Abstract
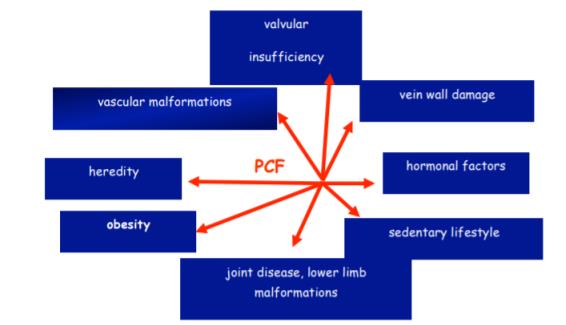
Peripheral circulatory failure (PCF) is a complex of lesions of different severity and magnitude affecting different leg veins which have in common a slowly progressive evolution of their condition and the occurrence of chronic complications. Varicose veins prevalence among the adult population; 10% - 33% in women and 10% - 20% respectively, in men, with an impressive socio-economic impact. RELIEF Study: 78% of symptomatic patients were untreated. This paper aims at addressing issues of peripheral circulation from a kinetic point of view. The trial was conducted by direct observation and tracking of the 121 cases studied between November 2014 and May 2015 within the SPINOF center of kinesiology at the Lower Danube University of Galati. The study showed the need for a minimum 3-week wellcoordinated kinetic program, adjusted to the stage of peripheral circulatory failure. Its association with drug therapy significantly decreases the intensity of specific symptoms and increases the duration of remission periods. Physical therapy is preferred for preventing the installation of peripheral circulatory failure, preferably in the case of people who are prone to peripheral collapse or present environmental factors favoring the emergence of peripheral circulatory failure, and becomes helpful in advanced stages of peripheral circulatory failure.
Keywords: Posturecompressionedemaphysical therapy
Introduction
Statistics in our country shows that arterial and venous diseases of the limbs are almost similar to
those of Western Europe, where a woman out of four and one man out of 15 suffers from insufficient
peripheral circulation, and people with arteriopathy amount to about 1/4 of the total number of patients
with phlebitis. There were about a million and a half sick with vascular peripheral registered issues in
Romania in 2000. The patients diagnosed with peripheral circulatory failure need to be taken care of in
more clinical departments: surgery, internal medicine, cardiology, balneology and physiotherapy, and
physiotherapy. (Coleridge-Smith PD. In: Gloviczki P, Yao JST, eds.
Guidelines of the American Venous Forum. 2 ed. London: Arnold; 2001).
The purpose of this paper is that of demonstrating the effectiveness of drug treatment method
associated to that of the physical therapeutic method in ameliorating the disease and even in arresting its
development.
The hypothesis of the paper: physical therapy is a primary means in preventing peripheral
circulatory failure and a secondary one in medical treatment.
Peripheral circulatory failure. Definition (Abenhaim L.
Jantet G.
magnitude affecting the leg veins, which have in common a slowly progressive evolution of their
condition and the occurrence of chronic complications.
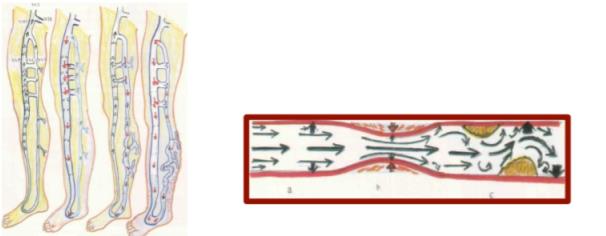
a. Normal b. postthrombotic syndrome (PTS); c. varicose syndrome; d.
CEAP classification is widely recognized: decompensated
- C (clinical) is the often visible clinical manifestations of the disease.
- E (etiology) is etiology, the cause of the condition.
- A (anatomy) refers to the affected vein segments
- P (pathology) defines how the local venous damage actually occurs.
There are six degrees of damage from simple, mild events to severely damaged vessels, echoing the
adjacent structures – muscles, structures, skin, fat, joints. ( E. Apetrei, 1979).



Objective physical exam of patients with P.C.F.
