Abstract
Wellbeing of citizens is a multifactorial and a multi-aspect process. One of the key aspects is health. Despite the fact that health depends on the healthcare system on 15-20% only, it is vital to improve its efficiency. Authors highlight that, on the one hand, healthcare as social-economical system must be targeted on citizens’ health improvement, and on the other hand, it must obey economic processes. Modernization and reforming of healthcare system demand effectiveness increase of all types of resources in this context; but authors imply that the key ones are the workforce resources. A conducted monitoring of Russian Federation citizens’ health on several diseases as well as an evaluation of Russian Federation workforce resources usage through 2003-2013 (level of an institution (federal, regional, municipal), provision, staff ratio (physicians and nurses), its correspondence to staff schedule, qualifications level, etc. were used as the criteria) and also a comparison of federal districts healthcare system effectiveness (using Minmax method) did not show synonymous dynamics. Increase in staff usage effectiveness is a factor of healthcare system effectiveness raise, which is a factor of citizens wellbeing improving.
Keywords: effectivenesshealthcareworkforce resourceswellbeing
Introduction
The World Health Organization notes that health in the context of wellbeing should include at least the aspects of social, mental and physical health. At that, meaning (data) for each index of health should be determined, as well as various potential approaches should be tested and evaluated to the system of indicators with the introduction and interpretation of a single index (WHO, 2013a). The healthcare system is designed to ensure the maintaining and strengthening of public health. However, the contribution of environmental factors, economic conditions and lifestyle of the population play a much more important role in the health achievement. The importance of medical and clinical services provided by the health care system is 10-25% (Figueras et al., 2004; Wendt, 2009).
There is a special term introduced in medicine. It is called «quality of life related with health» - an integral characteristic of physical, psychological, emotional and social condition of a patient, based on his subjective perception (Starodubov et al., 2013). The modern health-related concept of life quality is based on three components: multidimensionality, variability in time and patients participation in the evaluation of their condition. The first component of life quality related with health is evaluated by characteristics, which are connected or not connected with a disease, which allow defining the influence of disease and the treatment on a patient's condition on a case-by-case basis. The second component varies in time, depending on the patient condition, which allow to provide continuous monitoring of the patient and adjust the treatment when it needs. Self-assessment of life quality, related to health, which are made by the patient - an important indicator of general state of health, influencing on the course of the disease.
Healthcare is a socioeconomic system; therefore, on the one hand, it must be primarily aimed at improving the health of individuals, and, on the other hand, the laws of economy. The global problems associated with deterioration of public health are discussed all over the world. Various ways of overcoming the crisis of healthcare are suggested, in particular, by strengthening and improving the health care system, enhancing its effectiveness (Eremina, & Kudelina, 2014a, b).
Effectiveness and Efficiency of Healthcare Systems
The European Office of the World Health Organization notes that the state should give priority to healthcare, which should be considered as an investment in the future prosperity and social wellbeing (WHO, 2009). However, the increase in spending on healthcare (The World Bank, 2015; OECD, 2015) does not lead to improvement of population`s health outcomes, some of them are even becoming worse. 36 million people (63%) of the 57 mln. died from non-communicable diseases in 2008 (WHO, 2011a, b). By 2030, the projected annual number of deaths from cardiovascular disease will reach the amount of 17-25 million people. The annual number of deaths from malignant neoplasms will reach the level of – 7.6-13 million people (WHO, 2013b). Total mortality from noncommunicable diseases are projected to be 55 million people a year; while the predicted mortality from infectious diseases will be reduced in the next 20 years.
Morbidity of the population of the Russian Federation is growing steadily, as well as it grows throughout the world. For the period from 2005 to 2013, the overall morbidity of the population increased by 17.7%, including the growth of morbidity in Siberian Federal District – 13.7% (fig. 1). Significant reduction in morbidity - to 1517.4 per 1000 population - was fixed in the Tomsk oblast in 2008, which was lower than the rate of the region and the country. However, the overall morbidity increased in subsequent years. The growth for the entire period was 3.2%.
