Abstract
Chronic pain affects the whole person, not just physically, but also psychologically, spiritually and emotionally. Several studies have found a relationship between chronic pain and depression. Nurses play a key role in the treatment of these conditions. Which nursing interventions are referenced in the literature for the relief of pain and depression? To identify the nursing interventions referenced in the literature for the relief of chronic pain and depression.An electronic research of articles was performed in the following databases: CINHAL Complete, CINHAL Plus and MEDLINE (via EBSCOhost). Selection criteria: experimental or quasi-experimental studies published between 1st January, 2007 and 31st December, 2014; Participants older than 18 years with chronic pain and depression; Nursing interventions; Results in relieving pain and depression.17 experimental and quasi-experimental studies were included in the final sample, all with a high level of evidence. Cognitive-behavioural therapy and education were the most frequently referenced interventions, with significant results in the relief of chronic pain and depression. Exercise and relaxation also showed an important contribution to the achievement of positive results in these conditions.There is evidence that the combination of intervention such as cognitive behavioural therapy, education and, eventually, exercise and relaxation, may have a positive contribution in reducing chronic pain and depression. The implementation of these interventions should be encompassed within a complex, multimodal treatment plan and it should be individualized, tailored to the specific characteristics of each individual.
Keywords: Chronic Pain, depression, nursing interventions
Problem Statement
Pain is a symptom that accompanies, in general terms, most pathological situations that require health care (DGS, 2003), for which reason it is a source of frequent attention in nursing practice. Nowadays, the most consensual definition of pain explains this phenomenon as an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage (International Association for the Study of Pain – IASP, 2012).
In as far as duration is concerned, pain can be classified as acute pain or chronic pain (CP). Acute pain corresponds to pain that(Portuguese Nursing Council, 2008, p. 25).
CP is defined by the Portuguese Health Directorate-General (DGS, 2008, p. 7) as persistent or recurrent pain, whose duration is equal to or longer than 3 months and/or which extends beyond the cure of the injury that caused it. According to Castro-Lopes et al. (2010) and Azevedo et al. (2012), this type of pain affects, on average, one in every five Europeans and approximately 36% of the adult population in Portugal, with repercussions on well-being, health, capacity to work or perform daily activities. In this way, we can conclude that we are faced with a serious public health problem that must be combated with every available means (Castro-Lopes et al., 2010, p. 6). In fact, CP affects the person in their entirety, not just in physical terms, but also in psychological, spiritual and emotional terms, disturbing their mental balance and affectivity deeply and violently. Seeing that, unlike acute pain, chronic pain cannot be cured by treatment, it is necessary for a person to incorporate a series of self-management strategies in order to learn to “live with” it (Metzger et al., 2002, p. 191).
In the field of health, controlling pain is the duty of all professional carers, by adopting methods of preventing and treating this significant issue, directed at every individual under their care, in order to contribute towards their well-being, while reducing morbidity and also humanising healthcare (DGS, 2008).
Depression relates to the inhibition or slowdown of one or more psychophysiological functions, loss (or decrease) of initiative and vital capacity, with prevailing feelings of guilt and a decreased sense of wellbeing (Fonseca, 1997; Matos, 2012). According to the American Psychiatric Association (2014), depressive disorders the presence of sadness, emptiness or irritability, together with somatic and cognitive changes that significantly affect the individual’s capacity to function.
The prevalence of depressive disorders in the general population is increasing. According to the World Health Organisation (WHO), depression affects approximately 350 million people worldwide and in 2020, it will became the second-leading cause of disability caused by illness (Saraiva, 2014; Frasquilho & Guerreiro, 2009). According to the Portuguese Nursing Council (2012), in Portugal, every year, approximately 7% of people suffer from depression. Saraiva (2014) states that one in every five users of the National Health Service suffers from this illness.
Depression significantly compromises every part of an individual’s life, in particular family relationships, work performance and social interactions. Furthermore, there are negative repercussions on the prognosis of other pre-existing pathologies and contributes towards the appearance of new symptoms, such as pain, anhedonia and lack of energy (Chatuverdi & Maguire, 1998, cit. Pimenta, 2000). Horimoto, Ayache & Souza (2005) say that depression is the most relevant factor causing personal, functional and social harm nowadays.
Preventing depression and suicide is one of the priority intervention areas of the National Mental Health Programme 2007-2016 (National Coordination for Mental Health, 2008). The Portuguese Nursing Council (2012) emphasises that, in view of their proximity to citizens and their responsibility in promoting health, nurses have an essential role to play in cases of depression.
The correlation between CP and depression has motivated increasing levels of interest. Although interdependence between cases has not been proven, it is undeniably assumed that a correlation does exist. Several studies and literature reviews demonstrate high prevalence of depressive disorders in people suffering from CP, and individuals with depressive symptoms suffer more intense levels of pain, as well as longer-lasting pain, with deeper implications on their life (Phyomaung et al., 2014; Ferreira-Valente et al., 2012; Farmer et al., 2010; Marta et al., 2010; Laird, 2009; Capela & Loura, 2008; Teixeira, 2006; Berber et al., 2005; Stanos, 2005; Pimenta et al., 2000). Horimoto, Ayache & Souza (2005) all corroborate these findings, emphasizing that depression and pain are related in psychological and biochemical terms, sharing neurotransmitters involved in nociceptive terminations and mood.
