Abstract
Starting with 1983, when the DRG payment system was introduced in the United States as a control system of healthcare costs, the medical community expressed concern related to the impact this will have on the quality of medical assistance. Nevertheless, it is remarkable that a convergence was created between a payment pattern for hospitals and the efficient execution of medical services, by introducing the DRG payment system. Thus, through the DRG payment system, patients can be classified simultaneously based on their illness and based on the care costs, which ensures the possibility of associating types of patients with realised healthcare expenses. Implementing the DRG in Romania has started between 1999 – 2001, having as objectives the calculation of cost per patient, based on electronic records of patient data and grouping these in DRG, changing the financing method of hospitals, in view of increasing the quality and efficiency of care given to hospitalized patients. The DRG was developed in Romania based on defined strategies for different time periods, for a number of 409 hospitals, by elaborating the necessary legislative frame, developing a collection app for clinical data, encoding diagnoses based on International classification of Illness, classifying discharged patients into diagnoses groups (DRG), collecting and electronic reporting of clinical data, calculating necessary tariffs on patient levels / DRG, assessing clinical activity of hospitals based on discharged patient data.
Keywords: health economicspayment systemsdiagnosis-related groups (DRGs)healthcare spending;
Introduction
Promoting and protecting health is essential to human welfare and sustained economic and social development. This was recognized more than 30 years ago by the Alma-Ata Declaration signatories, who noted that health for all would contribute both to a better quality of life and also to global peace and security (World Health Organization, 2010, p. 9).
An important aspect belonging to the development of healthcare systems is the efficient use of all resources, together with concentrating these resources towards improving and developing healthcare systems. The substantial growth in efficiency can be realized by reforming payment mechanisms in hospitals, especially due to the fact that expenses for hospital services have the largest shares out of the total expenses of healthcare in all countries, irrespective of their income levels.
Payment systems based on diagnosis-related groups (DRGs) are one type of such hospital payment mechanisms, along with capitation payments, global budgets and a combination thereof. Today, DRGs are used primarily by purchasers to reimburse providers for acute inpatient care, but in principle they can also be used to reimburse them for non-acute inpatient care (Mathauer & Wittenbecher, 2013, p. 1).
The DRG model has been created and developed in the late 1960s, at Yale University, by a group of doctors, economists and statisticians, that attempted to envision an assessment system for hospital results and had as initial motivation the creation of an efficient monitoring frame of healthcare quality and the degree of using hospital services. Therefore, DRGs must be considered, first and foremost, a financing system, and not only a classification system. The first large scale use of the DRG was done at the end of the 1970s in New Jersey when The State Department of Health used DRGs as the basis of a prospective payment system in which hospitals were reimbursed a fixed DRG specific amount for each patient they treated. In 1982, the Tax Equity and Fiscal Responsibility Act modified section 223 on Medicare hospital reimbursement limits to include a case mix adjustment based on DRGs. In 1983, the Congress amended the Social Security Act to include a national DRG-based hospital prospective payment system for all Medicare patients (Clinical Research and Documentation Departments of 3M Health Information Systems, 2003, p. 3).]
Problem Statement
The current evolution of the DRG model and its use as cornerstone payment system represents recognition of the fundamental role that a hospital’s case mix plays in determining its costs. The development of the DRGs provided the first operational means of defining and measuring a hospital’s case mix complexity.
The concept of case mix complexity initially appears very simple, but users of the system have often attached different meanings to the concept of case mix complexity depending on their backgrounds and purposes. The term case mix complexity has been used to refer to an interrelated but distinct set of patient attributes which include severity of illness, risk of dying, prognosis, treatment difficulty, need for intervention, and resource intensity.
Research Questions
The research aims to measure the efficiency in the implementation of the DRG for financing hospitals in Romania, by increasing the responsibility and autonomy of hospital management, generating profit, avoiding financial losses, improving the quality of healthcare services.
How can we define DRGs?
DRGs can be defined as a manageable number of categories based on diagnosis that are clinically differentiated, as well as resource wise, give the possibility of correlating case types that the hospital is treating (case–mix index) and afferent costs (www.drg.ro/DocDRG/download.php?fi=15). DRG classifies cases based on the following patient variables: primary and secondary diagnoses, patient age and sex, existing comorbidity and complications, as well as the procedures the patient underwent. These make possible the measuring of hospital results and provide a data base for funds, budget and other obligations. Moreover, DRGs can be used for the development policy related to access and equity, analysis of clinical and encoding practice and market and medication requisition, as well as prostheses, mobile chairs, etc.