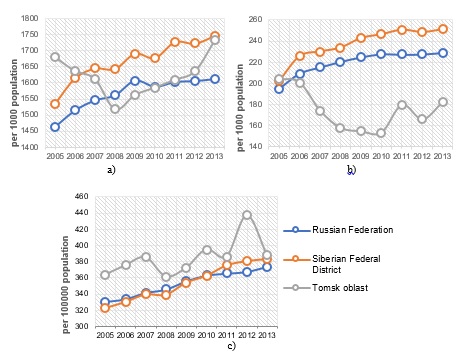
The amount of circulatory system diseases among the population of the Russian Federation and Siberian Federal District increased by 17,7% and 24,5% (respectively). During the study period, morbidity of cardiovascular system in the Tomsk oblast showed significantly low index across the country and had a reduction to 10.5% by end of 2013, despite unstable tendency toward growth in the last three years (fig. 1). The level of population`s morbidity of cancer in the Tomsk oblast has always been higher than the average indexes across the country. However, if the increase in morbidity across the Russian Federation and the Siberian Federal District was around 13.1% and 18.1%, it shows 6.7 % in the Tomsk oblast, which pays more attention to cancer pathology (fig. 1).
Taking into consideration divergent trends in health status of the population, a question arises of how efficiently resources of the healthcare system (in particular, labor resources) are used. Managers of national healthcare systems carry out a large number of functions. First, they lead the process of medical care providing (process of care delivery). Second, regional supervisors (managers) act as central government agents reforming healthcare system. Third, healthcare managers supervise workforce (Schofield, 2002). A leader should have skills of current and strategic planning, be able to make changes in his or her organization, control the situation characterizing internal processes and external relations of medical and preventive institutions (Knies, & Leisink, 2009). This includes the use of information and communication technologies (ICT) in several directions, e.g. better patient care and health care provision, analysis of the processes and better working conditions. This includes education and training in ICT (Engelbrecht et al., 2014).
On the average, in 2012 3.6 established positions of managers in Russia are accurate to 100 positions of physicians, that has been considered as the lowest index since 2002. Central Federal District and Northwestern Federal District showed a few lower level, rather than in the Russian Federation on average. Significant excess occurred in North Caucasian Federal District (4.25 managers to 100 positions of physicians), Far Eastern Federal District (4.15 managers to 100 positions of physicians) and Southern Federal District (4.06 managers to 100 positions of physicians). The amount of healthcare institution`s executives (according to the amount of staff places and including alternates) in the Russian Federation amounted to 28 100 people in 2012.
The annual negligible decrease in the number of established positions of medical institution’s executives has been recorded since 2002. The highest rate of decline took place in the last few years: 4.5% in 2011 and 6.6% in 2012. The amount of medical institution`s executives has decreased by 18.8% during the last 10 years. A similar trend, but in varying degrees, took place in all federal districts: more than 26% in Far Eastern Federal District and Volga Federal District; by 23.0% in Central Federal District; Northwestern Federal District, Siberian Federal District and Ural Federal District showed not more than 12-13% (Siburina et al., 2014).
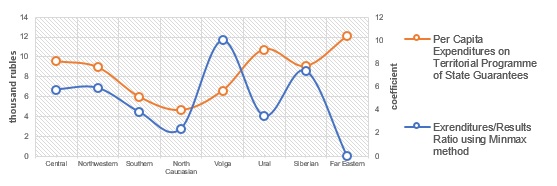
In terms of investment, the investigation of the effectiveness of healthcare systems in the federal districts showed that high or average expenditures on healthcare in any of the districts are not combined with the average results calculated by the Minimax method (fig. 2). High expenditures level in Far Eastern Federal District and Ural Federal District combined with the low effectiveness of the regional delivery of healthcare system, which is probably a consequence of inefficient budget funds usage (Eremina, & Kudelina, 2014a).
As the number of institutions, which reached an average of 54.2% in the Russian Federation has reduced, medical staff has been virtually retained (staffing positions growth was 6.4%). The number of medical institution`s executives decreased by an average of 18.8% (the rate of decline is three times lower), which may indicate either the closure of institutions, or its consolidation (Siburina et al., 2014).
