Psychological Intervention For Improving Prenatal Attachment Of Pregnant Women With A History Of Previous Miscarriage
Abstract
Given that pregnant women who went through the miscarriage experience during one or moreprevious pregnancies have difficulties in forming emotional attachments to the fetus during the current pregnancy, development of psychological interventions for improving their maternal-fetal attachment is needed. The aim of this study is to present a psychological intervention centered on the Unifying-Experiential Psychotherapy for improving the prenatal attachment in pregnant women with a history of miscarriage and to investigate its effectiveness. Hence, 32 pregnant women at 10-30 weeks of gestation, who reported miscarriage in previous pregnancies, were divided in two groups: experimental and control group. All participants had completed Romanian version of Maternal-Fetal Attachment Scale MFAS) (
Keywords: Maternal-fetal attachmentmiscarriagepregnancyprenatal psychology
Introduction
Out of all the pregnancy specific complications, miscarriage has the highest incidence. Because
most miscarriages occur during the first trimester, the trend among Romanian obstetricians is to ignore
this experience, especially when it is a singular one, be it at that respective moment in time or during a
following pregnancy arguing with reasons such as: It’s a common occurrence, It was just an accident,
Your loss was not an actual baby etc.
However, for women that went through a miscarriage, including the post-miscarriage period, this
experience is quite a complex one and mainly influenced by many variables: physical pain during the
moment of miscarriage, social support, age, whether the pregnancy was a natural one or obtained via IVF
procedure, if it was a desired one or unwanted, or on the information received from the medical staff.
Given that approximately 50% of women who experience a miscarriage get pregnant again,
increasingly more studies have focused on investigating the impact of prenatal losses during the
following pregnancies. Out of these, the most frequently mentioned are the pregnancy specific anxiety
(Franche & Mikail, 1999; Geller, Kerns and Klier, 2004; Bergner, Beyer, Klapp & Rauchfuss, 2008) and
its effects on prenatal maternal-fetal attachment (Armstrong &Hutti, 1998 Armstrong 2004, O'Leary,
2004; Tsartsara & Johnson, 2006). It is important here to mention that most of these studies are
considering the entire prenatal losses registry, and not just the miscarriages.
An interesting fact regarding prenatal attachment on women with a history of miscarriage is that
the qualitative studies, the conclusions and the recommendations given in the course of some quantitative
studies, highlight the strong mechanisms for avoiding emotional attachment towards the fetuses in
pregnant women during the current pregnancy. As a need to protect themselves from a new suffering after
a possible abortion, pregnant women tend to emotionally distance themselves from the pregnancy, to
retain their feelings towards the fetus, focusing exclusively on a healthy intrauterine development in order
to avoid a new miscarriage (M. Andersson, S. Nilsson, A. Adolfsson, 2011; Green & Solnit, 1964 Carey
Smith, 198; Cote-Arsenault & Mahlangu, 1998; Cote-Arsenault & B. Morrison, 2001).
Because prenatal maternal attachment was associated with the adoption of healthy behaviors in
pregnancy – e.g. nutrition, sports, giving up smoking, alcohol and drugs (Lindgren, 2001; Ustunsoz,
Guvenc, Akyus, Oflaz, 2010; Ross, 2012), with the postnatal mother - newborn attachment (Fonaggy,
Steele & Steele, 1991; Benoit Parker & Zeanah, 1997; Siddiqui & Hagglof, 2000), clinicians are more
and more concerned to develop psychological interventions focused on prenatal attachment. The existent
psychological interventions focus on different techniques as mindfulness meditation (Duncan &
Bardacke, 2009), listening to music (Chang, Yu, Chen, Chen, 2015), abdominal palpation using Leopold's
maneuvers (Nishkawa & Sakakibara, 2013), reflective functioning (Jenkins & Williams, 2008), relaxation
training (Toosi, Akbarzadeh, Farkhondeh & Zare, 2014).
