correlated with the dynamic ones. The movements that can be performed in dynamic occlusion are propulsion protrusion laterality and retropulsion. Protrusion with a dental contact having as a support the anterior guidance on the active art we examine the test movement and the test position: the movement shapes ric rac (14.29% of cases), letters c (9.52% of cases), bayonet (35.71% of cases) it may be move to the left (14.29% of cases) or to the right (16.67% of cases); the test position represents the incisal edge on incisal ridge aspect, it should contact 4 maxillary front teeth with 4 mandibular four teeth (19.05% of cases), only 3 (30.95% of cases), 19.05% of cases 2 contacts and 1 contact (28.57% of cases).[8-12 ]
The laterality movement is concerned we examined the right and the left laterality. We will examine the active part and the inactive part and the test movement must be continuous slightly (50.00% of cases), left laterality (42.86% of cases), right laterality descending towards the lateral side. Pathological it may be interrupted modified as (45.24% of cases) left, (40.48% of cases) right shape or even impossible to perform in the case of inverted interlocking on the active side (4.76% of cases) left, right (16.67% of cases). The test position only the edges of the canines come in contact the patients presents canine conduction (40.48% of cases left, 35.71% of cases right) respectively the vestibular cuspidal edges may contact- the canine and /the molar one situation, named group conduction on the inactive part, there must exist any contact if there are any contacts they are pathological occlusal interferences for the rest of the cases. For this kind of problem we must act like the gnatologyst must action with the selective occlusal grinding (21.43% of cases) with different methods, Barelle, Dowson, Yankelson etc. till the patients have the right functionality and can execute the movement. Also, the muscle need to have the relaxant medication (42.86% of cases) accompanied by the application of relaxating trays (Felicio et al., 1991) and can also be used as adjuvant balneofiziochinetoterapic treatment like: ozonoterapy (28.57% of cases), masoterapy (11.90% of cases) and kinetoterapy (42.86% of cases). (Checherita, Forna, Stamatin, Cobzaru, Leon & Cioloca, 2013), (Checherita, Beldiman, Stamatin, Foia & Forna, 2013). The purpose of a therapy of fully or partially edentulous patients with removable or fixed dentures is to restore their chewing function, speaking ability, and to improve their facial appearance and overall quality of life. (Sarlani, Balciunas & Grace, 2005). Adequate chewing function should enhance both, general health and quality of life . Chewing difficulties are more commonly found in elderly population due to physiological ageing, which may be related to teeth wear and/or to a loss of periodontal tissues, increased mobility of residual teeth and/or teeth loss as well as decrease of residual alveolar bone. Even individuals with natural teeth may have problems with chewing of certain food due to restorations, tooth wear, oral mucosa diseases or temporomandibular disorders (Rener-Sitar et. al., 2008). Patients have been applied, simultaneously, different fixed prosthetic treatments, mobile, as well as relaxation mouth guards, an improvement of the quality of life of these patients being registered, as it follows: in 80.95% of cases were applied acrylic prostheses and in the rest, both fixed and mobile, only in 9.52% of cases being used the method of relaxation mouth guards, in the Clinical Base of “Mihail Kogalniceanu“, Iasi (Checherita et. al., 2016) (Forna, 2011).
Conclusion
The pathology of stomatognatic system is complex and general malady can created a great difficulty to approach the treatment of this and also the economic resources can indicated a difficulty to create the optimal functionality of it. From this point of view we can say about our investigated cases that the morphology is altered witch is indicated by the examination and results obtain of parameters of occlusion and the Angle key also this is indicated by the delay or absence of intervention with the specific treatment for different type of reasons, and the mandibulo-cranian relation are not favourable and also the articulation system is not in the right parameters indicated by paraclinic examination tomography TMJ, also the stress and the depression the anxiety, the absence of contacts can create a difference of the tonicity of the muscle, and also an impossibility to create a good dynamic occlusion. The treatment is interfered by a lot of difficulties in respecting and follow the indication and our prescription, but in the final we succeed to obtain in 88.09% of cases a good functionality.
References
- Checherita, L. E., Beldiman, M. A, Stamatin, O., Foia, L., Forna, N. C. (2013). Aspects on Structure of Materials Used for Different Types of Occlusal Splints. Revista de Chimie (Bucharest), 64(8), 864-867.
- Checherita, L. E., Forna, N. C., Stamatin, O., Cobzaru, R., Leon, M.M., Cioloca, D. (2013). Correlations between Biochemical Parameters Integrated in Stomatognathic System Dysfunctional Syndrome. Revista de chimie,(Bucharest), 64(10), 1172-1181.
- Checherita, L. E., Trandafir, D., Stamatin, O., Carausu, E. M. (2016). Study of Biochemical Levels in Serum and Saliva of Zinc and Copper in Patients With Stomatognathic System Dysfunctional Syndrome Following Bone Injury and prosthetical treatment. Revista de Chimie (Bucharest), 67, 8, 1628-1633.
- Felicio, C. M., Rodrigues da Silva, M. A., Mazzetto, M. O., Centola, A. L. (1991). Myofunctional therapy combined with occlusal splint in treatment of temporomandibular joint dysfunction-pain syndrome. Braz Dent J. 2(1), 27-33.
- Forna, N. C. (2011). Protetica Dentara, vol I ,II. Romania: Iasi.
- Janal, M. N., Raphael, K. G., Nayak, S., Klausner, J. (2008). Prevalence of myofascial temporomandibular disorder in US community women. J Oral Rehabil, 35(11), 801-809.
- Miettinen, O., Lahti, S., Sipilä, K. (2012). Psychosocial aspects of temporomandibular disorders and oral health-related quality-of-life. Acta Odontol Scand, 70(4), 331-336.
- Nekora-Azak, A. (2004). Temporomandibular disorders in relation to female reproductive hormones: a literature review. J Prosthet Dent, 91(5), 491-493.
- Okeson, J. P. (2008). Management of temporomandibular disorders and occlusion. St Louis, MO: Mosby.
- Rener-Sitar, K., Celebic, A., Stipetic, J., Marion, L., Petricevic, N., Zaletel-Kragelj, L. (2008). Oral Health Related Quality of Life in Slovenian patients with craniomandibular disorders. Coll Antropol, 2, 513–517.
- Sarlani, E., Balciunas, B. A., Grace, E. G. (2005). Orofacial Pain – Part II: Assessment and management of vascular, neurovascular, idiopathic, secondary, and psychogenic causes. AACN Clin Issues, 16(3), 347-58.
- Sunil, W., Sunil, K. (2008). TMJ Disorders: Future Innovations in Diagnostics and Therapeutics. Journal of Dental Education, 1(8), 930-947.
- Warren, M. P., & Fried, J. L. (2001). Temporomandibular disorders and hormones in women. Cells Tissues Organs, 169(3), 187-192.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
30 July 2017
Article Doi
eBook ISBN
978-1-80296-026-6
Publisher
Future Academy
Volume
27
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-893
Subjects
Teacher training, teaching, teaching skills, teaching techniques,moral purpose of education, social purpose of education, counselling psychology
Cite this article as:
Checheriță, L., Stamatin, O., & Costan, V. (2017). The Treatment Of Social Cases For Tmj Disorders. In A. Sandu, T. Ciulei, & A. Frunza (Eds.), Multidimensional Education and Professional Development: Ethical Values, vol 27. European Proceedings of Social and Behavioural Sciences (pp. 731-743). Future Academy. https://doi.org/10.15405/epsbs.2017.07.03.87