Within the scope of the intervention on the subject of pain and about depression, the World Health Organisation (WHO, 2007) underscores that the prescription of drugs is currently overestimated, ignoring non-pharmacological methods for controlling symptoms. This organisation also stated that, at chronic levels, pharmacological interventions may reveal inefficient, for which reason it can be necessary to include non-pharmacological interventions in the treatment.
Ribeiro & Cardoso (2007) affirmed that the suffering caused by pain, particularly in the event of chronic pain can be devastating if the patient does not receive help from family and friends and healthcare professionals, to mobilise their internal resources towards coping, modifying personal values, trying to accept them, adapting and (re)discovering a reason for the illness, the suffering and their life.
According to Teixeira (2007), the complete elimination of painful feeling, possible in most cases of acute pain, is not the main concern in most interventions on patients with chronic pain. The treatment of people suffering from chronic pain is centred, essentially, on helping them to adapt to their new condition, developing internal mechanisms that will help them cope with difficulties and maintain their quality of life. It is within this framework that the concepts of coping, self-efficacy and self-control assume all their relevance when we mention the diagnosis and treatment of pain and depression.
The concept of coping is defined by Lazarus (1991) as being the behavioural and cognitive efforts, under constant change, which aim to manage specific external or internal demands that are considered to exceed each person’s capacity.
Self-efficacy consists in the belief that individuals have in their own capacities to successfully reach a desired life objective (Bastos, 2012). It is composed of the expectation of efficacy, when a person believes in their capacity to achieve a certain goal and the expectation of result, when the person believes that the outcome will offer advantages (Salvetti & Pimenta, 2007).
Self-control is defined by the International Classification for Nursing Practice (ICNP) as a wish, translated as measures taken in order to care for what is necessary for own maintenance; in order to remain active, deal with basic and intimate needs and life activities (ICN, 2011). Ribeiro & Santos (2008) state that self-control is conditioned, on the one hand, by the characteristics of each person and, on the other hand, by the existence of interventions which healthcare professionals, particularly nurses, can offer, and adjust, to each person suffering with pain.
Research Methods
The strategy followed in order to perform this systematic literature review involved preparing a PICO question (articipants,ntervention,omparison andutcomes – Table 1): “How do nurses intervene in cases where chronic pain and depression are concurrent?” In order to perform this literature review, an online search of articles was performed on 12 February 2015, using the search engine, selecting the following databases:and
The keywords used were: (depression or “depressive symptoms”) and (“chronic pain”) and (“nurs* intervent*” “nurs* educat*” or program* or suppor* or therap*) – present in the title, the terms of the matter or the keywords – taking the following search parameters into account: ‘full text’, ‘all adult’, in the ‘Portuguese’, ‘English’ or ‘Spanish’ language. Initially, studies published between 2009 and 2014 were sought. The number of articles obtained within this time period seemed scarce, for which reason the search parameters were widened to include studies published between 2007 and 2014.
A group of inclusion and exclusion criteria was applied for the final identification of the sample, according to Table 2. The sample was selected by reading the title, the summary and, whenever necessary, the full text.
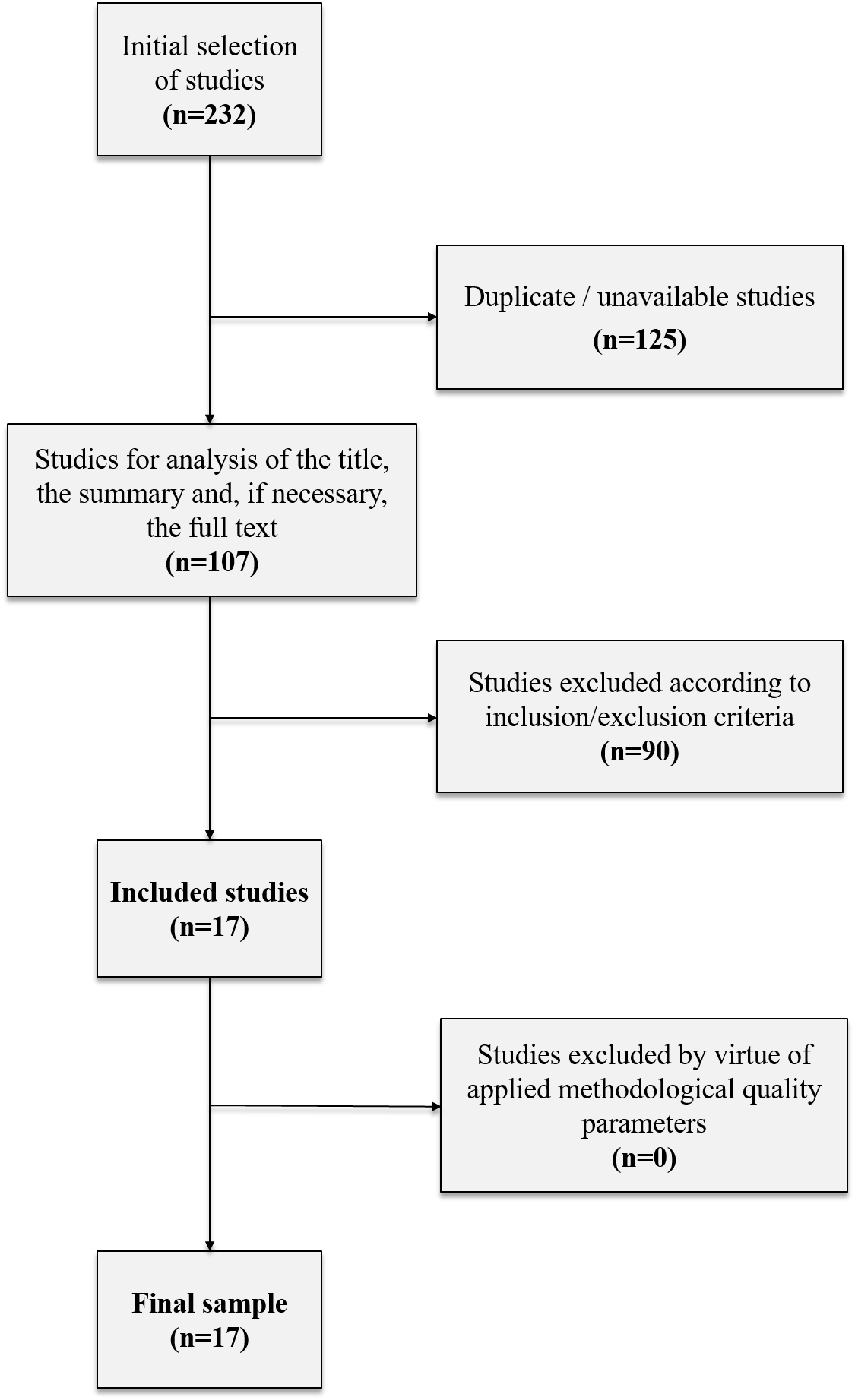