The prenatal attachment implications are sustained both by its complexity and by the variety of its
meanings, for example, Cranley M. (1981) defines prenatal attachment based on the affiliation and the
interaction behaviors of the pregnant women to the fetus, while M. Muller (1993) takes into account the
unique and affectionate character of the relationship between the mother and the unborn child and
Condon (1993), the love towards the fetus. Doan and Zimerman (2003) define prenatal attachment as an
abstract concept, which is representative for the affiliate relationship between the parent and the child,
potentially present even before pregnancy, which depends on cognitive and emotional abilities to
conceptualize another human being and that is developed within an ecological system.
Problem Statement
Given that pregnant women who went through the miscarriage experience during one or more
previous pregnancies have difficulties in forming emotional attachments to the fetus during the current
pregnancy, it is necessary that the psychological intervention refer primarily to the emotional dimension
of these women.
So, they need to be encouraged to experiment different personal and original interactions with their
fetuses using expressive-creative means, so as to be able to build a healthy and safe attachment during
pregnancy. Concerning this, the Unifying-Experiential Psychotherapy, method developed by Mitrofan
(2004) and centered on symbol analysis, personal and self-change development through challenging
exercise, on the creative improvisation and meditation with art-therapy and expressive support, answers to
the genuine psychological needs during pregnancy.
PEU focuses on three axes of intervention – the identity roles axis, the time axis and the awareness
axis, among which, subjective experiences are being processed through a four-step methodology:
a) the identification of lived through experiences, their meanings and manifestations;
b) the connection and analysis of the level of merger of the experiences with the verbal and
nonverbal external manifestations;
c) the symbolic outsourcing or reconstitution of traumatic experiences that allow their exploration
and redefinition;
d) the creative self-transformation based on the activation of inventive resources by methods of
identification, formulation, rearrangement and integration of alternative, healthy and creative solutions,
actions and behaviors. Each of the three experiential- unifying ways aims specific milestones, and their
unifying effect is the result of the simultaneous and interrelated functioning.
Research Questions
The questions that we ask ourselves in this study are:
i. What is the specific of psychological intervention carried out in order to optimize the
maternal-fetal attachment in pregnant women with a history of miscarriage?
ii. To what extent does the therapeutic intervention program proposed lead to the
improvement of the maternal-fetal attachment in pregnant women with a history of
miscarriage?
Purpose of the Study
The purpose of this article is to present a psychological intervention centered on the Unifying-
Experiential Psychotherapy techniques (Mitrofan, 2004) formulatedin order to optimize the maternal-
fetal attachment in women with a history of miscarriage and also to examine its effectiveness on the
maternal-fetal relationship.
Research Methods
Instruments
The participants’ prenatal attachment to her fetus is assessed before and after psychological
intervention using the Romanian version of Maternal-Fetal Attachment Scale (Cranley 1981), which
contains 22 items. MFAS is not just the first, but also one of the most widely used instruments in
measuring prenatal attachment in the world. The items are conceived as sets of affirmations, and each
item measures one of five dimensions or subscales of the prenatal attachment identified by Cranley, that
is Differentiation of Self from Fetus, Interaction with the Fetus, Attributing Characteristics and Intentions
to the Fetus, Giving of the Self, and Role Taking. The response options in the MFAS are ranged from
“Definitely Yes” to “Definitely No”, and are scored from 1-5, with 5 being the most positive statement,
except 21 item for which options are reversed. The fidelity of Romanian version Cranley’s scale, α =
0.73, supports the fidelity α = 0.85 of the original instrument.
In spite of the fact that Cranley’s Maternal-Fetal Attachment Scale was constructed exclusively
based on a sample of pregnant women with gestation ages between 35 and 40 weeks, the data obtained
through relating the scores to variables such as age, socio-economic status, parity, self-confidence,
perceived stress support the idea of hierarchically ordering behaviours specific to the maternal-fetal
attachment and the fact that some dominate over others throughout the various stages of pregnancy. Also,
the administration of MFAS in the first and second trimesters of pregnancy allows for the measurement of
the development stage of each behaviour, which in turn allows for the evaluation of their evolution and
for highlighting any risky situations as far as the maternal-fetal relationship is concerned.
Participants
Our study involved 32 pregnant women (10-30 weeks of gestation, m = 22.28, std. deviation =
6.65) with a history of miscarriage, recruited from the database of a private center in Bucharest providing
prenatal service, as well as via online publishing of an information notice regarding this research on blogs
for future parents. All expecting mothers involved in this study are married and aged between 27 and 39,
with an average age of 30.6 years old.
