Abstract
Confrontation with breast and gynecologic cancer causes difficulties of psychological adaptation. In young women, the reproductive and gynecologic consequences of the disease and treatments emerge as an additional threat. This study aimed to: (i) analyze depressive symptoms, anxiety, quality of life and reproductive concerns in young women with breast or gynecologic cancer, in comparison with healthy women; (ii) explore the mediator effect of depression and anxiety symptoms on the relation reproductive concerns → quality of life in women with cancer. This transversal study was conducted in “Centro Hospitalar Baixo Vouga II”, Aveiro, and through various Facebook pages supporting women with cancer. The sample included 95 women, 52 with breast or gynecologic cancer diagnosis and 43 healthy controls. Participants completed the Reproductive Concerns Scale, the Hospital Anxiety and Depression Scale (HADS) and the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core-30 (EORTC QLQ-C30). Diagnosed women reported more depressive symptoms, anxiety and reproductive concerns than healthy women (p<0.001). An effect mediation of depressive symptoms (p=0.001) was found. Reproductive concerns affected the quality of life in this population, by being associated with more depression and anxiety symptoms. Although there is currently a careful selection of treatments to preserve fertility, our findings show that the diagnosis of breast or gynecologic cancer in phase I to III leads to concerns and beliefs associated with impaired fertility. This fact results in difficulties of psychological adaptation. Thus, we emphasize the importance of directing the psychological interventions towards this aspect.
Keywords: Reproductive concerns, anxiety, depression, life quality
Introduction
According to WHO – International Agency for Research on Cancer, gynecologic and breast cancers showed, in 2012, a world incidence rate of 71.7/100,000 women per year. Breast cancer is the second most common cancer in the world and the most frequent cancer among women, with an estimated 1.67 million new cancer cases diagnosed in 2012 (25% of all cancers) with a incidence rate of 74.1/100,000 in developed countries. Corpus uteri cancer is the most common gynecologic cancer in developed countries (14.7/100,000 women), followed by cervical cancer (9.9/100,000 women) and ovarian cancer (9.1/100,000). While endometrial and ovarian cancers generally occur in the postmenopausal years, cervical cancer tends to emerge earlier (Carter, Stabile, Gunn, & Sonoda, 2013). In the world and in the European Region, breast and cervical cancers are the most frequent cancers at the age of 15 to 39 (Ferley et al., 2013), which means that many women diagnosed with breast and cervical cancer are of childbearing age.
Currently, the breast and gynecological cancer diagnosis assumes a reasonably good prognosis (Björneklett et al., 2013) with the advances in the field of oncology treatments. Nevertheless, the presence of psychosocial adjustment difficulties immediately after its detection and in the moment of treatments is consistently found in literature (Consolo & Romão, 2012; Silva, Crespo & Canavarro, 2012). The personal interpretation of the cancer diagnosis and the side effects of the treatments are on the basis of numerous difficulties that the patient and her family face throughout the process. Some research studies show that cancer patients presented fear of recurrence and/or death, feelings of loss of control, isolation, problems adjusting to physical changes (loss of energy, fatigue, infertility, weight gain, changes in sleep patterns and in the food, etc.), anxiety, depression, low self-esteem and changes in the body image, difficulty in sexual relationships and redefining basic values, beliefs and goals (Björneklett et al., 2013; Bloom, Stewart, Oakley-Girvan, Banks & Shema, 2012; Rodriguez & Font, 2013; Vargas et al., 2010).
High levels of stress were found especially in young women with breast and gynecologic cancer, followed by significant psychological morbidity (Gorman, Malcarne, Roesch, Madlensky & Pierce, 2010; Carter et al., 2005). The physical and psychosocial morbidity related with diagnosis and treatments can impair the performance of social roles (Dunn & Steginga, 2000; Gorman et al., 2010). At the time of diagnosis, patients who report high levels of pain, low levels of self-esteem and emotional support are at greater risk of experiencing depressive symptoms (Wong-Kim & Bloom, 2005). The quality of life can also be negatively influenced by the maintenance of psychosocial concerns after diagnosis (Consolo & Romão, 2012), despite social support be a protective factor of this injury (Ng et al., 2015).