According to the search parameters, a selection of 232 studies was found, of which 118 were excluded because they had been duplicated (113 automatically and five following analysis of the article). In this way, a total of 114 studies were achieved, in 13 of which the full text was not available. Of these, three were found using the “Google” search engine. One of the remaining ten studies did not provide an email address, for which reason we were unable to contact their authors. An email was sent to the authors of the other nine studies requesting if they would provide them. We obtained a reply to three of thesent, all of them with the requested study in attachment.
At the end of this entire procedure, we had obtained a total of 107 articles. Of these, 90 were excluded according to the inclusion and exclusion criteria defined beforehand, after reading the title, the summary and, if necessary, the full text. In order to ease this selection process, a study register was created based on the inclusion-exclusion criteria defined beforehand. In this process, a final sample of 17 articles was obtained for complete analysis, which were then subject to validation of their methodological quality.
In order to assess the methodological quality of the articles obtained, the authors translated and adapted the JBI Critical Appraisal Checklist for Randomised Control/Pseudo-randomised Trial, developing two distinct instruments adjusted to the type of study: one for the appraisal of the methodological quality of the randomised trials and the other for the appraisal of the pseudo-randomised trials. Of the 17 studies analysed, six were experimental studies – randomised control trials (Poleshuck et al., 2014; McCracken, Sato & Taylor, 2013; Tse, Vong & Tang, 2013; Dear et al., 2013; Frich et al., 2012; Chen & Francis, 2010) and eleven were pseudo-randomised trials (Fullen et al., 2013; Lattie et al., 2013; Nash et al., 2013; Taloyan, Alinaghizadeh & Löfvander, 2013; Tan et al., 2013; Nicholas et al., 2011; Bremander, Holmström & Bergman, 2010; Darchuk et al., 2010; Samwel et al., 2009; Unützer et al., 2008; Field et al., 2007). Based on our methodological quality instruments, we concluded that all the studies presented a high level of evidence. Figure 1 illustrates the entire article selection process.
The “article database search” and “study selection based on inclusion/exclusion criteria” stages, specified in the methodology, were performed by two independent researchers, and there was a discrepancy of opinions as to the inclusion/exclusion of five of the articles examined. Afterwards, a consensus was achieved following analysis by a third researcher.
Findings
Participants
The clinical studies reported in this review were performed in different countries: USA (Poleshuck et al., 2014; Lattie et al., 2013; Nash et al., 2013; Darchuk et al., 2010; Unützer et al., 2008; Field et al., 2007); Republic of Ireland (Fullen et al., 2013); United Kingdom (McCracken, Sato & Taylor, 2013); Sweden (Taloyan, Alinaghizadeh & Löfvander, 2013; Bremander, Holmström & Bergman, 2010); Singapore (Tan et al., 2013); China (Tse, Vong & Tang, 2013); Denmark (Frich et al., 2012); Australia (Dear et al., 2013; Nicholas et al., 2011; Chen & Francis, 2010) and the Netherlands (Samwel et al., 2009). In many of these studies, some of the participants were immigrants. The number of participants varied between 14 and 567. All participants had CP and in all the studies, some or all of them had depression.
Instruments for Evaluation
Several instruments were used in the studies in order to evaluate the different parameters, particularly pain and depression. The quality of life, anxiety, sleep and functional capacity are examples of some of the other variables taken into account.
(Poleshuck et al., 2014; Nicholas et al., 2011; Darchuk et al., 2010); Escala numérica da dor (Fullen et al., 2013; Lattie et al., 2013; McCracken, Sato e Taylor, 2013; Tan et al., 2013; Tse, Vong e Tang, 2013);(Fullen et al., 2013);(Nash et al., 2013; Tse, Vong e Tang, 2013; Dear et al., 2013); Escala Visual Analógica de Dor (Taloyan, Alinaghizadeh e Löfvander, 2013; Frich et al., 2012; Bremander, Holmström e Bergman, 2010; Chen e Francis, 2010; Samwel et al., 2009; Field et al., 2007);(Dear et al., 2013);(Dear et al., 2013);(Chen e Francis, 2010);(Darchuk et al., 2010);(Samwel et al., 2009);(Samwel et al., 2009);(Unützer et al., 2008).