The criteria for including pregnant women as participants were:
i.age over 18;
ii.the existence of at least one previous miscarriage,
iii.confirmed pregnancy;
iv.willingness to participate in this study.
The participants were divided into two groups: one experimental group (N = 16) and one control
group (N = 16). From the experimental group, 11 pregnant women went in previous pregnancy through a
singular experience of miscarriage, 4 of them went through two miscarriages and one pregnant woman
through three miscarriages. The pregnant women in the control group, experienced one single
miscarriage.
All participants had completed Romanian version of MFAS in the pre-experiment and post-
experiment stages. The experimental group participated in a psychological intervention program which
we present below, while the control group did not benefit of any psychological intervention.
Description of psychological intervention program
The psychological intervention program was conducted over 10 weeks and included one individual
session and 9 group sessions. During the individual session, the pregnant women have undergone a semi-
structured interview covering three areas: current pregnancy, previous pregnancy / previous miscarried
pregnancies and the experience going through miscarriage. The group sessions were held on a weekly
bases, for 3 hours each. As expressive-creative means used in our intervention we can mention here was:
dancing and movement, collage, creative improvisation, centered on musical rhythm, guided meditation
and the actual story.
During the first group session, information regarding the purpose of the intervention and the
principles of the experimental-unifying orientation on which the intervention that took place after were
presented. Also, we clarified the rules of the group and the administrative aspects regarding the group
sessions: the program, the location, the number of sessions, the duration and frequency of the meetings. In
order to develop a group cohesion, every participant opened up about herself, her pregnancies (current
and previous one/s) and their motivation to participate in the prenatal attachment improvement program
developed by us. After that, using some dies with images on them, the participants working together
formulated a definition of the prenatal maternal-fetal attachment. Finally, they were verbally encouraged
to explore the group experience, process that revealed enlightening insights on the personal significance
attributed to the maternal-fetal relationship.
From the second meeting, all the sessions were held with a common structure composed of four
parts:
1) group cohesiveness by free sharing of mutual novelties on the pregnancy evolution of each
participant (e.g. information on the size of the fetus, the results of medical tests, appearance / reduction /
disappearance of physiological discomforts during pregnancy etc.);
2) introducing a provocative exercise specific to experiential psychotherapy, based on art-
therapeutic techniques;
3) analysis and verbal exploration on the experience within the exercise;
4)closing by highlighting new resources, significances, and emotional implications in order to
integrate them within the realistic and healthy actions of the participants during the pregnancy and after.
Thus, given that parts 1, 3 and 4 of the group sessions are similar in their evolution, further we
shall only describe the challenging exercises.
During the second session we used an exercise inspired from dancing and movement therapy with
musical support from the "Earth Spirit" Carlos Nakai collection for flute. After an exercise on relaxation
and guided meditation, we asked them to position in a circle and greet the entire group via movement. In
return, the group responds the greeting by movement also reflecting it exactly the same.
Then, one by one, each of the pregnant women enters the circle and is encouraged to act and
express through dance and movement the relationship with their unborn baby. To prevent possible
accidents and sustain the attachment theme, each one chooses a partner from the support group to keep
close for physical support and more. Throughout the dance, the other pregnant women, sited in the circle,
carefully pay attention to the movements of the pregnant woman in the center and also to their own
thoughts, questions, emotions, needs, movements. One by one, each pregnant woman is part of the
continuous circle and of the circle’s content as well.
The purpose of the 3rd session of the group was to put the participants in touch with the maternal-
fetal relationship specific rhythm, but also with the rhythm changes that occur during pregnancy. In order
to do this, we introduced a provocative exercise using Boom Whackers polyphonic tubes which are
percussion instruments. First, the participants are invited to play with the chords tubes, hitting them with
their palms, thighs or the floor, and then, each creating a personal musical rhythm, rhythm that can later
be followed by the group. This exercise them in increasing responsiveness to the personal rhythm, rhythm
produced by another person and the changes of pace and awareness of thoughts, moods, needs and
behaviors related to the sender and receiver experience.