Checking the patient while standing and lying with both limbs without clothes on, examining the
front and rear. Rating: differences in thickness (edema), differences in length (present in genetic disorders)
may be seen on lower limb. Among the aspects which can be noticed upon examination, one should
mention: edema, distended veins, crown ectasias leg veins, pigmentation, skin trophic disorders (leg
ulcer), and skin nodules.
The diagnosis of peripheral circulatory failure involves: the affected limb edema, venous pain,
claudication; posture tests.
Medications and surgical treatment:
• suppression of venous reflux by crossectomy;
• suppression of dilated superficial veins by stripping;
• venous bypass methods;
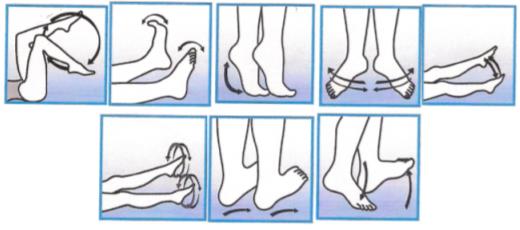
Physical therapy consists of:(Sbenghe. T. ,1996)
1. Posture Exercises, which are identifiable with peripheral ischemia tests applied symmetrically, with
functional diagnostic purposes, to assess the severity of ischemia (1, 2, 4) (Sbenghe T. : Barnea. L, 1995).
a. Buerger test
b. Ratschow Test position - supine (I) enthrosis (II) - refilling veins (III) and - increased entemulm (IV).
c Posture test
2. Oscillating bed (Forno) has peripheral vasomotor effect
3. Syncardon type pneumatic devices ("sincardiale" Fuchs massages) (Obrașcu C., 1986).
4. Smoothing circulatory effect massage, deep sliding pressure, deep, strong massage).
Connective tissue massage is applied in stage IV (trophic disorders, canker).
5. Compress therapy and gravity postural drainage: internal active compress therapy, external passive
compress therapy (elastic stockings, antigravity rubber stockings).
Research organization and conduct
This study was conducted through direct observation and tracking of the 121 cases studied
between November 2014 and May 2015 in SPINOF Physical Therapy Center of the Lower Danube
University of Galati. Patients with the following conditions were excluded: kidney dysfunction; liver
dysfunction; severe cardiac dysfunction; pure lymphedema, venous acute disorders.
Subjects were divided into three equal experimental groups, as follows:
-GROUP A - formed of patients who underwent medical treatment and physical therapy,
-GROUP B - consisted of patients who underwent only physical therapy;
-GROUP C - consisted of patients who underwent medical treatment only.
�45 patients in urban areas (the town of Galati), representing 23.80%
�76 patients in rural areas (villages adjacent to the town of Galati) representing 72.20%
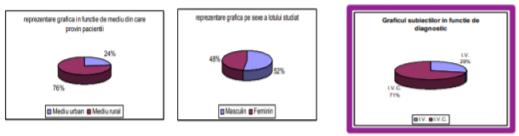
Out of the 21 subjects:
�68 were male, accounting for 52.38%
�53 were female, representing 47.62%
The study group included:
�46 patients with venous insufficiency representing 28.57%
�75 patients with chronic venous insufficiency representing 71.43%
Methods and techniques used
The Method of Theoretical Documentation; The Observation Method, The History Interview; The
Experimental Method; The Method of Graphical Representation; The Clinical Study
In terms of evaluation methods and techniques for peripheral venous circulation, I used:
Three garrot test; Trendelemberg test; anthropometric measurement of the leg (using metric band);
pain assessment (according to 0-10 visual analogue scale);
Comparison chart of the results in the first and final testing of pain assessment. Subsequent to
medication, it has been noticed that pain was reduced the most in the experimental group, A, who
received both medication and physical therapy. Pain evaluation was done according to 0-10 visual analogue graded scale.
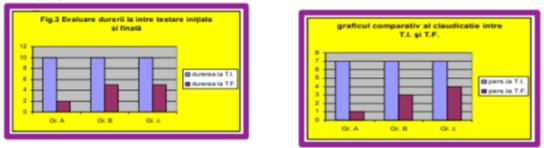
In the initial testing, all subjects in all three groups showed signs of lameness. After the treatment given in group A, only 21 individuals showed signs of lameness, while in group B there were 14, and in group C there were 56.