The use of surgery, chemotherapy, endocrine therapies or a combination of these is common in the treatment of oncological diseases. Reproductive and sexual organs are frequently either directly or indirectly involved in the treatment of breast and gynecologic cancer. In premenopausal women the reproductive and gynecologic consequences can act as a wear factor, added to emotional clutter in the course of the disease. The increase in miscarriages, with a probability of 25%, and fertility problems due to adjuvant treatments are recognized risks (Mastro, Catzeddu & Venturini, 2006; Zebrack, Casillas, Nohr, Adams & Zeltzer, 2004) that young women consider distressing and divergent from their future parenting projects (Thewes et al., 2005), especially in a society where there is a tendency for women to drag the first pregnancy up to their 30 years of age. Thus, specific reproductive concerns were found in this clinical population, namely in relation of infertility and satisfaction of parenthood, early menopause and the risk of post-pregnancy recurrence, among others (Gorman et al., 2010).
Parallel to the psychological distress caused by the disease, it is important to understand the additional impact of reproductive concerns on the psychosocial adaptation to the diagnosis, in order to adjust interventions. Even today, many diagnosed women have lack of information on issues related to contraception, menopause symptoms and about one's own fertility and real reproductive effects of cancer (Zebrack et al., 2004). It is in this sense that, in our study, we defined as the main research question: “What is the relationship between reproductive concerns and psychosocial adaptation to the disease?” Some studies have already shown that the increase of reproductive concerns is associated with a higher likelihood of young women survivors of cancer to present a moderate to severe depressive condition (Gorman, Roberts, Dominick & Malcarne, 2015). Likewise, the long-term quality of life is significantly affected by concerns at this level, even after stabilization of the disease (Carter et al., 2005). However, a gap is found in understanding the indirect effects of reproductive concerns on the experience of breast and gynecological cancer.
In our study, we aimed to:
- Analyze depression and anxiety symptoms, reproductive concerns and quality of life of young women with breast and gynecologic cancer, compared with a control group;
- Explore the indirect effects of reproductive concerns on the quality of life, by their association with depression and anxiety symptoms.
Research Methods
Participants
The study included a sample of 52 young women with breast and gynecologic cancer and 43 healthy controls. The clinical population was collected in “Centro Hospitalar Baixo Vouga II”, Aveiro, and through Facebook pages to support cancer patients. Our inclusion criteria were: (i) be between the ages of 18 and 40; (ii) have previous diagnosis of stage I-III breast or gynecological cancer; (iii) be able to read and understand the Portuguese language; and (iv) not have diagnosis of psychiatric disorders, communication disorders, severe medical condition or coexisting cancer. Tables 1 and 2 present the sociodemographic and clinical characteristics of the participants. Group differences were found for all sociodemographic variables, except for the educational status. Women with breast and gynecologic cancer were older than the control sample, the majority were married, had a college degree and were employed. In terms of their clinical characteristics, 44 women had breast cancer diagnosis and the remaining had gynecologic cancer diagnosis. All these women had undergone at least one cancer treatment and 40% of them were in stage III of the disease. Still in this sample, the diagnosis was made, on average, at 34 years of age and the most common forms of cancer detection were palpation and routine medical consultation.
Measures
A questionnaire was administered to collect sociodemographic and clinical data, namely age, educational status, professional situation, cancer types, treatment cancer types, stage cancer, etc. Levels of anxiety and depression were assessed using the Hospital Anxiety and Depression Scale (HADS validated for the Portuguese population (Zigmond & Snaith, 1983; Pais-Ribeiro et al., 2007). This questionnaire includes two subscales with seven items to assess anxiety and depression. The participants should self-report their symptoms through a 4-point scale and scores for each subscales can vary between 0 and 21 points. For our sample, the internal consistence is satisfactory, assuming a Cronbach’s alpha of .868 for the anxiety subscale and .864 for the depression subscale.
