Abstract
The increased recognition of the qualitative methodology in the health field is a way of enhancement and highlights topics that would remain hidden if the option was the quantitative research. The purpose of this systematic review paper is to reflect about the importance of the qualitative methodology in the study of community health with the elderly. It seeks to identify areas of existing research, describe findings and analyse implications emerged for socio-educational intervention to inform practice and further research. The relevant literature was identified through two electronic databases: MEDLINE and PubMed (2010-2015). Inclusion criteria were: published qualitative or mixed-method studies, about elders, in community health. Relevant data including findings and practice recommendations were extracted and compared in tabular format and were included 48 articles of the 226 initially identified. The majority (20) came from Europe and 11 from North America, but we found studies in all Continents. Study repliers included health professionals, informal carers, patients, community members and relatives. Most (13) were focused on health care network, six on end-of-life care and six on quality of life and successful aging. The others referred to multiples themes. Qualitative research in elderly community health can help researchers to gain a more complete understanding or interpret the results of quantitative data more completely, as well as show us local specificities, that support a differentiated socio-educational intervention.
Keywords: Qualitative researchelderlycommunity healthsocio-educational intervention
Introduction
Quantitative research come from the positivist paradigm, dominated studies in the scientific
community for decades and says that research must use the methods and procedures of the physical-
natural sciences, such as physics, chemistry, biology and others, including the medical sciences. With the
development of the social and human sciences, research has assumed that the nature of the social world is
not the same as that of the natural world, often finding multiple realities considering the meanings that
individuals attribute to phenomena. Hence, a second paradigm of a constructivist nature has emerged in
the scientific community, specifically from the 60's of last century (Coutinho, 2011). Paulilo (1999, cit. in
Araújo, Martins, Fernandes, Mendes, & Magalhães, 2016) discusses that this phenomenological research
permits deeping facts and specific processes of individuals, including values, attitudes and
representations. In fact, the intention is to obtain an in-depth knowledge of people's life experiences
through their representations of it and not of events per se or by measuring behaviors and quantitatively
correlating them, as defended in the positivist paradigm also called empirical-analytic (Bogdan & Biklen,
1998).
Qualitative and quantitative research are complementary and the choice of one or another way of
investigating will always depend on the questions that are the basis of the researcher's study. Despite their
relevance in different areas, including in medicine and health in general, as we will see below, papers
using the qualitative methodology were for a long time scarce and even considered of less value and non-
scientific (Britten, 2005). In the past, if the researcher wanted, by instance, to explain the phenomenon of
drug abuse the study might be carried out by psychiatrists, epidemiologists or researchers in the field of
clinical pharmacology, whereas if the aim was to understand their implications for the patient's life, the
study would be easily attributed to "qualitative researchers" in the field of psychology, sociology or
education (Turato, 2005). However, according to the author, it is essential that health professionals also
become interested in qualitative methods, since they have the advantage of linking a clinical attitude (as
result of their practice) with an existential one, which will allow to bring important contributions for the
advancement of scientific knowledge.
Nevertheless, the methodological option for qualitative research has been only recently (especially
in the last decade) valued in several areas, including in health. Nowadays, health professionals have been
choosing for a scientific model, complementary to the positivist, helping them to understand the human
being in his relationship with the environment, namely the way he/she lives in society (Santos, Azevedo,
Costa, & Medeiros, 2011). In fact, taking care of health, besides knowledge and technique, also integrates
emotion and creativity and has a relational, existential and contextual nature (Barbosa, Motta, & Resck,
2015). Using the qualitative methodology in the health area allows us to understand the feelings, ideas
and behaviors of the patients and their families, as well as of the health professionals themselves,
improving the quality of the professional-patient relationship and the treatment and preventive measures
compliance (Turato, 2005).
Public health, as a fundamentally interventional area, is an organized and concerted effort in the
conditions of life that create, maintain and protect the health of individuals. Community health represents
an evolution of this concept, by the emphasis placed on responsibility and community participation in this
process. The attention given to community health emerges from the development of science in medicine
and its care of the population. In this context, the present paper will be focus on health support to a
rapidly growing age group in the most developed countries: the elderly. Data from the World Health
Organization (WHO), in 2011, show that the process of population aging, which is intended to be active,
is occurring on a planetary scale and is associated with a decrease in mortality and an increase in life
expectancy both resulting from improvements in medical care and living conditions, at home and in
permanent and partial elderly support services. Understanding living conditions and health care needs of
elderly people is becoming increasingly need considering the demographic data above.