What are the main characteristics of diagnoses groups?
Diagnoses groups have two main characteristics: (1) clinical homogeneousness, meaning that in a certain DRG, cases (patients) are similar (but not identical) from a clinical point of view and (2) price homogeneousness, meaning that each DRG contains cases needing a similar resource consumption.
Diagnoses group are medical and surgical according to the presence or absence of a surgical intervention and are conceived to cover the pathology associated to patients with acute illnesses that need hospitalization. These are conceived in the light of standardizing hospital results (expressed through the number of released patients, homogenised inside these groups (Haraga & Radu, 2006, p. 91).
Purpose of the Study
The Romanian healthcare system valid until 1989, was inspired in the 1940s by the Soviet model (Semasko). This was state funded, centralized and was based on prevention, planning, gratuity, wide accessibility to healthcare, the scientific character of the healthcare policy and self-conscious participation of the population in safeguarding the or own health. Essentially, healthcare system was and is a state organized and funded system that is comprised of a network of state healthcare units, managed through a centralized structure. Financing is done via contributions, taxes from the state budget and doctors are employees of the state.
As it became obvious in the prior period from the financing, organization and functioning perspective, the healthcare system, despite its deficiencies, has also had a series of advantages, due to the fact that the system was developed on equity principles, thus ensuring the access to healthcare almost to the entire population. The access to healthcare was not influenced by the patient’s capacity to pay. System financing and organization allowed a thorough cost control. Expense share for health from GDP was relatively low, these limitations have generated the lack or access limitation to certain services, especially to those that imply high costs for equipment or materials (dialysis, cardiovascular surgical procedures, transplant, prosthetics, CAT scans, etc.), healthcare system functioning being done with reduced administrative costs.
After 1990, as a result of the free market economy, together with the development requirements of a democratic society, the healthcare system characteristics have become inconsistent with the specific health needs of the new state, it became increasingly important that health be understood as ‘a business of the entire society’, that targets its embedment as a target into the economic and social development plans. Healthcare underfinancing has determined considerable delays in introducing new technologies necessary to current diagnosis or treatment of pathology, subsequently generating severe deficiencies in ensuring medication and current use healthcare materials. This discouraged the preoccupation of healthcare services in the insurance and assessment of healthcare quality, an essential element of system performance.
The first attempt in this respect was done in 1997, when Romania introduced a new healthcare insurance system by way of law no. 145/1997, based on a modified version of the Bismarck model, a social insurance healthcare system (based on mandatory, income dependant insurance bonuses).
Implementing the DRG system in Romania has started between 1999 and 2001, with the debut of the "
Implementing the DRG in Romania was based on well-defined strategies for different periods of time, as well as on specific action plans developed by the Health Ministry, in conformity with the national strategies related to the healthcare reform. The experience accumulated during this first project has allowed the initiation of the ‘DRG National Project’, based on the provisions of the collaboration agreement dated June 1st, 2000, between the Health Ministry, the National Healthcare Insurance House, the Romanian Board of Doctors, the Ministry of Finance and the Health and Human Services Department of USA, as well as the Order of the Health Ministry no. 935/2000, related to the approval of first stage implementation of the financing project for case based hospitals, completed by the Order of the Health Ministry no. 137/2001.
Subsequently, as a follow up for the start of the DRG National Project, the mechanisms necessary for the case based financing were applied, in the beginning in 23 pilot states, meaning in 409 hospitals, currently: elaborating the legislative frame, developing a clinical data collection app, encoding diagnoses based on the Illness International Classification, classifying discharged patients per diagnoses groups, electronically collecting and reporting clinical data, calculating necessary tariffs for hospital financing per patient level / DRG, evaluating the quality of clinical activity of hospitals based on data related to discharged patients.