In the 4th session we focused on differentiating between the past prenatal experiences, from the
previous to the present pregnancy, from the previously spontaneously stopped evolving fetus and the fetus
currently in the womb. This way, our intervention is in line with J. O 'Leary (2016), who emphasized the
need to support mental representations of the parental role in connection to both the stop evolving fetus
(the deceased baby) and the current one (the unborn baby). After a relaxation exercise, the participants
were challenged by using plastic clay, to mold to a certain form the fetus from the pregnancy that ended
in miscarriage and the fetus form the current one. This way, the pregnant women are actually aware that
they use different symbols and mental representations for their fetuses and that they continue to develop
an attachment relationship with each and every one of them, realizing that "they are parents to two babies,
the one who dies and the one in the present pregnancy "(O'Leary 2016).
The 5th group session, our psychological intervention continues to support the needs of unborn
baby, giving them voice. During the provocative exercise from this session, the participants have
completed sentences / phrases beginning with a given start, as if the current unborn baby would actually
talk to them about his needs.
Considering the temporal interference plans (past with present, previous pregnancy with current
pregnancy) that we noticed during the individual sessions when talking about the ongoing pregnancy, in
the 6th group session we intended to evaluate the status of this interference. For this purpose, we used the
story with a given beginning as a prenatal experience exploring instrument. Each participant received an
A4 sheet of paper on which the introductory sentence of the story was written:
was a kangaroo bearing in its pouch a precious crystal ...."
Sessions 7 and 8 beyond the mindfulness exercises, were focused on the interaction with the fetus
through different techniques: singing, speaking, reading, writing, touching, massaging, visualization,
playing in order to stimulate the prenatal attachment behavior through the expressive communication and
creative actions according to their personal resources. The focus was on becoming aware of their own
bodily sensations, emotions and thoughts from here and now, the existence of fetal movements, issues
that we explored verbally later within the group.
In the last group session, we focused through collage technique, on the integration of maternal-
fetal attachment components and on assessment of their prenatal attachment progress during our
psychological intervention program.
Findings
Our study focuses on presenting a psychological intervention in order to improve the prenatal
attachment in pregnant women with a history of miscarriage and also to measure its effectiveness.
According to Table.1, the results in this study show that after our psychological intervention are
significant differences in prenatal attachment, that is the MFAS overall score, in pregnant women in the
experimental group compared to the control group (t (29.66) = 2.87, p <0.05).
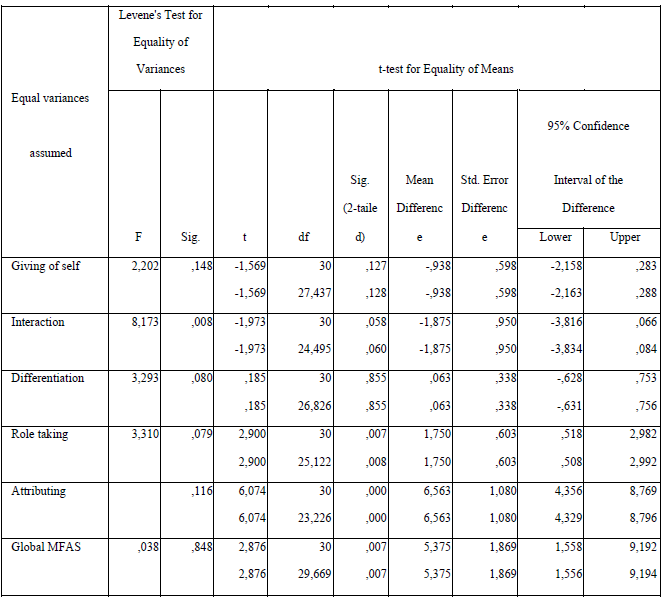
On the MFAS subscale level, the results show that for the Attributing characterics to the fetus
and Roletaking subscale level, pregnant women in the experimental group compared with ones in the
control group had significantly higher scores or t (23.22) = 6.07, p <0.05 and t (25,12) = 2.90, p <0.05.