According to WHO (2011), currently the non-communicable diseases, such as heart problems,
cancer and diabetes, affect most of the elderly people, reflect changes in lifestyle and diet. Hence, WHO
(2011) recommend that it is fundamental to guarantee appropriate care and to implement preventive
measures to live longer, with quality, letting the elderly people to remain active and autonomous, which
will reduce health costs for the family and society. However, this international organization underlinethat
families and societies have been decreasing their support to the elderlypopulation, requiring an
investment in the collection of data and intervention tools to ensure the well-being of this group that has
been living more and more alone.
In this sense, to understand how to support this population can start from studies of a qualitative
nature that gives information to complement the results that we already have stemming from the
quantitative studies that have dominated the panorama of research for centuries. By understanding local
and individual specificities, will be possible to design well-founded socio-educational intervention
guidelines, that will be implemented by social workers, as well as by nurses, physicians, psychologists
and other health technicians traditionally included in these intervention programs in public health.
This systematic review aims to understand the relevance of the qualitative methodology in the
field of community health with the elderly, namely the existing publications and their results, with
implications for the emergence of guidelines for socio-educational intervention.
Problem Statement
According to WHO (2011) maintain independence and active life, strengthen health prevention
and promotion policies for elderly people, and maintain and/or improve the quality of life in aging, are the
main challenges for public health.
Therefore, it is an area of intervention with a strong component of epidemiology, but with the
participation of multiple areas of knowledge (medicine, statistics, law, social sciences ...) in intervention
planning. The social work intervention in health, particularly socio-educational intervention, constitutes a
privileged field of action, in empowering individuals for social life, fostering autonomy, responsibility,
understanding and involvement/participation in the surrounding environment, as well as the change of
behaviours, in order to improve their living conditions (Carvalho & Baptista, 2004). Community health
research with the elderly population has become increasingly important (Lima-Costa & Veras, 2003),
reinforced by the fact that population aging is considered one of the greatest challenges of contemporary
public health (WHO, 2011). In this context, quantitative and qualitative studies increase, highlighting the
latter by the possibility of identifying specific and contextual needs that become fundamental for local
intervention, enhancing results. Hence, it’s important to know the contributes of the qualitative research
in this field in order to improve the socio-educational intervention.
Research Questions
Given the problem statement, we formulated the following research questions: what’s the
relevance of qualitative methodology in the community health with elderly population? What are the
main themes and the main socio-educational practice implications in this field?
Purpose of the Study
The purpose of this systematic review paper is to identify and appraise the importance of the
qualitative methodology in the study of elderly in community health. It seeks to identify areas of existing
research, describe findings and analyse implications emerged for socio-educational intervention to inform
practice and further research.
Research Methods
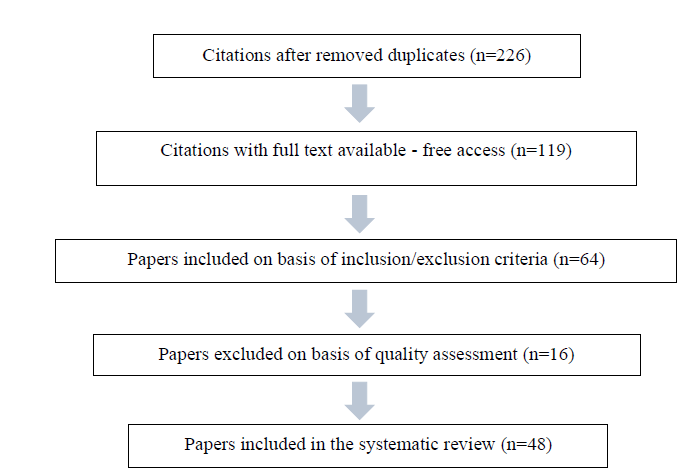
This is a systematic review and the relevant literature was identified through two electronic
databases: MEDLINE and PubMed (2010-2015). The search terms were qualitative research AND
community health AND elderly and the inclusion criteria were: published qualitative or mixed-method if
the qualitative methods could be considered as a separate section of the study; with elderly samples (≥65
years); and studies in community health. Following we excluded duplicates and 226 citations were
retrieved for possible inclusion in the present review. With full text available (free access) we found only
119 articles. The study selection criteria were applied by one author in consultation with at least one
other, by reading titles and abstracts, and if the source was suitable for inclusion, the full article was read.