Research Methods
In field literature, the DRG payment system is attributed with different approaches, being influenced by a series of factors. Each DRG is associated with a specific cost weight or tariff, which is usually calculated from the information about average treatment costs of patients falling within a specific DRG, in at least a sample of other hospitals in the past (Olteanu, Szora, & Dobra, 2014, p. 71). Irrespective of the chosen approach, hospitals under DRG-based hospital payment systems who either receive a DRG-based case payment or a DRG-based budget allocation, are exposed to the financial risk of having costs above the payment rate and are rewarded for keeping costs below (Scheller-Kreinsen, Quentin & Busse, 2011, p. 1166).
The study was based on archived data from the website of the Center for Research and Assessment for Health Services, a structure within the National School of Public Health, Management and Continuous Education in Health Bucharest, and the collected data from the Orders of the Ministry of Health and of the President of the National Health Insurance House, between 2013 – 2016 (The Orders of the Ministry: no. 763/377 of 2016, pp. 241 – 264; no. 388/186 of 2015, pp. 260 – 272; no. 619/360 of 2014, pp. 218 – 247; no. 423/191 of 2013, pp. 191 - 216), for the approval of the methodological norms for implementing the Framework Agreement regarding the conditions of granting medical assistance within the social health insurance system for 2013, 2014, 2015 si 2016, in Romania. Starting with 2003, the National School of Public Health, Management and Continuous Education in Health, Bucharest is the main institution responsible for the national coordination of all patients that had access to Romanian hospitals, irrespective of their type of financing.
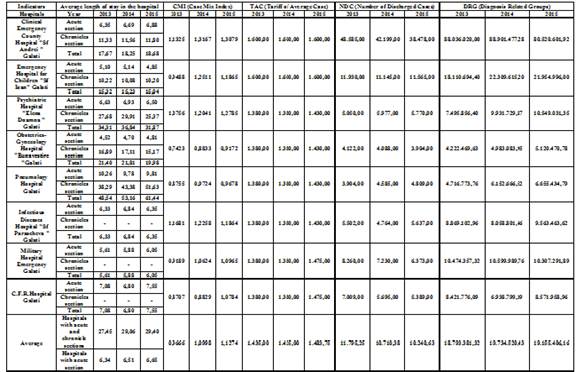
Within the herewith study, we made a qualitative analysis of hospital activity over a period of three years (2013 – 2015), on a sample of 8 Galati based hospitals, financed through the DRG payment system.
Within the framework of the qualitative analysis through data, rule and regulation collection process related to the reimbursement of expenses for hospital healthcare, we looked for the impact of the following indicators over the evolution of financing of the presented hospitals, as well as over the level of healthcare service quality given to patients: average length of stay in the hospital, Case Mix Index (CMI), Tariff of Average Case (TAC), Number of Discharged Cases (NDC), Diagnosis Related Groups (DRGs) – Table no.1.
In order to calculate the value of the DRGs realized in the 8 hospitals between 2013 – 2015, we used the below presented formula based on specialty indicators:
DRGij = NDCij x CMIij x TACij
where:
i – year;
j – hospital;
NDC - Number of Discharged Cases, realized by each hospital, based on number of beds;
CMI - Case Mix Index, realized by each hospital based on the complexity of the medical activity and correctness of medical cases’ encoding;
TAC - Tariff of Average Case, observant of the competence based hospital classification.