We used the Portuguese version of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core-30 (EORTC QLQ-C30) to assess the quality of life of our sample (Aaronson et al., 1993; Pais-Ribeiro, Pinto & Santos, 2008). This is a 30-item inventory, targeted to cancer patients, and it is composed of five functional scales (physical, role, cognitive, emotional and social functioning), three symptom scales (fatigue, pain and nausea/vomiting), single items for the assessment of additional symptoms (dyspnoea, appetite loss, sleep disturbance, constipation, and diarrhea), one item related with financial difficulties perceived and a subscale relation with global health status/quality of life. The participants were instructed to make their assessment through a 4-point scale, ranging between “not at all” and “very much”, for most items. Regarding internal consistency for this young women sample, we found that Cronbach’s alpha coefficient was .850 for global quality life. For functional scales, the alpha value ranges between .882 and .796, and for symptoms scales it ranges between .805 and .663.
Finally, reproductive concerns were assessed with a translated version of the Reproductive Concerns Scale (RCS) (Wenzel et al., 2005). This questionnaire has 14 items and examines reproductive concerns using 5-point Likert type scales, ranging from 0 “not at all” to 4 “very much”. Similarly to the original version of the RCS, an internal consistency satisfactory was obtained in this study. The Cronbach’s alpha’s value was .812.
Procedure
This study was proposed and approved by the Ethics Committee of “Centro Hospitalar do Baixo Vouga”, before starting data collection. Wenzell et al.’s (2005) Reproductive Concerns Scale (RCS) was translated from American English to European Portuguese by translation back-translation, with the authors’ permission. The scale was analyzed in terms of conceptual, cultural and linguistic equivalence and content validity. We also used the spoken reflection to see how respondents understood the questions and then we made the necessary changes.
The participants in our study were contacted through of the external consultation of the Unit of Oncology and Pain of the hospital. The cancer patients that accepted to participate signed an informed consent and completed the sociodemographic and clinical sheets and psychological assessment instruments. However, given the small size of the sample, we also recruited some participants through support cancer pages on Facebook.
For the data analysis, we used the Statistical Package for Social Sciences, version 20 (SPSS Inc., Chicago). The sample assumed a non-normal distribution and the Mann-Whitney test was applied to examine group differences between women with and without breast and gynecological cancer diagnosis. Spearman correlations were conducted for the analysis of associations between reproductive concerns and depression, anxiety and quality of life only in cancer patients. Based on this analysis, the indirect effect of reproductive concerns on the quality of life of these women was tested using AMOS. Bootstrap methods (the bias-corrected (BC) bootstrap 95% confidence intervals (CIs)) were used to estimate significance of the mediation effect of depression and anxiety symptoms on this relation.
Findings
Differences in the psychological adjustment of the young women with or without breast and gynecologic cancer
Table 3 presents the psychological adjustment differences between the two groups included in our study. Cancer patients reported more depression and anxiety symptoms compared to healthy women. In HADS global and in its subscales, young women with diagnosis showed higher scores. Regarding the EORTC QLQ-C30 scores, we also found group differences for functional scales and symptom scales. Women without breast and gynecologic cancer diagnosis showed worse results in functional scales, namely in physical, emotional, cognitive, social and role functioning, than women with diagnosis. However, in this last group, more symptoms were reported, such as fatigue, nausea and vomiting, pain, dyspnoea and constipation, as well as more financial difficulties. Ultimately, we found that cancer patients still showed higher global scores in terms of reproductive concerns than controls.
Association between reproductive concerns of the women with breast and gynecologic cancer and anxiety, depression and quality of life
According to the correlation analysis, reproductive concerns in young women with breast and gynecologic cancer was positively associated with scores reported in the global HADS (r=.46, p=.001) and its anxiety (r=.44; p=.001) and depression (r=.42; p=.002) subscales. A negative relation was also found between reproductive concerns of these cancer patients and global health status/quality of life (r=-.42, p=.002). Conversely, these concerns assumed positive correlations with emotional (r=.38, p=.006), cognitive (r=.37; p=.007) and role functioning (r=.52; p<.001). Symptoms as fatigue (r=.37, p=.007), nausea and vomiting (r=.37, p=.007), pain (r=.40, p=.004), dyspnoea (r=0.47. p<.001) and constipation (r=.36; p=.010) were also positively associated with reproductive concerns of the sample of diagnosed women. All associations found assumed a medium or large effect size.