Each study was rated for seven quality using pre-defined assessment criteria (Table
authors independently.
69
The final result of agreement between encoders was 94%, and discrepancies were discussed as a
panel with a third author to reach consensus. In the quality assessment were awarded grades ranging from
one (very poor) to four (good), providing a maximum score of 28, and only were accepted studies with
≥21 score. Finally, there were 48 articles included in the study, whose information extracted was
tabulated. Figure
Findings
The majority (20) of analysed studies came from Europe and 11 from North America, especially
from EUA, but we found studies in all Continents (Asia 7, Australia 5, South America 4 and Sub-Saharan
Africa 1). Study respondents were health professionals, informal carers, patients, community members
and relatives. According to the techniques of collecting dates, predominate semi structured interviews
(34) and focus group (16). Questionnaires, observation, workshops, inventories and document analysis,
all of them, only appear eleven times.
According to the themes, most (13) of the articles are focused on health care network, six on end-
of-life care and six on quality of life and successful aging. The others refer to multiples themes (Table
each of them with a frequency between one (7 references) and three (two references).
1.Legend: Courtney et al. (2010); 2. Heravi-Karimooi, Anoosheh, Foroughan, Sheykhi, & Hajizadeh (2010); 3. Mullen, Nicolson, & Cotton (2010); 4. Chan & Pang (2011); 5. Gysels, Pell, Straus, & Pool (2011); 6. Hansen, Bi, Nitschke, Pisaniello, Newbury, & Kitson (2011); 7. Kennedy, Harbison, Mahoney, Jarvis, & Veitch (2011); 8. Klymko, Artinian, Price, Abele, & Washington (2011); 9. Medbo, Melbye, & Rudebeck (2011); 10. Motta, Aguiar, & Caldas (2011); 11. Stewart, Goddard, Schiff, & Hall (2011); 12. Uchoa, Firmo, Lima-Costa, & Corin (2011); 13. van Uffelen, Heesch, Hill, & Brown (2011); 14. Yamada, Vass, Hvas, Igarashi, Hendriksen, & Avlund (2011); 15. Antonsson, Korjonen, & Rosengren (2012); 16. Huong, Hai Ha le, Quynh Chi, Hill, & Walton (2012); 17. Tsai, Wong, Ku, & Liu (2012); 18. Tynkkynen, Lehto, & Miettinen (2012); 19. Aase, Laugaland, Dyrstad, & Storm (2013); 20. Breitholtz, Snellman, & Fagerberg (2013); 21. Garcia, Espinoza, Lichtenstein, & Hazuda (2013); 22. Horder, Frandin, & Larsson (2013); 23. Muller-Mundt, Bleidorn, Geiger, Klindtworth, Pleschberger, Hummers-Pradier, & Schneider (2013); 24. Romo, Wallhagen, Yourman, Yeung, Eng, Micco, . . . Smith (2013); 25. Thai, Walter, Eng, & Smith (2013); 26. Turjamaa, Hartikainen, & Pietila (2013); 27. Zayas, Wisniewski, & Kennedy (2013); 28. Au, Wong, McMillan, Bridges, & McGrath (2014); 29. Cheung, Geisler, & Sunneberg (2014); 30. Corvol, Balard, Moutel, & Somme (2014); 31. Countouris, Gilmore, & Yonas (2014); 32. Ferretti, Gris, Mattiello, Paz Arruda Teo, & De Sa. (2014); 33. Gilmartin, Marriott, & Hussainy (2014); 34. Goth & Smaland (2014); 35. Heppenstall, Keeling, Hanger, & Wilkinson (2014); 36. Resnick, Michael, Griffith, Klinedinst, & Galik (2014); 37. Riva, Monti, Iannello, Pravettoni, Schulz, & Antonietti (2014); 38. Wiig, Guise, Anderson, Storm, Lunde Husebo, Testad, . . . Moltu (2014); 39. Andreasen, Lund, Aadahl, Gobbens, & Sorensen (2015); 40. Bindels, Cox, Abma, van Schayck, & Widdershoven (2015); 41. Geisler & Cheung (2015); 42. Holloway, Toye, McConigley, Tieman, Currow, & Hegarty (2015); 43. Karki, Bhatta, & Aryal (2015); 44. Ligthart, van den Eerenbeemt, Pols, van Bussel, Richard, & Moll van Charante (2015); 45. McCloskey, Jarrett, & Stewart (2015); 46. Pereira, Giacomin, & Firmo (2015); 47. Philippi, Luderer, & Altenhoner (2015); 48. van Erning, Janssen-Heijnen, Creemers, Pruijt, Maas, & Lemmens (2015)
About the healthcare network for the elderly, the main conclusions are: a) elderly-related health
and social policies and national guidelines related on what is best for the local people rather than related
to the benefits of the governmental or municipality, contrary to what is most frequent; this has a potential
to compromise the affordability of the services and undermining the principles of the welfare state; b) the
needs of hierarchically organized services and levels of care that provide support for the healthcare teams'
work; d) a good relationship between participating organizations and professionals is required for
successful by identifying barriers concerning institutional collaboration.