Regarding the other scales - Interaction, Differentiation of Self from Fetus, Giving of Self, we can
notice that the scores increase both for pregnant women in the experimental group and for the ones in
the control group, with no significant difference between them. We believe that this is due to specific
intrauterine fetal development, with frequent and strong movements that begin to structure in ceritain
recognizable patterns known by pregnant women, but also as a response to the ways of interaction of
pregnant women. In this regard, the results obtained are consistent with those obtained by Cranley
showing that maternal fetal attachment increases during pregnancy.
We consider that Giving of Self subscale scores of the two groups are closely related to the
history of miscarriage of the participants, whereas the adoption of healthy practices in the current
pregnancy is for the pregnant women a way to avoid another perinatal loss and so ensure the viability of
the fetus.
Significant differences between the two subgroups on the prenatal attachment overall score, but
also on the Attributing characteristics to the fetus and Role-taking scores subscales, arising from our
psychological intervention support its effectiveness in improving maternal-fetal relationship.
As result of our study, we can say that through the creative language used according the Unifying
Experiential Psychotherapy in our psychological attachment intervention, the pregnant women had a
direct access to their own “here and now” experiences with their unborn babies. In this way, the
participants of or experimental group became aware of the way they get in touch with their fetus from a
cognitive, emotional, and behavioural point of view, the difficulties preventing them from establishing a
secure and intense attachment relationship to their fetus
Conclusion
The results confirm that the psychological intervention is an important factor in improving the
maternal-fetal relationship for pregnant women with a history of miscarriage. Just time as factor or
moving from week to week in pregnancy is not always enough to reach a strong and secure maternal fetal
attachment. Depending on the type and number of previous losses, structure of personality, social
support, reaching a strong prenatal attachment requires or not involvement of pregnant women in
psychological programs to support and improve their relationship with unborn babies.
In this regard, gynecologists should pay special attention to pregnant women with a history of
prenatal loss and encourage them to participate in therapy groups focused on psychological counseling in
order to optimize their maternal-fetal attachment.
Also, because there are pregnant women who have been through not only early but also late
miscarriages (which occurred after the 13th week of gestation) or recurrent (minimum 3 miscarriages), it
is necessary that gynecologists work closely with psychologists, who in return to provide the most
specific psychological interventions, responding to psychophysiological peculiarities of the participating
pregnant women.
The limitations of our study are considering the small number of expecting mother involved, and
the lack of standardization of some variables (i.e.: age, abortion history, age of gestation, etc.), and for
this reason is necessary to extend this psychological intervention to a larger group of pregnant women
with miscarriage in history.
References
- Andersson, I.M., Nilsson, S., Adolfsson, A. (2012). How women who have experienced one or more miscarriages manage their feelings and emotions when they become pregnant again – A qualitative interview study. Scandinavian Journal of Caring Sciences, 26, 262-270.
- Armstrong, D., Hutti, M. (1998). Pregnancy after Perinatal Loss: The relationship between anxiety and prenatal attachment. Journal of Obstetric, Gynecologic & Neonatal Nursing, 27(2),183-189.
- Armstrong, D. (2004). Impact of Prior Perinatal Loss on Subsequent Pregnancies. Journal of Obstetric,Gynecologic & Neonatal Nursing, 33 (6), 765-773.
- Benoit, D., Parker, K. C., & Zeanah, C. H. (1997). Mothers' representations of their infants assessed prenatally: stability and association with infants' attachment classifications. Journal of Child Psychology and Psychiatry, 38(3), 307-13.
- Bergner A., Beyer R., Klapp BF, Rauchfuss M. (2008). Pregnancy after early pregnancy loss: a prospective study of anxiety, depressive symptomatology and coping. Journal of Psychosomatic Obstetrics & Gynaecology, 29(2), 105-13.
- Chang, S., Park, S., & Chung, C. (2004). Effect of Taegyo-focused Prenatal Education on Maternal-fetal Attachment and Self-efficacy Related to Childbirth. Journal of Korean Academy of Nursing, Vol. 34, No. 8.
- Condon, J.T. (1993). The assessment of antenatal emotional attachment: development of a questionnaire instrument. British Journal of Medical Psychology, 66 (Pt 2), 167-83.
- Cranley, M.S. (1981). Development of a tool for the measurement of maternal attachment during pregnancy. Nursing Research, 30, 281–284.