Findings
As a result of the calculations that were made, based on the evolution of the indicators presented beforehand, the following results were obtained, presented in different situations for each hospital:
a) A hospital that registered a growth in the level of the DRG amount during the analysed period, in 2014 as compared with 2013, and a drop in 2015 compared to 2014 and 2013. The amounts were realized in the following conditions: has had the same TAC (Tariff of Average Case) over the entire period, realized CMI (Case Mix Index) has grown in 2014 compared to 2013 and has started to drop in 2015 compared with 2014,
Number of Discharged Cases (NDC) has dropped in 2014 and 2015 compared, with positive effects over the improvement of healthcare services quality as a result of the increase in financing allocated to each patient, for the amount allocated through TAC (Tariff of Average Case), for the entire period, nationwide;
b) A hospital that registered a growth in the level of the DRG amount during the analysed period, in 2014 compared to 2013 and a drop in 2015 compared to 2014. The amounts were realized in the following conditions: has had the same TAC (Tariff of Average Case) over the entire period, realized CMI (Case Mix Index) has grown in 2014 compared to 2013 and has started to drop in 2015 compared with 2014, Number of Discharged Cases (NDC) has dropped in 2014 compared in 2013 and has grown in 2015 compared to 2014, with positive effects over the improvement of healthcare services quality as a result of the increase in financing allocated to each patient, for the amount allocated through TAC (Tariff of Average Case), for the entire period, nationwide;
c) A hospital that registered a growth in the level of the DRG amount during the analysed period, in 2014 compared to 2013, as well as in 2015 compared with 2014 and 2013, the amounts were realized in the following conditions: has had the same TAC (Tariff of Average Case) in 2013 and 2014, and has grown in 2015, compared to previous years, the realized CMI (Case Mix Index) has grown in 2014, compared to 2013, as well as in 2015 compared with 2014 and 2013, the Number of Discharged Cases (NDC) has grown in 2014, compared with 2013, has also grown in 2015 compared with 2013 but less than in 2014, with positive effects over the improvement of healthcare services quality and increase in hospital financing, as a result of the increase in financing allocated per patient during the period of three years, over the amount allocated through TAC (Tariff of Average Case), nationwide;
d) A hospital that registered a growth in the level of the DRG amount during the analysed period, in 2014 compared to 2013, as well as in 2015 compared with 2014 and 2013, the amounts were realized in the following conditions: has had the same TAC (Tariff of Average Case) in 2013 and 2014, that has grown in 2015, the realized CMI (Case Mix Index) has grown in 2014 compared to 2013, as well as in 2015 compared to 2013 and 2014, Number of Discharged Cases (NDC) has dropped in 2014 and 2015 , compared to 2013, with positive effects over the improvement of healthcare services quality and increase in hospital financing, as a result of the increase in financing allocated per patient during the period of three years, under the amount allocated through TAC (Tariff of Average Case), nationwide, due to ‘less than one unit’ values of the CMI realized by the hospital in the entire three-year period;
e) A hospital that registered a growth in the level of the DRG amount during the analysed period, in 2014 compared to 2013, as well as in 2015 compared with 2014 and 2013 the amounts were realized in the following conditions: has had the same TAC (Tariff of Average Case) in 2013 and 2014, that has grown in 2015 compared to previous years, the realized CMI (Case Mix Index) has grown in 2014 compared to 2013, as well as in 2015 compared to 2013 and 2014, Number of Discharged Cases (NDC) has grown in 2014, compared to 2013, as well as in 2015 compared to 2013 and 2014, with positive effects over the improvement of healthcare services quality and increase in hospital financing, as a result of the increase in financing allocated per patient during the period of three years, under the amount allocated through TAC (Tariff of Average Case), nationwide, due to ‘less than one unit’ values of the CMI realized by the hospital in the entire three-year period;
f) A hospital that registered a decrease in the level of the DRG amount during the analysed period, in 2014 compared to 2013, due to the decrease of patients, and a growth in 2015 compared with 2013 and 2014. The amounts were realized in the following conditions: has had the same TAC (Tariff of Average Case) in 2013 and 2014, that has grown in 2015 compared to previous years, the realized CMI (Case Mix Index) has grown in 2014 and 2015 compared to 2013, Number of Discharged Cases (NDC) has decreased in 2014, compared to 2013, and has grown in 2015 compared to 2014 and 2013, with positive effects over the increase of hospital financing.
The financing allocated per patient during the period of three years was over the amount allocated through TAC (Tariff of Average Case), nationwide.
g) A hospital that registered a growth in the level of the DRG amount during the analysed period, in 2014 compared to 2013, and a drop in 2015 compared to 2014 and 2013. The amounts were realized in the following conditions: has had the same TAC (Tariff of Average Case) in 2013 and 2014, that has grown in 2015 compared to previous years, the realized CMI (Case Mix Index) has grown in 2014 compared to 2013, as well as in 2015 compared to 2014 and 2013, Number of Discharged Cases (NDC) has decreased in stages in 2014, compared to 2013, as well as in 2015 compared with 2013 and 2014, with positive effects over the improvement of healthcare services quality and increase in hospital financing as a result of the increase in financing allocated per patient during the period of three years, over the amount allocated through TAC (Tariff of Average Case), nationwide, only in 2014 and 2015.
h) A hospital that registered a decrease in the level of the DRG amount during the analysed period, in 2014 compared to 2013, and a growth in 2015 compared with 2013 and 2014. The amounts were realized in the following conditions: has had the same TAC (Tariff of Average Case) in 2013 and 2014, that has grown in 2015 compared to previous years, the realized CMI (Case Mix Index) has grown in 2014 compared to 2013, as well as in 2015 compared to 2014 and 2013, the Number of Discharged Cases (NDC) has decreased in 2014 in stages, compared to 2013, as well as in 2015 compared to 2013 and 2014, with positive effects over the improvement of healthcare services quality and increase in hospital financing as a result of the increase in financing allocated per patient during the period of three years, over the amount allocated through TAC (Tariff of Average Case), nationwide, only in 2015.