We also found that: e) structural funding and the need of education programs for teams, that
facilitate the development of professional and personal skills, including project leadership are also key
elements; f) the psychological and social resources should be valued as well as the economical resource;
g) It is fundamental to identify needs, including instrumental activities of daily living, from the elderly,
families and caregivers, to support programs and services that emphasize person-centered approach; h)
community involvement to promote supportive social networks including the participation of the elderly.
Concerning the end-of-life care planning, stands out: a) the identification of decision-making
processes for the elderly and caregivers, and the development of strategies to involve them (self-
determination), adopting a person-centered approach; b) understanding sociocultural specificity in
choices; c) find methods of overcoming the barriers\ perceived by the elderly; d) adjust care throughout
the aging process in terms of clinical, psychosocial and information needs. Promote quality of life (QoL)
and successful aging, it is important, according to the elaborated synthesis: a) to measure QoL as a
support for the intervention; b) respect the elderly (interests and values); c) understand the elderly's
perception about successful enrichment, to improve communication with the technicians and the
intervention; d) involve the elderly in volunteering activities with peers; e) stop and prevent resignation of
the elderly. Different conclusions, given the diversity of themes, can be drawn from the remaining
articles. However, all refer the possibility of using the results in terms of developing socio-educational
actions. Indeed, in general, all results point out changeable behavioral aspects, as well as providing,
identifying and respecting individual and collective specificities in the intervention to promote successful
aging.
Conclusion
Qualitative research in elderly community health can help researchers to gain a more complete
understanding or interpret the results of quantitative data more completely, as well as show local
specificities. Europe and North America stand out with the greatest focus (33 out of 48 studies) in the
review. Generally, there is an investment in the network of care, end-of-life care planning and quality of
life and active aging.
In terms of conclusions, emphasis is placed on the need to value the interests and needs of the
elderly and caregivers, focusing on less economic approaches, favoring psychological, personal and social
aspects, as well as people-centered interventions. It is also noted the concern to capture the perceptions of
all involved in the aging process: health professionals, informal carers, patients, community members and
relatives.
We observed an increase in the qualitative studies, in multiple themes, that support a socio-
educational intervention respecting the individual, local and regional specificities, in order to value and
imply the individual in the modification of behaviors that promote an aging with quality. Professionals in
this area can and should collaborate intensively in multidisciplinary teams that also involve health
professionals. We emphasize a limitation due to the inclusion of free access texts, hence the need to revise all the
texts resulting from the research and the inclusion criteria referring to the nature and characteristics of the
works. We believe that the search for research in other electronic databases and other time periods is
relevant. It is important to use these and other results of similar work as support for programs and socio-
educational practices.
Acknowledgments
To the Centre for Studies in Education, Technologies and Health (CI&DETS) at the Polytechnic
Institute of Viseu, Portugal.
References
- Araújo, P., Martins, E., Fernandes, R., & Mendes, F. (2016). O método das histórias de vida na investigação qualitativa em psicologia. In A. Costa, P. Castro, S. Sá, J. Carvalho, F. Souza, & D.
- Souza (Eds.), Atas do 5º Congresso Ibero-Americano em Investigação Qualitativa - Investigação Qualitativa na Educação (pp. 588-595). Porto: Ludomedia.