Based on this results the mediation model, illustrated in Figure 1, was tested.
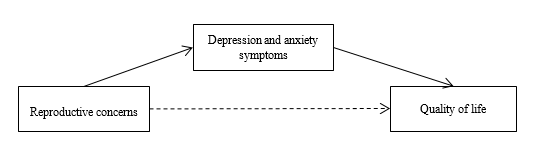
The results showed a significant total mediation effect. Depression and anxiety symptoms were mediators of the relation reproductive concern → quality of life. Increased reproductive concerns in cancer patients were associated with the presence of more depression and anxiety symptoms. As a consequence of this relation, their quality of life was negatively affected.
Conclusions
Our conclusions show that the presence of breast and gynecologic cancer in stages I to III causes psychological adaptation difficulties in young women. Compared to healthy controls, we found that cancer patients, aged between 18 and 40 years, reported more depression and anxiety symptoms, result that is consistently found in literature (Howard-Anderson, Ganz, Bower & Stanton, 2011). In contrast, the quality of life was a bit impaired. Young women with diagnosis presented a better cognitive, emotional and social functioning. This finding is not new in investigations in this area (Härtl et al., 2010; Howard-Anderson et al., 2011; Ng et al., 2015) and it may be related to the dynamism found by Danhauer, Crawford, Farmer and Avis (2009) between coping strategies and quality of life, through a predictive relation. In our sample, the adoption of adaptive coping strategies to deal with the disease may be the basis of the perception of the overall health.
In terms of reproductive concerns, the results found in this and in other studies (Garvelink, ter Kuile, Louwé, Hilders & Stiggelbout, 2015) demonstrate that young breast and gynecologic cancer patients reported more concerns of this type that healthy women. Considering that reproduction and, consequently, achievement of parenting are life cycle tasks, the onset of a cancer disease and the treatments arising can represent an additional threat.
The awareness of the impaired anatomy and reproductive function in women (Maltaris et al., 2006) and increased risk of miscarriage (Mastro, Catzeddu & Venturini, 2006) may explain our results. The studies by Simon, Lee, Partridge and Runowicz (2005) show that treatment decisions may be influenced by fertility preservation, a fact that reflects the impact of this aspect in the life of a young diagnosed woman.
Thus, in our study we also seek to understand the direct and indirect effects of reproductive concerns on psychological adjustment variables. In addition to the conclusions of the study by Gorman, Malcarne, Roesch, Madlensky and Pierce (2010), which indicate that these concerns are a predictor that accounted for 5% of the variance in depressive symptoms perceived for cancer patients, in our findings a total mediation effect on quality of life was found. The reproductive concerns of this clinical population appear to affect negatively their quality of life, by its association with more depression and anxiety symptoms. Still in the present day, women portrait themselves as the main responsible for the reproductive function and social pressure helps to maintain this belief. Faced with a disease that affects the physical health, reproductive concerns become an additional disorganization factor.
This study may be a contribution for the understanding of the psychosocial impact of reproductive concerns of young diagnosed women. Despite the increasing care in the selection of treatments to preserve fertility, the identification and intervention in the psychological rehabilitation needs at this level are still developing. However, we acknowledge some limitations in this study. The inclusion of a larger sample would make the conclusions more representative and more easily generalizable. In parallel, the adjustment of young women with breast cancer or gynecologic cancer may assume variabilities and in subsequent studies effects within each group should be considered. Likewise, the inclusion of different cancer stages, I, II and III, may be the basis for the adjustment differences and consequent impact, as well as associated treatments. The fact that anatomy and the reproductive function are more or less impaired may influence particularly the intensity of reported reproductive concerns. Lastly, we emphasize as a limitation the fact that the Reproductive Concern Scale applied is still being subjected to validation in studies for the Portuguese population. However, counteracting this methodological gap, a good internal consistency for the sample under analysis was obtained.
We suggest that future studies consider other adjustment variables, such as the marital relationship and the impact of sociodemographic and clinical aspects (for example, prior pregnancy and/or associated complications, treatments type, reproductive function changes, etc.). It is also important to carry out further research focused on the remediation and preventive psychological intervention directed to cancer patients, taking into account the influence of reproductive concerns. The understanding, by health professionals, of oncological diseases as a biopsychosocial problem is fundamental to an intervention that is integrated and adjusted to the patient’s needs.