From the results obtained, we can draw the conclusion that all hospitals aim at increasing their incomes and improving their healthcare services, the main indicator with major effects being CMI (Case Mix Index). As a result of its dynamic value, hospitals can realize the incomes necessary for their functioning with less expenses, due to the drop of Number of Discharged Cases (NDC) and, therefore, increasing the quality of the medical act by additional sum allocation towards patient care.
The analysed hospitals, under DRG-based hospital payment systems, receive a DRG-based case payment and are allocated a limited budget imposed by the above shown formula. Thus, hospitals are exposed to the financial risk of having costs above the payment rate and are rewarded for keeping costs below. For these hospitals, implementing the DRG has helped their management by improving the quality of economic and financial indicators, cutting losses, increasing incomes, adapting medical indicators to current economic and financial conditions, by efficient use of strategic, financial planning, cutting large variations in medical performance and economic results. Patient dissatisfaction level was reduced, related to the services they received and waiting time. The quality of healthcare has increased and has become a priority for healthcare suppliers, hospital managers, patients, third party payers, but also governmental organizations / institutions.
Conclusion
Financially speaking, by dropping out the previous healthcare system, the current system has advocated two important principles of a very suitable healthcare policy, meaning: equity and sustainability of healthcare financing.
In view of abiding by the above stated principles within medical units with beds, the Health Ministry has started the flattening of tariffs per average case, the purpose being equal payment for all units to similar medical cases. This TAC flattening was possible together with the implementation of the previsions of the 2010 Frame Agreement, by comparing the TAC of every hospital with the national TAC and making use of the risk interval principle that was used in the previous years.
This first step towards an equitable base financing has continued in future frame agreements, meaning that if in 2010, the proportion between minimal and maximal TAC was 77, 76%, in 2016 we have a difference of 55,94%. Also, in order to diminish inequitable financing sources, a financing strategy was developed for healthcare of chronic type, as well as a rethinking of financing for healthcare services that need day hospitalization.
Using the DRG financing system of hospitals aims at distributing similar patients in homogenous diagnoses groups, based on clinical illness and used resources during the treatment period, expressed through the relative group value. The payment of the service performed by the hospital is done by multiplying the relative value with TAC that is a medial cost, calculated beforehand for all diagnoses groups. Thus, the hospital is motivated to come under TAC, as low as possible, controlling at the same time the increase of the CMI.
Due to the fact that there are no national relative values based on real relative costs, values that have been taken over and partially correlated are used. These are more specific to the Australian healthcare system and not to the Romanian system. One of the explanations for inequitable financing between different specialties and hospitals, and for the increase of clinical hospitals debts through the years is due to borrowed relative values, as well as to the tariff paid by CNAS that does not cover medial hospital costs, especially for complicated cases, with long hospital stays. The mechanisms afore mentioned encourage hospitals to grow the number of hospitalizations (formally or fictitiously) for simpler cases
As it was introduced in many high income countries, the DRG payment system was meant to reduce costs, in Romania as well, to increase efficiency of patient care inside hospitals or to improve the transparency of medical activities. Being a progressive financing, the introduction of DRG based financing healthcare in Romania has changed the vision of hospital management. From the introduction of financing these services based on diagnoses groups, when TAC was originally calculated based on historical financing, flattening was tried every year, as well as bringing paid tariffs closer to real costs. The development and implementation of DRG based payment systems in Romania has brought about the introduction of a set of quality indicators that, correlated with financial incentives for reaching them in hospital care, has optimized the level of hospitals services, the efficiency and quality, by reducing patient costs.