(Poleshuck et al., 2014);(Poleshuck et al., 2014);(Fullen et al., 2013; Bremander, Holmström e Bergman, 2010);(Nash et al., 2013; Tan et al., 2013; Darchuk et al., 2010);(Tse, Vong e Tang, 2013);(Frich et al., 2012);(Nicholas et al., 2011; Chen e Francis, 2010);(Samwel et al., 2009);(Unützer et al., 2008);(Field et al., 2007).
Intervention
In summary, the interventions employed in the 17 studies under analysis were:
- Interpersonal Psychotherapy (Poleshuck et al., 2014);
- Cognitive-behavioural therapy (CBT) (Fullen et al., 2013; Nash et al., 2013; McCracken, Sato & Taylor, 2013; Taloyan, Alinaghizadeh & Löfvander, 2013; Tan et al., 2013; Dear et al., 2013; Nicholas et al., 2011; Bremander, Holmström & Bergman, 2010; Darchuk et al., 2010; Samwel et al., 2009);
- Physical exercise (Lattie et al., 2013; Taloyan, Alinaghizadeh & Löfvander, 2013; Tse, Vong & Tang, 2013; Bremander, Holmström & Bergman, 2010; Darchuk et al., 2010);
- Relaxation (Tan et al., 2013; Chen & Francis, 2010; Darchuk et al., 2010; Field et al., 2007);
- Motivational Interview (Tse, Vong & Tang, 2013);
- Education (Dear et al., 2013; Fullen et al., 2013; Lattie et al., 2013; Nash et al., 2013; Tan et al., 2013; Frich et al., 2012; Nicholas et al., 2011; Darchuk et al., 2010; Unützer et al., 2008).
- Biofeedback (Darchuk et al., 2010);
- Massage (Field et al., 2007).
The table below (Table 3) presents the interventions employed and described in each article.
Effectiveness of the Intervention
Pain and depression
Out of the 17 studies under analysis, the outcome of 12 was significant improvements in terms of pain and depression, while three reported significant improvement only in pain and two reported significant improvement only with regard to depression. None of the studies presented an outcome where there was a not very significant improvement or absence of improvement in, at least, one of the two fields (CP and depression).
As we can see in Table 4, CBT was applied in ten studies and was effective in reducing pain and depression in eight, effective in reducing just pain in one and just depression in another; education was an approach used in nine studies and was effective in reducing pain and depression in six of them, effective in reducing just pain in two and just depression in one; physical exercise was employed in five studies and was effective in all of them, while relaxation was implemented in four studies, effectively reducing pain and depression in three. Each of the remaining interventions (interpersonal psychotherapy, motivational interview, and massage) were applied in one study only, with varying results.
In view of these results, two interventions stand out due to the high frequency with which they are used, compared to the others, as well as their effectiveness regarding improving CP and depression: CBT (implemented in ten of the studies) and education (implemented in nine of the studies). The (2008) underscores the existence of ever increasing evidence that proves the importance of cognitive-behavioural interventions and education in relief of CP and its repercussions, particularly at emotional level, noting that this education should be based on a multidisciplinary approach and constant interaction between user, carers and health. Also, in six of the studies analysed, CBT is implemented in association with education (Fullen et al., 2013; Nash et al., 2013; Tan et al., 2013; Dear et al., 2013; Nicholas et al., 2011; Darchuk et al., 2010). In view of the results obtained, physical exercise and relaxation should also be mentioned.
Cognitive-Behavioural Therapy
According to the American Psychiatric Association (2010), CBT has revealed an effective means of treatment for depression, increasing individuals’ capacity to maintain interpersonal relationships as well as understand and react to the cause of their depressive symptoms. The Portuguese Nursing Council (OE, 2012) also refers to CBT as a relevant means of intervention with positive results regarding depression. Some studies even conclude that CBT is the ideal means of treating depression (Butler et al., 2006; Powel et al., 2008). The effectiveness of CBT in CP has also been proven in several randomised control trials and systematic literature reviews (Williams, Eccleston & Morley, 2012; Morley, 2011; McCracken, MacKichan & Eccleston, 2007). The guidelines for evaluation and treatment of CP, developed by Hooten. (2013) recommend CBT as an important strategy in contexts of concurrent CP and depression.
Of the ten studies that used CBT as a means of intervention (almost in association with other forms of treatment), eight reported significant improvements in terms of pain and depression, one obtained a significant improvement regarding pain and another obtained a significant improvement regarding depression. These results suggest that CBT, together with other forms of therapy, can be established as an effective means of intervention in contexts where CP and depression occur.
Education
Several guidelines found within the field of pain management recommend that education should be included in its treatment (Broadfield et al., 2005; Swarm et al., 2011; Scottish Intercollegiate Guidelines Network, 2008; The British Pain Society, 2007; The British Pain Society, 2010). The British Pain Society (The British Pain Society, 2010) recommends that educating users, carers and health professionals is essential in order to obtain positive results in the field of pain management. Additionally, a meta-analysis developed by Bennet (2009) concluded that interventions within the scope of education will significantly promote knowledge and positive attitudes in the scope of pain, as well as the reduction of its intensity. The American Psychiatric Association (2010) establishes that providing education regarding depression to individuals who suffer from this condition, as well as educating their family, is a basic principle for their treatment.