- Doan, H.Mck., & Zimerman, A. (2003). Conceptualizing Prenatal Attachment: Toward a Multidimensional View. Journal of Prenatal & Perinatal Psychology & Health, 18. 2 (Winter 2003): 109-129.
- Duncan, L.G., & Bardacke, N. (2010). Mindfulness-Based Childbirth and Parenting Education: Promoting Family Mindfulness During the Perinatal Period. Journal of Child and FamiliesStudies ,19(2):190-202.
- Fonagy, P., Steele, H., & Steele, M. (1991). Maternal representations of attachment during pregnancy predict the organization of infant-mother attachment at one year of age. Child Development, 62:891–905.
- Franche, R. L, Mikail, S. F. (1999). The impact of perinatal loss on adjustment to subsequent pregnancy. Social Science & Medicine, 48:1613–1623.
- Geller P. A., Kerns D., Klier C.M. (2004). Anxiety following miscarriage and the subsequent pregnancy. A review of the literature and future directions. Journal of Psychosomatic Research, 56: 35-45.
- Green M., Solnit A.J. (1964). Reactions to the threatened loss of a child: A vulnerable child syndrome. Pediatric management od dying child, Part.III. Pediatrics, 34: 58-66.
- Jenkins, C., & Williams, A. (2008). The Mother-Baby Prenatal Group: Nurturing Reflective Functioning in a MethadoneMaintenance Clinic. Journal of Prenatal and Perinatal Psychology and Health, 22(3).
- Lindgren K. (2001).Relationships among maternal-fetal attachment, prenatal depression, and health practices in pregnancy. Research in Nursing & Health, 4(3):203-17.
- Nishikawa, M., Sakakibara, H. (2013). Effect of nursing intervention program using abdominal palpation of Leopold's maneuvers on maternal-fetal attachment. Reproductive Health Journal, 19;10:12. doi: 10.1186/1742-4755-10-12.
- Mitrofan, I. (2004). Terapia unificării. Abordarea holistică a dezvoltării și a transformării umane. Editura
- Sper, București.
- Muller, M.E. (1993). Development of the prenatal attachment inventory. Western Journal of Nursing
- Research, 15(2):199–215.
- O’Leary J. (2004). Grief and its impact on prenatal attachment in the subsequent pregnancy. Archives of
- Women’s Mental Health,7(1):7-18.
- O’Leary J., Warland J. (2016). Meeting the needs of parents pregnant and parenting after perinatal loss. Routledge Taylor & Francis Group.
- Siddiqui, A., & Hägglöf, B. (2000). Does maternal prenatal attachment predict postnatal mother–infant interaction?Early Human Development, 59, 1, 13–25 Toosi, M., Akbarzadeh, M., Sharif, F., & Zare N. (2014). The Reduction of Anxiety and Improved Maternal Attachment to Fetuses and Neonates by Relaxation Training in Primigravida Women.
- Women’s Health Bulletin, 1(1): e18968.
- Tsartsara, E., Johnson, M. P. (2006). The impact of miscarriage on women's pregnancy-specific anxiety and feelings of prenatal maternal-fetal attachment during the course of a subsequent pregnancy: an exploratory follow-up study. Journal of Psychosomatic Obstetrics and Gynecology, 27(3):173-82. Ustunsoz, A., Guvenc, G., Akyuz, A. & Oflaz, F. (2010). Comparison of maternal-and paternal-fetal attachment in Turkish couples. Midwifery2010, 26(2): e1-e9.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
08 May 2017
Article Doi
eBook ISBN
978-1-80296-021-1
Publisher
Future Academy
Volume
22
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-283
Subjects
Psychology, clinical psychology, psychotherapy, abnormal psychology
Cite this article as:
Camelia-Vasilica, C. (2017). Psychological Intervention For Improving Prenatal Attachment Of Pregnant Women With A History Of Previous Miscarriage. In Z. Bekirogullari, M. Y. Minas, & R. X. Thambusamy (Eds.), Clinical & Counselling Psychology - CPSYC 2017, vol 22. European Proceedings of Social and Behavioural Sciences (pp. 89-98). Future Academy. https://doi.org/10.15405/epsbs.2017.05.11