- Barbosa, L., Motta, A., & Resck, Z. (2015). Os paradigmas da modernidade e pós-modernidade e o processo de cuidar na enfermagem. Enfermería Global, 37, 342-349.
- Bogdan, R., & Bilken, S. (1998). Qualitative research for education: An introduction for theory and methods. Boston: Allyn and Bacon.
- Britten, N. (2005). Making sense of qualitative research: A new series. Med Educ, 39(1), 5-6.
- Carvalho, A., & Baptista, I. (2004). Educação Social. Fundamentos e estratégias. Porto: Porto Editora. Countouris, M., Gilmore, S., & Yonas, M. (2014). Exploring the impact of a community hospital closure on older adults: a focus group study. Health Place, 26, 143-148.
- doi:10.1016/j.healthplace.2013.11.008 Courtney, K. L., Lingler, J. H., Mecca, L. P., Garlock, L. A., Schulz, R., Dick, A. W., & Olshansky, E.
- (2010). Older adults' and case managers' initial impressions of community-based telehealth kiosks. Research in gerontological nursing, 3(4), 235-239.
- Coutinho, C. (2011). Metodologia de investigação em ciências sociais e humanas: Teoria e prática. Coimbra: Edições Almedina.
- Ferretti, F., Gris, A., Mattiello, D., Paz Arruda Teo, C. R., & De Sa, C. (2014). [Impact of a health education program on the elderly's knowledge about cardiovascular diseases]. Impacto de programa de educacao em saude no conhecimento de idosos sobre doencas cardiovasculares. Revista de salud publica (Bogota, Colombia), 16(6), 807-820.
- Garcia, C. H., Espinoza, S. E., Lichtenstein, M., & Hazuda, H. P. (2013). Health literacy associations between Hispanic elderly patients and their caregivers. J Health Commun, 18 Suppl 1, 256-272.
- doi:10.1080/10810730.2013.829135 Geisler, C. C., & Cheung, C. K. (2015). Complementary/alternative therapies use in older women with arthritis: Information sources and factors influencing dialog with health care providers. Geriatr Nurs, 36(1), 15-20. doi:10.1016/j.gerinurse.2014.08.013 Gilmartin, J. F., Marriott, J. L., & Hussainy, S. Y. (2014). Exploring factors that contribute to dose administration aid incidents and identifying quality improvement strategies: the views of pharmacy and nursing staff. Int J Pharm Pract, 22(6), 407-414. doi:10.1111/ijpp.12091 Goth, U. S., & Smaland, E. (2014). The role of civic engagement for men's health and well being in Norway-a contribution to public health. Int J Environ Res Public Health, 11(6), 6375-6387.
- doi:10.3390/ijerph110606375 Gysels, M., Pell, C., Straus, L., & Pool, R. (2011). End of life care in sub-Saharan Africa: a systematic review of the qualitative literature. BMC Palliat Care, 10, 6. doi:10.1186/1472-684X-10-6
- Hansen, A., Bi, P., Nitschke, M., Pisaniello, D., Newbury, J., & Kitson, A. (2011). Perceptions of heat-susceptibility in older persons: barriers to adaptation. Int J Environ Res Public Health, 8(12), 4714-4728. doi:10.3390/ijerph8124714 Heppenstall, C. P., Keeling, S., Hanger, H. C., & Wilkinson, T. J. (2014). Perceived factors which shape decision-making around the time of residential care admission in older adults: a qualitative study.
- Australas J Ageing, 33(1), 9-13. doi:10.1111/j.1741-6612.2012.00644.x Heravi-Karimooi, M., Anoosheh, M., Foroughan, M., Sheykhi, M. T., & Hajizadeh, E. (2010).