Of the nine studies that used education as a means of intervention (in isolation or articulated with other forms of treatment), six (Lattie et al., 2013; Tan et al., 2013; Dear et al., 2013; Nicholas et al., 2011; Darchuk et al., 2010; Unützer et al., 2008) reported significant improvements regarding pain and depression (in one of these – Unützer et al., 2008 – education was the only intervention used), two (Nash et al., 2013; Frich et al., 2012) obtained significant improvements only regarding pain (in one of these - Frich et al., 2012 – education was the only intervention used) and one (Fullen et al., 2013) obtained significant improvements only regarding depression. These results indicate that education, especially when used in articulation with other forms of therapy, may offer positive results in treatment of contexts where CP and depression occur.
Physical Exercise
Users with CP often reduce the amount of physical exercise, over time, avoiding certain movements and exercises, compromising their physical wellbeing, muscular strength, flexibility and aerobic capacity, which has repercussions on their ability to perform daily tasks (Teixeira, 2007). Physical exercise helps fight dystrophy and muscular hypotonia, as well as improving moods, quality of life, intellectual functions, self-care abilities, sleeping patterns and anxiety, and is recommended as an important means of intervention regarding pain and depression (Ritto, s. d.). The American Psychiatric Association (2010) states that regular physical exercise may also reduce the prevalence of depressive symptoms in the general population, with some specific benefits on the elderly and on individuals who suffer from other medical problems.
All the studies (five) that implemented physical exercise as a means of intervention obtained significant positive results regarding pain and depression (Lattie et al., 2013; Taloyan, Alinaghizadeh & Löfvander, 2013; Tse, Vong & Tang, 2013; Bremander, Holmström & Bergman, 2010; Darchuk et al., 2010). However, physical exercise was not implemented on its own in any of the studies, but was always part of a multimodal intervention, for which reason it is not possible to award this form of intervention all the credit for these results.
Relaxation
Relaxation is a means of psychological reconditioning that permits the achievement of better bodily perception and increase the control over ones own body, by means of techniques in which muscular contraction is alternated with periods of relaxation (Teixeira, 2007). Relaxation with imagination consists in the decrease of muscular tension by means of the imagination, visualization and meditation, in order to increase the focus on sensations of wellbeing and decrease tension, anxiety, depression and pain associated to periods of inactivity (OE, 2008).
Of the four studies that applied this intervention, three resulted in a significant improvement regarding pain and depression (Chen & Francis, 2010; Tan et al., 2013; Darchuk et al., 2010). The fourth study (Field et al., 2007) compared and contrasted “relaxation” and “massage” interventions and found that results were improved in terms of pain and depression in the massage group, when compared to the relaxation group.
These results suggest that physical exercise and relaxation, in conjugation with other forms of intervention, may offer positive results in the treatment of situations where CP and depression occur.
Coping, Self-efficacy and Self-control
Out of all the studies under analysis, only one performed a prior appraisal and a subsequent appraisal of the intervention, regarding coping strategies; only two performed a prior appraisal and a subsequent appraisal of the intervention, regarding self-efficacy; and none of them performed an appraisal regarding self-control, so no significant results were obtained as to which interventions were effective in promoting adaptive coping, self-efficacy or self-control in people with CP and depression.
However, after performing a survey regarding the frequency within which these concepts were applied in the studies under analysis (Table 5), we can see that of the 17 studies in the sample, seven make reference to coping (Fullen et al., 2013; Lattie et al., 2013; Tan et al., 2013; Tse, Vong & Tang, 2013; Dear et al., 2013; Frich et al., 2012; Samwel et al., 2009) and five make reference to self-efficacy (Nash et al., 2013; Taloyan, Alinaghizadeh & Löfvander, 2013; Tse, Vong & Tang, 2013; Dear et al., 2013; Unützer et al., 2008).
Notwithstanding the lack of references to the concept of self-control (search for the term), seven of the studies refer to the concept of which, despite being different to the former, does involve some common points (Fullen et al., 2013; Tse, Vong & Tang, 2013; Dear et al., 2013; Nicholas et al., 2011; Darchuk et al., 2010; Samwel et al., 2009; Unützer et al., 2008). Self-management corresponds to the daily tasks performed by an individual in order to prevent, control or reduce the impact of a chronic disease, whereby patients who appropriately self-manage show attitudes and behaviour that lead to health or avoid worsening their illness. This management presumes adequate awareness of their condition and the illness they aim to prevent or control and the level of self-motivation necessary to choose and adopt healthy behaviours (Bodenheimer & Grumbach, 2007,. Almeida, 2010).
Frequent mention of coping, self-efficacy and self-management within the scope of pain and depression denotes the growing research trend towards and deeper awareness of the importance of these concepts in managing these health conditions. Nowadays, studies don’t only focus on the final result “decreasing pain intensity” or “decreasing depression”, but rather offer an approach more centred on the internal strategies that each subject can use and develop in order to cope with these phenomena. In this sense, the aim of interventions is not just to decrease pain intensity or symptoms of depression, but also to increase the internal skills of individuals to deal with chronic illnesses via self-control or self-management. The evolution of research in this field focuses its attention on the specific characteristics of each individual, emphasising them and acknowledging their key role for a personalised definition of interventions, replacing less adaptable approaches or, to put it differently, somewhat standardized approaches that did not take this individuality into account.
Multimodal approach
Out of the 17 studies analysed, 13 implemented more than one means of intervention. Only the studies of Tan (2013), Frich (2012) and Unützer (2008) implemented education alone while the study of Field (2007) applied, separately, massage and relaxation (massage was implemented in one group of participants and relaxation in another group of participants).