The graph of edema reduction following treatment
Subsequent to treatment, there was a 6 cm edema reduction in group A, and a 4 cm edema reduction in group B following the physical therapy applied, while within group C a reduction of up to 3 cm after the drug treatment was applied has been noticed.
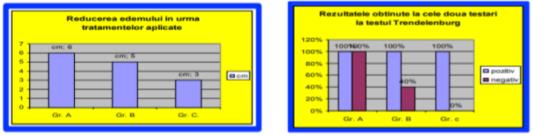
Following the applied treatment, it was noticed that the best outcome was registered within the experimental group whose treatment consisted both in medication and physical therapy
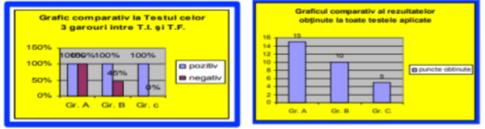
Following the medical treatment and physical therapy, all patients in the study group A had negative test results in the three garrot test.
The comparison graph on the results obtained for all tests
The values obtained were pooled and compared, the group which obtained the best results (for each test) received 3 points; the second group received 2 points, and the third one, 1 point. The most visible improvement has been noticed for group A, whose patients underwent both medication and physical therapy, followed by group B patients, who were only provided physical therapy, group C coming last, its members being exclusively given medication.
Conclusions
The study has showed the need for a minimum 3-week well-coordinated kinetic program according to the stage of the PCF condition. Its association with drug therapy significantly decreases the intensity of specific symptoms and increases the remission periods. The physical therapy programs applied to stage I PCF can reduce symptoms without requesting the administration of adequate medication. It is nevertheless hazardous not to associate physical therapy and medication in advanced symptoms cases. Physical therapy is the optimal choice in preventing the installation of peripheral circulatory failure, preferably in the case of people who are prone to PCF or present environmental factors which favor PCF occurrence.
Further suggestions
Physical therapy programs specific to the vascular system should be grouped into a minimum of 3-week physiotherapy treatment, followed by sustenance programs 2-3 times a week (primary and secondary physical prophylaxis), especially for patients who carry out standing or sitting activities.
References
- Coleridge-Smith PD. (2001). In: Gloviczki P, Yao JST, eds. Handbook of Venous Disorders. Guidelines of the American Venous Forum. 2 ed. London.
- Abenhaim, L. (1999). Phlebology. 14 (suppl. 1):1-126. 4. Jantet G. Angiology. 2002. 53:245-256.
- Chirilă, L. (1983). Recuperarea funcţională a vasculopatiilor periferice cronice .Ed Medicală, Bucureşti.
- Apetrei, E. (1979). Arteriopatiile periferice .Ed Medicală, Bucureşti.
- Gherasim, L. (1996). Medicina internă. Vol. II. Bolile cardiovascuare, metabolice. Ed medicală. Bucureşti.
- Obrașcu, C. (1986). Recuperarea bolnavilor cardiovasculari prin exerciţii fizice. Ed Medicală, Bucureşti.
- Sbersghe, T. (1996). Recuperarea medicală la domiciliul bolnavului. Ed Medicală, Bucureşti.
- brenghe T. & Barnea. L (1995) (sub red) Recuperarea bolnavilor cardiovasculari, Cluj-Napoca.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
25 May 2017
Article Doi
eBook ISBN
978-1-80296-022-8
Publisher
Future Academy
Volume
23
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-2032
Subjects
Educational strategies, educational policy, organization of education, management of education, teacher, teacher training
Cite this article as:
Cristea, F. (2017). Physical Therapy in Poor Peripheral Circulation or in Peripheral Circulatory Failure. In E. Soare, & C. Langa (Eds.), Education Facing Contemporary World Issues, vol 23. European Proceedings of Social and Behavioural Sciences (pp. 1778-1785). Future Academy. https://doi.org/10.15405/epsbs.2017.05.02.218