Acknowledgements
The authors wish to thank all participants that are included in this sample.
References
Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J.,… Haes, J. C. (1993). The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of life-instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute, 85(5), 365-375.
Björneklett, H., Rosenblad, A., Lindemalm, C., Ojutkangas, M., Letocha, H. Strang, P., & Bergkvist, L. (2013). Long-term follow-up of a randomized study of support group intervention in women with primary breast cancer. Journal of psychosomatic research, 74(4), 346-353.
Bloom, J., Stewart, S., Oakley‐Girvan, I., Banks,P., & Shema, S. (2012). Quality of life of younger breast cancer survivors: persistence of problems and sense of well‐being. Psycho‐Oncology, 21(6), 655-665.
Carter, J., Rowland, K., Chi, D., Brown, C., Abu-Rustum, N., Castiel, M., & Barakat, R. (2005). Gynecologic cancer treatment and the impact of cancer-related infertility. Gynecologic oncology, 97(1), 90-95.
Carter, J., Stabile, S., Gunn, A., & Sonoda, Y. (2013). The physical consequences of gynecologic cancer surgery
and their impact on sexual, emotional, and quality of life issues. The journal of sexual medicine, 10(suppl 1), 21-34.
Consolo, F. & Romão, A. (2012). Women's poorer satisfaction with their sex lives following gynecologic cancer treatment. Clinical journal of oncology nursing, 16(3), 273-277.
Danhauer, S. C., Crawford S. L., Farmer, D. F., & Avis, N. E. (2009). A longitudinal investigation of coping strategies and quality of life among younger women with breast cancer. Journal of Behavioral Medicine, 32(4), 371-379.
Dunn, J. & Steginga, S. (2000). Young women's experience of breast cancer: defining young and identifying concerns. Psycho‐Oncology, 9(2), 137-146.
Ferlay, J., Soerjomataram, I., Ervik, M., Dikshit, R., Eser, S., Mathers, C., … Bray, F. (2013). GLOBOCAN 2012
v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://globocan.iarc.fr, accessed on 02/06/2016.
Garvelink, M.M., ter Kuile, M.M., Louwé, L.A., Hilders, C.G., & Stiggelbout, A. M. (2015). Validation of a Dutch Version of the Reproductive Concerns Scale (RCS) in Three Populations of Women. Health Care for Women International, 36(10), 1143-1159.
Gorman, J., Malcarne, V., Roesch, S., Madlensky, L., & Pierce, J. (2010). Depressive symptoms among young breast cancer survivors: the importance of reproductive concerns. Breast cancer research and treatment, 123(2), 477-485.
Gorman, J.R., Su, H.I., Roberts, S.C., Dominick, S.A., & Marcarne, V.L. (2015). Experiencing reproductive concerns as a female cancer survivor is associated with depression. Cancer, 121(6), 935-942.
Härtl, K., Schennach, R., Müller, M., Engel, J., Reinecker, H., Sommer, H., & Friese, K. (2010). Quality of life, anxiety, and oncological factors: a follow-up study of breast cancer patients. Psychosomatics, 51(2), 112-123.
Howard-Anderson, J., Ganz, P. A., Bower, J., & Stanton, A. (2011). Quality of Life, Fertility Concerns, and Behavioral Health Outcomes in Younger Breast Cancer Survivors: A Systematic Review. Journal of the National Cancer Institute, 104(5), 386-405.
Maltaris, T., Seufert, R., Fischl, F., Schaffrath M., Pollow, K., Koelbl, H., & Dittrich, R. (2007). The effect of cancer treatment on female fertility and strategies for preserving fertility. European Journal Obstetrics Gynecology Reproductive Biology, 130(2), 148-155.
Mastro, L., Catzeddu, T., & Venturini, M. (2006). Infertility and pregnancy after breast cancer: current knowledge and future perspectives. Cancer treatment reviews, 32(6), 417-422.