Additionally, 14 of the 17 studies in this sample implemented interventions aimed at CP and depression, as part of a complex and multimodal programme addressing pain management. Only the studies of Poleshuck (2014), Frich (2012) and Chen & Francis (2010) did not involve pain management programmes.
Multimodal approaches are based on the use of more than one form of therapy in order to treat CP. Pain is approached in a multidisciplinary manner, focusing on multiple fields of care (Carlson, 2014). According to the British Pain Association (2007), pain management programs are the ideal form of treatment for people suffering persistent pain that affects their quality of life. The integrated process of treatment of patients with pain (…) frequently requires adhering to several types of research and appraisal, as well as multipoint or multimodal, concomitant or sequential approaches (Teixeira, 2007).
Nurses are entirely capable of leading pain management programmes, particularly in the community, seeing that they possess the skills and closeness to users that are necessary to ensure the success of interventions (Carr, Layzell & Christensen, 2010). If nursing practitioners pay attention to opportunities to develop and implement new perspectives in the treatment of pain and associated symptoms, according to the needs revealed by the population, they can make a real difference for gains in the population’s health.
Conclusions
Nursing practitioners have a relevant part to play in the treatment of CP and depression, for they are responsible for adopting strategies that assist the illness-health process experienced by the individuals who suffer from these conditions. In this sense, they assume a crucial role, not just due to their direct contact with patients, but also in terms of research, finding evidence that justifies their professional work.
On the basis of the results obtained in this RSL, there are signs that the conjugation of different means of intervention, such as CBT, education and, possibly, physical exercise and relaxation, may offer a positive contribution towards reducing CP and depression. These interventions should be applied as part of a complex, multimodal treatment plan and should aim to increase coping, self-efficacy and self-control skills regarding the illness, in order to support its self-management. The intervention should be individualised and adapted to the specific characteristics of each person. For this purpose, it should be preceded by an extensive appraisal. Although significant results were not obtained regarding which interventions were most effective in promoting adaptive coping, self-efficacy and self-control in people with CP and depression, we can perceive, due to frequent reference to these concepts in the studies under analysis, that their importance in the treatment of pain and depression is increasingly evident in the literature.
References
Almeida L. M. (2010) – Os serviços de saúde pública e o sistema de saúde. Revista Portuguesa de Saúde Pública. Vols. 28, nº 1, pp. 79-92.
American Psychiatric Association (2010) – Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd ed.
American Psychiatric Association (2014) – Manual de Diagnóstico e Estatística das Perturbações Mentais DSM-5. 5ª Ed. Lisboa: Climepsi Editores.
Azevedo, L. F.; Costa-Pereira; A.; Mendonça, L.; Dias, C. C.; Castro-Lopes, J. M. (2012) - Epidemiology of Chronic Pain: A Population-Based Nationwide Study on Its Prevalence, Characteristics and Associated Disability in Portugal. The Journal of Pain, Vol 13, No 8 (August), 2012: pp 773-783. Disponível na internet: www.jpain.org and www.sciencedirect.com.
Bastos, F. (2014) – A pessoa com doença crónica: uma teoria explicativa sobre a problemática da gestão da doença e do regime terapêutico. Porto: Universidade Católica Portuguesa. Tese de Doutoramento.
Berber, J. S. S.; Kupek, E.; Berber, S. C. (2005) – Prevalência de Depressão e sua Relação com a Qualidade de Vida em Pacientes com Síndrome de Fibromialgia. Revista Brasileira de Reumatologia, Vol. 45, nº 2, pp. 47-54.
Bremander, A. B.; Holmström, G.; Bergman, S. (2010) – Depression and Age as Predictors of Patient-Reported Outcome in a Multidisciplinary Rehabilitation Programme for Chronic Muskuloskeletal Pain. Musculoskelet. Care, 9, pp. 41-48.
Broadfield, L. [et al.] (2005) – Guidelines for the Management of Cancer - Related Pain in Adults. Supportive Care Cancer Site Team, Cancer Care Nova Scotia.
Butler, A. C. [et al.] (2006) – The Empirical Status of Cognitive Behavioral Therapy: A Review of Meta-analyses. Clinical Psychological Review, 26, pp. 17-31.
Capela C.; Loura R. (2008) – Perturbação de Dor. Revista do Serviço de Psiquiatria do Hospital Fernando Fonseca, 1 (5), 30-45.
Carlson, M. (2014) – CBT for Chronic Pain and Psychological Well-Being. United Kingdom: Wiley Blackwell.
Castro-Lopes J. [et al.] (2010) – Pain Proposal A Dor Crónica em Portugal. Portugal, 2010.
Carr, E.; Layzell, M.; Christensen, M. (2010) – Advancing Nursing Practice in Pain Management. United Kingdom: Wiley-Blackwell.
Chen, Y. L.; Francis, A. J. P. (2010) – Relaxation and Imagery for Chronic Nonmalignant Pain: Effects on Pain Symptoms, Quality of Life and Mental Health, Pain Management Nursing, Vol 11, nº 3, pp. 159-168.
Coordenação Nacional Para A Saúde Mental (2008) – Plano Nacional de Saúde Mental 2007-2016, Resumo Executivo. Lisboa: Coordenação Nacional para a Saúde Mental.
Darchuk, K. M. [et al.] (2010) – Longitudinal Treatment Outcomes for Geriatric Patients with Chronic Non-Cancer Pain at an Interdisciplinary Pain Rehabilitation Program. Pain Medicine, 11, pp. 1352-1364.