- Understanding loneliness in the lived experiences of Iranian elders. Scand J Caring Sci, 24(2), 274-280. doi:10.1111/j.1471-6712.2009.00717.x Holloway, K., Toye, C., McConigley, R., Tieman, J., Currow, D., & Hegarty, M. (2015). National consultation informing development of guidelines for a palliative approach for aged care in the community setting. Australas J Ageing, 34(1), 21-26. doi:10.1111/ajag.12083 Horder, H. M., Frandin, K., & Larsson, M. E. (2013). Self-respect through ability to keep fear of frailty at a distance: successful ageing from the perspective of community-dwelling older people. Int J Qual Stud Health Well-being, 8, 20194. doi:10.3402/qhw.v8i0.20194 Huong, N. T., Hai Ha le, T., Quynh Chi, N. T., Hill, P. S., & Walton, T. (2012). Exploring quality of life among the elderly in Hai Duong province, Vietnam: a rural-urban dialogue. Glob Health Action, 5, 1-12. doi:10.3402/gha.v5i0.18874 Karki, S., Bhatta, D. N., & Aryal, U. R. (2015). Older people's perspectives on an elderly-friendly hospital environment: an exploratory study. Risk Manag Healthc Policy, 8, 81-89.
- doi:10.2147/RMHP.S83008 Kennedy, C., Harbison, J., Mahoney, C., Jarvis, A., & Veitch, L. (2011). Investigating the contribution of community nurses to anticipatory care: a qualitative exploratory study. Journal of advanced nursing, 67(7), 1558-1567.
- Klymko, K. W., Artinian, N. T., Price, J. E., Abele, C., & Washington, O. G. (2011). Self-care production experiences in elderly African Americans with hypertension and cognitive difficulty. J Am Acad Nurse Pract, 23(4), 200-208. doi:10.1111/j.1745-7599.2011.00605.x Ligthart, S. A., van den Eerenbeemt, K. D., Pols, J., van Bussel, E. F., Richard, E., & Moll van Charante, E. P. (2015). Perspectives of older people engaging in nurse-led cardiovascular prevention programmes: a qualitative study in primary care in the Netherlands. Br J Gen Pract, 65(630), e41-48. doi:10.3399/bjgp15X683149 McCloskey, R., Jarrett, P., & Stewart, C. (2015). The Untold Story of Being Designated an Alternate Level of Care Patient. Healthcare policy = Politiques de sante, 11(1), 76-89.
- Medbo, A., Melbye, H., & Rudebeck, C. E. (2011). "I did not intend to stop. I just could not stand cigarettes any more." A qualitative interview study of smoking cessation among the elderly. BMC Fam Pract, 12, 42. doi:10.1186/1471-2296-12-42 Motta, L. B., Aguiar, A. C., & Caldas, C. P. (2011). [The Family Health Strategy and healthcare for the elderly: experiences in three Brazilian cities]. Cad Saude Publica, 27(4), 779-786.
- Mullen, K., Nicolson, M., & Cotton, P. (2010). Improving medical students' attitudes towards the chronic sick: a role for social science research. BMC medical education, 10, 84.
- Muller-Mundt, G., Bleidorn, J., Geiger, K., Klindtworth, K., Pleschberger, S., Hummers-Pradier, E., & Schneider, N. (2013). End of life care for frail older patients in family practice (ELFOP)--protocol of a longitudinal qualitative study on needs, appropriateness and utilisation of services. BMC Fam Pract, 14, 52. doi:10.1186/1471-2296-14-52 Pereira, J. K., Giacomin, K. C., & Firmo, J. O. (2015). [Functionality and disability in old age: to stay still or not to stay still]. Cad Saude Publica, 31(7), 1451-1459. doi:10.1590/0102-311X00046014 Philippi, M., Luderer, C., & Altenhoner, T. (2015). ["So I would have been sitting at home and moping...": How do older single people in need of support experience companionship by volunteers after discharge from hospital?].
- Resnick, B., Michael, K., Griffith, K., Klinedinst, J., & Galik, E. (2014). The impact of PRAISEDD on adherence and initiation of heart health behaviors in senior housing. Public Health Nurs, 31(4), 309-316. doi:10.1111/phn.12080
- Riva, S., Monti, M., Iannello, P., Pravettoni, G., Schulz, P. J., & Antonietti, A. (2014). A preliminary mixed-method investigation of trust and hidden signals in medical consultations. PLoS One, 9(3), e90941. doi:10.1371/journal.pone.0090941 Romo, R. D., Wallhagen, M. I., Yourman, L., Yeung, C. C., Eng, C., Micco, G., . . . Smith, A. K. (2013).
- Perceptions of successful aging among diverse elders with late-life disability. Gerontologist, 53(6), 939-949. doi:10.1093/geront/gns160 Santos, Q., Azevedo, D., Costa, R., & Medeiros, F. (2011). A crise de paradigmas na ciência e as novas perspectivas para a enfermagem. Escola Anna Nery Rev. Enferm.,15(4), 833-837.