This situation was realized as a result of a drop in hospitalization days, avoiding to offer healthcare services that are not necessary, treating patients based on hospital competency, introducing illness encoding practices, improving diagnosis and procedure encoding, eliminating and diminishing fraud.
Together with these advantages created by the current payment system, a series of disadvantages was created: early patient discharge in need of medical care, refusal / not granting healthcare to patients, fraudulent reclassification of patients by adding secondary diagnoses to increase the value of CMI and also the financial value received by the hospital for the patient, reporting medical services that were not granted to patients.
References
- Clinical Research and Documentation Departments of 3M Health Information Systems (2003). All patient refined Diagnosis Related Groups (APR-DRGs), Version 20.0. Methodology Overview. Wallingford, Connecticut and Murray, Utah, USA. Retrieved from http://docplayer.net/71458-All-patient-refined-diagnosis-related-groups-apr-drgs-methodology-overview.html .
- Haraga, S. & Radu, P. (2006). Hospital Management, National School of Public Health and Health Management, Chapter III - System DRGs (DRGs). Bucharest: Public H Press.
- World Health Organization, (2010). The world health report: health systems financing: the path to universal coverage. Retrieved from http://www.who.int/whr/2010/en/.
- Mathauer, I. & Wittenbecher, F. (2013). Hospital payment systems based on diagnosis-related groups: experiences in low - and middle-income countries. Bulletin of the World Health Organization, 91, 746-756A. doi: DOI: 10.2471/BLT.12.115931 .
- Olteanu, E., Szora, A.T. & Dobra I. B. (2014). The effect of financing hospital health care providers through updated Diagnosis Related Groups. Case studies: the municipal hospitals in Romania. Finance – Challenges of the Future, no. 16, 70-81 .
- Scheller-Kreinsen D., Quentin W., Busse R., (2011). DRG-Based Hospital Payment Systems and Technological Innovation in 12 European Countries. Value in Health, 14(8), 1166-1172. doi: DOI: 10.1016/j.jval.2011.07.001 .
- Manual definitions. (2011). Volume 1 - Diagnosis related groups - DRG classification EN v.1, p. 2, Retrieved from www.drg.ro/DocDRG/download.php?fi=15 .
- The Order of the Ministry of Health and of the President of the National Health Insurance House no. 763/377 of 2016, for the approval of the Methodological Norms for implementing the Framework Agreement regarding conditions for granting medical assistance within the social health insurance system for the years 2016, pp. 241 – 264. Retrieved from http://www.cnas.ro/casgl/post/type/local/ordin-nr-377-763-2016.html .
- The Order of the Ministry of Health and of the President of the National Health Insurance House no. 388/186 of 2015, for the approval of the Methodological Norms for implementing the Framework Agreement regarding conditions for granting medical assistance within the social health insurance system for the years 2015, pp. 260 – 272. Retrieved from http://www.cnas.ro/national-page/ordinul-388-186-2015-pentru-aprobarea.html .
- The Order of the Ministry of Health and of the President of the National Health Insurance House no. 619/360 of 2014, for the approval of the Methodological Norms for implementing the Framework Agreement regarding conditions for granting medical assistance within the social health insurance system for the years 2014, pp. 218 – 247. Retrieved from http://www.cnas.ro/national-page/ordin-619-360.html .
- The Order of the Ministry of Health and of the President of the National Health Insurance House no. 423/191 of 2013, for the approval of the Methodological Norms for implementing the Framework Agreement regarding conditions for granting medical assistance within the social health insurance system for the years 2013, pp. 191 – 216. Retrieved from http://www.casan.ro/national-page/ordin-nr-423-191.html .
- www.drg.ro.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
30 July 2017
Article Doi
eBook ISBN
978-1-80296-026-6
Publisher
Future Academy
Volume
27
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-893
Subjects
Teacher training, teaching, teaching skills, teaching techniques,moral purpose of education, social purpose of education, counselling psychology
Cite this article as:
Antohi, V. M. (2017). Romanian Healthcare Financing Based On The Diagnosis - Related Group Payment System (Drg). In A. Sandu, T. Ciulei, & A. Frunza (Eds.), Multidimensional Education and Professional Development: Ethical Values, vol 27. European Proceedings of Social and Behavioural Sciences (pp. 19-28). Future Academy. https://doi.org/10.15405/epsbs.2017.07.03.4