Dear, B. F. [et al.] (2013) – The Pain Course: A randomised controlled trial of a clinician-guided Internet-delivered cognitive behaviour therapy program for managing chronic pain and emotional well-being. Pain, 154, pp. 942-950.
Direcção-Geral da Saúde (2003) – A dor como 5º sinal vital. Registo sistemático da intensidade da dor. Lisboa: DGS.
Direção-Geral Da Saúde (2008) – Programa Nacional de Controlo da Dor. Lisboa: DGS.
Farmer, C., Zaslavsky, A., Reynolds, C. F., Cleary, P. D. (2010) – Effect of Depression Treatment on Chronic Pain Outcomes. Psychosomatic Medicine, Vol. 72, nº 1, pp. 61-67.
Ferreira-Valente M. A., Ribeiro J. L., Jensen M. P. (2012) – Further Validation of a Portuguese Version of the Brief Pain Inventory Interference Scale. Clínica y Salud, Vol. 1, nº 23, pp. 89-96.
Field, T. [et al.] (2007) – Lower back pain and sleep disturbance are reduced following massage therapy. Journal of Bodywork and Movement Therapies, 11, pp. 141-145.
Frasquilho, M. A.; Guerreiro, D. (2009) – Stress, Depressão e Suicídio Gestão de Problemas de Saúde em Meio Escolar. Lisboa: Coisas de Ler Edições, 1ª ed.
Frich, L. M. H. [et al.] (2012) – Outcomes of Follow-Up Visits to Chronic Nonmalignant Pain Patients. Pain Management Nursing, Vol 13, nº 4 pp. 223-235.
Fullen, B. M. [et al.] (2013) – Ulysses: the effectiveness of a multidisciplinary cognitive behavioral pain management programme – an 8-year review. Ir J Med Sci, 183, pp. 265-275.
Hooten, W. M. [et al.] (2013) – Assessment and Management of Chronic Pain. Institute for Clinical Systems Improvement, 6.ª ed..
Horimoto, F. C.; Ayache, D. C. G.; Souza, J. A. (2005) – Depressão Diagnóstico e Tratamento pelo Clínico. São Paulo: Editora Roca.
ICN (2011) – Classificação Internacional para a Prática de Enfermagem (versão 2). Lisboa: Ordem dos Enfermeiros.
Laird, B. J. A.; Boyd, A. C.; Colvin, L. A. E Fallon, M. T. (2009) – Are cancer pain and depression interdependent? A systematic review. Psycho-Oncology, 18: 459–464.
Lattie, E. G. [et al.] (2013) – MBMD Coping Styles and Psychiatric Indicators and Response to a Multidisciplinary Pain Treatment Program. J Clin Psychol Med Settings, 20, pp. 515-525.
Lazarus, R. S. (1991) – Emotion & Adaptation. New York: Oxford University Press.
Marta, I. E. R. [et al.] (2010) – Efetividade do Toque Terapêutico sobre a dor, depressão e sono em pacientes com dor crônica: ensaio clínico. Rev Esc Enferm USP, 44(4):1100-6.
Matos, A. S. S. (2012) – Ansiedade, depressão e Coping na Dor Crónica. Dissertação apresentada à Faculdade de Ciências Humanas e Sociais da Universidade Fernando Pessoa do Porto para obtenção do grau de Mestre em Psicologia.
Mccracken, L.; Mackichan, F.; Eccleston, C. (2007) – Contextual Cognitive-behavioral Therapy for Severely Disabled Chronic Pain Sufferers: Effectiveness and Clinically Significant Changes. European Journal of Pain, 11, Published by Elsevier, pp. 314-322.
Mccracken, L. M; Sato, A.; Taylor, G. J. (2013) – A Trial of a Brief Group-Based Form of Acceptance and commitment Therapy (ACT) for Chronic Pain in General Practice: Pilot Outcome and Process Results. The Journal of Pain, Vol. 14, nº 11, pp. 1398-1406.
Metzger, C.; Muller, A.; Schwetta, M.; Walter, C. (2002) – Cuidados de Enfermagem e Dor. Avaliação da Dor, Modalidades de Tratamento, Psicologia do doente. Loures: Lusociência – Edições Técnicas e Científicas, Lda.
Morley, S. (2011) – Efficacy and Effectiveness of Cognitive-behavioral Therapy for Chronic Pain: Progress and some Challenges. Pain, 152, Published by Elsevier, pp. 99-106.
Nash, V. R. [et al.] (2013) – Cognitive Behavioral Therapy, Self-Efficacy and Depression in Persons with Chronic Pain. Pain Management Nursing, Vol. 14, nº 4, pp. 236-243.
Nicholas, M. K. [et al.] (2011) – Is adherence to pain self-management strategies associated with improved pain, depression and disability in those with disabling chronic pain? European Journal of Pain, 16, pp. 93-104.
Ordem dos Enfermeiros – Conselho De Enfermagem (2008) – DOR - Guia Orientador de Boa Prática. Lisboa: Ordem dos Enfermeiros.
Ordem dos Enfermeiros (2012) – Guia Orientador de Boas Práticas para a Prevenção de Sintomatologia Depressiva e Comportamentos da Esfera Suicidária. Cadernos OE. Série 1, nº 4.
Phyomaung, P. P. [et al.] (2014) – Are depression, anxiety and poor mental health risk factors for knee pain? A systematic review. BMC Musculoskeletal Disorders, 15:10.