- Stewart, F., Goddard, C., Schiff, R., & Hall, S. (2011). Advanced care planning in care homes for older people: a qualitative study of the views of care staff and families. Age Ageing, 40(3), 330-335.
- doi:10.1093/ageing/afr006 Thai, J. N., Walter, L. C., Eng, C., & Smith, A. K. (2013). Every patient is an individual: clinicians balance individual factors when discussing prognosis with diverse frail elderly adults. J Am Geriatr Soc, 61(2), 264-269. doi:10.1111/jgs.12098 Tsai, Y. F., Wong, T. K., Ku, Y. C., & Liu, W. C. (2012). Reasons for living among older male Chinese residents of veterans' homes. J Adv Nurs, 68(9), 1978-1987. doi:10.1111/j.1365-2648.2011.05884.x Turato, E. (2005). Qualitative and quantitative methods in health: Definitions, differences and research subjects. 39(3), 1-8.
- Turjamaa, R., Hartikainen, S., & Pietila, A. M. (2013). Forgotten resources of older home care clients: focus group study in Finland. Nurs Health Sci, 15(3), 333-339. doi:10.1111/nhs.12037 Tynkkynen, L. K., Lehto, J., & Miettinen, S. (2012). Framing the decision to contract out elderly care and primary health care services - perspectives of local level politicians and civil servants in Finland.
- BMC Health Serv Res, 12, 201. doi:10.1186/1472-6963-12-201 Uchoa, E., Firmo, J. O. A., Lima-Costa, M. F., & Corin, E. (2011). An anthropologic study on strategies for addressing health problems among the elderly in Bambui, Minas Gerais State, Brazil. Cadernos de saude publica, 27 Suppl 3, S370-377.
- van Erning, F. N., Janssen-Heijnen, M. L., Creemers, G. J., Pruijt, H. F., Maas, H. A., & Lemmens, V. E.
- (2015). Deciding on adjuvant chemotherapy for elderly patients with stage III colon cancer: a qualitative insight into the perspectives of surgeons and medical oncologists. J Geriatr Oncol, 6(3), 219-224. doi:10.1016/j.jgo.2015.02.001 van Uffelen, J. G., Heesch, K. C., Hill, R. L., & Brown, W. J. (2011). A qualitative study of older adults' responses to sitting-time questions: do we get the information we want? BMC Public Health, 11, 458. doi:10.1186/1471-2458-11-458 Wiig, S., Guise, V., Anderson, J., Storm, M., Lunde Husebo, A. M., Testad, I., . . . Moltu, K. L. (2014).
- Safer@home-Simulation and training: the study protocol of a qualitative action research design.
- BMJ Open, 4(7), e004995. doi:10.1136/bmjopen-2014-004995 World Health Organization (2011). Global Health and Aging. Obtido de http://www.who.int/ageing/publications/global_health.pdf Yamada, Y., Vass, M., Hvas, L., Igarashi, A., Hendriksen, C., & Avlund, K. (2011). Collaborative relationship in preventive home visits to older people. Int J Older People Nurs, 6(1), 33-40.
- doi:10.1111/j.1748-3743.2010.00213.x Zayas, L. E., Wisniewski, A. M., & Kennedy, T. (2013). Instrumental activity of daily living limitations and supports in a clinic population of low-income Puerto Rican elderly adults with chronic diseases. J Am Geriatr Soc, 61(10), 1789-1795. doi:10.1111/jgs.12461
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
08 May 2017
Article Doi
eBook ISBN
978-1-80296-021-1
Publisher
Future Academy
Volume
22
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-283
Subjects
Psychology, clinical psychology, psychotherapy, abnormal psychology
Cite this article as:
Martins, E., Fernandes, R., Mendes, F., & Magalhães, C. (2017). Qualitative Studies In Community Health: A Systematic Review In The Elderly Population. In Z. Bekirogullari, M. Y. Minas, & R. X. Thambusamy (Eds.), Clinical & Counselling Psychology - CPSYC 2017, vol 22. European Proceedings of Social and Behavioural Sciences (pp. 66-75). Future Academy. https://doi.org/10.15405/epsbs.2017.05.9