Ng, G.C., Mohamed, S., See, M.H., Harun, F., Dahlui, M., Sulaiman, A.H.,… Taib, N.A. (2015). Anxiety,
depression, perceived social support and quality of life in Malaysian breast cancer patients: a 1-year prospective study. Health and Quality of Life Outcomes, 13(1), 205.
Pais-Ribeiro, J., Pinto, C., & Santos, C. (2008). Estudo de validação da versão portuguesa do QLQ-C30-V.3. Psicologia, Saúde & Doenças, 9(1), 89-102.
Pais-Ribeiro, J., Silva, I., Ferreira, T., Martins, A., Meneses, R., & Baltar, M. (2007). Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychology, Healthy & Medicine, 12(2), 225-237.
Rodríguez, E. & Font, A. (2013). Eficacia de la terapia de grupo en cáncer de mama: evolución de las emociones desadaptativas. Psicooncología, 9(2-3), 275-287.
Senkus, E., Cardoso, F., & Pagani, O. (2014). Time for more optimism in metastatic breast cancer?. Cancer treatment reviews, 40(2), 220-228.
Silva, S., Crespo, C., & Canavarro, M. (2012). Pathways for psychological adjustment in breast cancer: A longitudinal study on coping strategies and posttraumatic growth. Psychology & Health, 27(11), 1323-1341.
Silva, S., Moreira, H., & Canavarro, M. (2012). Examining the links between perceived impact of breast cancer and psychosocial adjustment: the buffering role of posttraumatic growth. Psycho‐Oncology, 21(4), 409-418.
Simon, B., Lee, S. J., Partridge A. H., & Runowicz C. D. (2005). Preserving fertility after cancer. A Cancer
Journal for Clinicians, 55, 211-228.
Thewes, B., Meiser, B., Taylor, A., Phillips, K., Pendlebury, S., Capp, A., Dalley, D., Goldstein, D., Baber, R., & Friedlander, M. (2005). Fertility-and menopause-related information needs of younger women with a diagnosis of early breast cancer. Journal of Clinical Oncology, 23(22), 5155-5165.
Vargas, S., Wohlgemuth, W., Antoni, M., Lechner, S., Holley, H., & Carver C., (2010). Brief Report: Sleep Dysfunction and Psychosocial Adaptation Among Women Undergoing Treatment for Non-Metastatic Breast Cancer. Psycho-oncology, 19(6), 669-673.
Wenzel, L., Dogan-Ates, A., Habbal, R., Berkowitz, R., Goldstein, D., Bernstein, M., Kluhsman, B., Osann, K., Newlands, E., & Seckl, M. (2005). Defining and measuring reproductive concerns of female cancer survivors. JNCI Monographs, 2005(34), 94-98.
Wong‐Kim, E., & Bloom, J. (2005). Depression experienced by young women newly diagnosed with breast cancer. Psycho‐Oncology, 14(7), 564-573.
Zavesky, L., Jandakova, E., Turyna, R., Langmeierova, L., Weinberger, V., Minar, L., & Kohoutova, M. (2015). New perspectives in diagnosis of gynaecological cancers: Emerging role of circulating microRNAs as novel biomarkers. Neoplasma 62(4), 509-520.
Zebrack, B., Casillas, J., Nohr, L., Adams, H., & Zeltzer, L. (2004). Fertility issues for young adult survivors of childhood cancer. Psycho‐Oncology, 13(10), 689-699.
Zigmond, A. P. & Snaith, R. P. (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67, 361–370.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
31 July 2016
Article Doi
eBook ISBN
978-1-80296-012-9
Publisher
Future Academy
Volume
13
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-462
Subjects
Health psychology, psychology, health systems, health services, ocial issues, teenager, children's health, teenager health
Cite this article as:
Cândido, M. J., Bártolo, A., & Monteiro, S. (2016). Reproductive concerns and psychosocial adjustment of young breast and gynecologic cancer patients. In S. Cruz (Ed.), Health & Health Psychology - icH&Hpsy 2016, vol 13. European Proceedings of Social and Behavioural Sciences (pp. 227-236). Future Academy. https://doi.org/10.15405/epsbs.2016.07.02.22