Pimenta, C. A. M., Koizumi, M. S.; Teixeira, M. J. (2000) – Dor Crónica e Depressão: Estudo em 92 Doentes. Rev. Esc. Enf. USP, Vol. 34, nº 1, pp. 76-83.
Poleshuck, E. L. [et al.] (2014) – Randomized controlled trial of interpersonal psychotherapy versus enhanced treatment as usual for woman with co-occurring depression and pelvic pain. Journal of Psychosomatic Research 77, pp. 264-272.
Powel, V. B. [et al.] (2008) – Terapia Cognitivo-comportamental da Depressão. Rev Bras Psiquiatr., 30 (Supl.II), pp.73-80.
Ribeiro, A. L.; Cardoso, A. (2007) – Dor: Um Foco da Prática dos Enfermeiros. Revista Dor. Lisboa: APED, Vol. 15, nº 1, pp.6-15. ISSN: 0872-4814.
Ribeiro A. L.; Santos C. (2008) – Coping e dor crónica. Revista Servir, Vol. 56, nº 3 e 4, pp. 99-111.
Ritto, C. [et al.] (s. d.) – Manual de Dor Crónica. Associação Nacional para o Estudo da Dor Oncológica, Clínica de Dor – Instituto Português de Oncologia de Lisboa; Fundação Grunenthal.
Salvetti, M. G. & Pimenta, C. A. M. (2007) – Dor Crónica e a Crença de Auto-eficácia. Rev. Esc. Enferm. USP. nº. 41(1), pp. 135-140.
Samwel H. J. A. [et al.] (2009) – Multidisciplinary Allocation of Pain Treatment: Long-Term Outcome and Correlates of Cognitive Behavioral Processes. Journal of Muskuloskeletal Pain, Vol 17 (1), pp. 26-36.
Saraiva, C. B. (2014) – Depressão e Suicídio: Um Guia Clínico nos Cuidados de Saúde Primários. Lisboa: Lidel – Edições Técnicas, Lda.
Scottish Intercollegiate Guidelines Network (2008) – Control of Pain in Adults with Cancer A National Clinical Guideline. Edinburgh: Scottish Intercollegiate Guidelines Network.
Stanos, S. (2005) – Pain and Depression: Pathology, Prevalence and Treatment. In CNS Special Edition.
Swarm, R. [et al.] (2011) – NCCN Clinical Practice Guidelines in Oncology Adult Cancer Pain. National Comprehensive Cancer Network,Version 1.
Taloyan, M.; Alinaghizadeh, H.; Löfvander, M. (2013) – Short-term cognitive-behavioral treatment in multicultural primary care of patients with longstanding backage. Scandinavian Journal of Psychology, 54, pp. 371-375.
Tan, G. [et al.] (2013) – Improving Access to Care for Women Veterans Suffering from Chronic Pain and Depression Associated with Trauma. Pain Medicine, 14, pp. 1010-1020.
Teixeira, M. J. (2006) – Dor e Depressão. Rev. Neurociências, Vol. 14, nº 2, pp. 44-53.
Teixeira, M. J. (2007) – Dor Manual para o Clínico. São Paulo, Rio de Janeiro, Ribeirão Preto, Belo Horizonte: Editora Atheneu.
The British Pain Society (2007) – Recommended Guidelines For Pain Management Programmes For Adults. London: The British Pain Society.
The British Pain Society (2010) – Cancer Pain Management A perspective from the British Pain Society, supported by the Association for Palliative Medicine and the Royal College of General Practitioners. London: The British Pain Society's.
Tse, M. M. Y.; Vong, S. K. S.; Tang, S. K. (2013) – Motivational interviewing and exercise programme for comunity-dwelling older persons with chronic pain: a randomised controlled study. Journal of Clinical Nursing, 22, pp. 1843-1856.
Unützer, J. [et al.] (2008) – Care management for depression and osteoarthritis pain in older primary care patients: a pilot study. International Journal of Geriatric Psychiatry, 23, pp. 1166-1171.
Williams, A. C. D. C.; Eccleston, C.; Morley, S. (2013) – Psychological Therapies for the Management of Chronic Pain (excluding headache) in Adults (Review). The Cochrane Collaboration, Published by John Wiley & Sons, Ltd.
World Health Organization (2007) – WHO Normative Guidelines on Pain Management: Report of a Delphi Study to determine the need for guidelines and to identify the number and topics of guidelines that should be developed by WHO. Geneva.
International Association for the Study of Pain [Em linha] [Consult. em Fev. 2015]. (2012) Disponível na Internet:
URL:http://www.iasp-pain.org/Content/NavigationMenu/GeneralResourceLinks/PainDefinitions/#Pain.org/Content/NavigationMenu/GeneralResourceLinks/PainDefinitions/#Pain>
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
31 July 2016
Article Doi
eBook ISBN
978-1-80296-012-9
Publisher
Future Academy
Volume
13
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-462
Subjects
Health psychology, psychology, health systems, health services, ocial issues, teenager, children's health, teenager health
Cite this article as:
Gonçalves, P., Pereira, N., Ribeiro, A., & Santos, C. (2016). Nursing Interventions in Patients with Chronic Pain and Depression: A Systematic Review. In S. Cruz (Ed.), Health & Health Psychology - icH&Hpsy 2016, vol 13. European Proceedings of Social and Behavioural Sciences (pp. 12-26). Future Academy. https://doi.org/10.15405/epsbs.2016.07.02.2