With the exception of the North Caucasus Federal District, for the period from 2005 to 2013, the number of physicians in the districts has increased (table
Analysis of Tomsk Oblast Workforce Resources
Use More than 27 thousand employees work in the healthcare system in the Tomsk oblast, 3791 of which are physicians and 7537 are nursing staff. The level of medical staff provision in the region is higher than in the Russian Federation and in the Siberian Federal District (table
There are two important characteristics of workforce: staffing level availability (the ratio of individuals to staff positions) and availability of positions (the ratio of positions, which are already taken to staff positions). Over a ten-year period availability of physicians decreased by 19.4%, availability of nurses - by 12.3% (table
The ratio of the number of physicians and nursing staff is another index of the efficient workforce usage. In the Tomsk oblast this index is slightly lower (1:2,1) than the average of the Russian Federation (1:2.15), however, it varies considerably not only among urban healthcare institutions (1.6-2.0), but also among rural (3.3). This indicates an increase in the load on nurses and, consequently, speak for a deterioration in performance of operations connected with care, follow-up care and rehabilitation of patients.
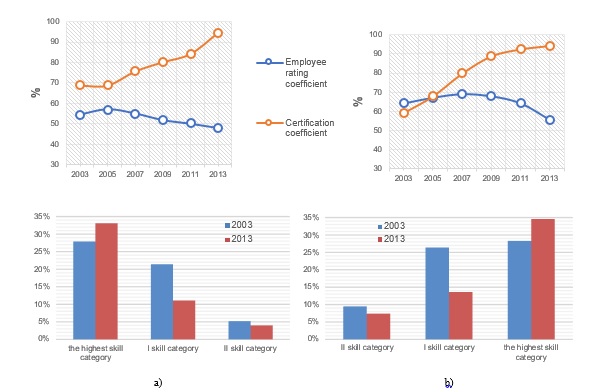
Qualitative characteristics of medical staff include the average age, coefficients of certification and employee rating. The average age of physicians in Tomsk is 48.3 ± 2.31 years, in the areas of the region – 54.82 ± 3.14 years; the average age of nurses – 54.3 ± 2.95 years in towns and 58.2 ± 4.12 years in the areas of the region. There is a growing number of specialists with a certificate, what considered as a necessary condition for the implementation of medical activities: physicians - by 29.9%, nurses - by 46.9%. (fig. 3). As for 2013, only 5.6% of medical stuff have not been certified according to established procedure. Decrease in the share of certified physicians and nurses was revealed (by 11.5% and 6.4%, respectively). At the present time 51.8% of physicians and 44.4% of nurses do not have a category, at the same time the number of professionals who have the highest category has increased, and it has decreased with skill category I and II (fig. 3).
Certainly, the level of wages considering challenging economic environment determines the attractiveness of the medical profession. According to Tomskstat (FSSS, 2015) average monthly nominal wages of health manpower resources is growing (table
While analyzing indicators of wages in different levels of healthcare institutions, it can be stated, that the trend is similar to the previous indicator, but it is not uniform across institutions (table
For the period from 2007 to 2011 public satisfaction with the quality of health care has increased not so much, despite a significant increase in workers' wages, Thus, it has increased by 12 % in Siberian Federal Districts (from 34.2 to 38.3%), by 15.9% in the Russian Federation (from 30.9 to 35.8%) (UISIS, 2015). Public satisfaction with the quality of health care in the Tomsk oblast has increased by 25.2% (from 29.7% to 37.2%).
A survey of physicians and healthcare managers in Tomsk oblast showed that 55.7% of managers assess their work as high professional, 39.2% - point the average level, 5.1% stayed with the low level. The physicians tend to evaluate work of their managers with slightly lower marks: only 48% of them rated the level of their managers as high and 8.6% of employees identified it as low. In assessing the quality of their work, 39.0% of the respondents noted the average level of performing duties, 60.3% - noted high level and 0.7% consider the level of their work as low. The level of performing duties associated with work experience (2=12.593, =2, р=0.002). The highest level of self-evaluating ranking were given by respondents with professional experience of up to 10 and over 20 years (67.7% and 62.5%, respectively), while the lowest level was noted more by respondents with professional experience of 10 to 20 years (Kudelina et al., 2013).
Conclusion
Assessing indexes of the health system presented above, it is necessary to notice, that workforce plays an essential role in enhancing effectiveness of the healthcare system (of the region). However, identified trends in public health, workers’ attitudes to their work and professional development demand managerial decisions, aimed at improving the effectiveness of labor.
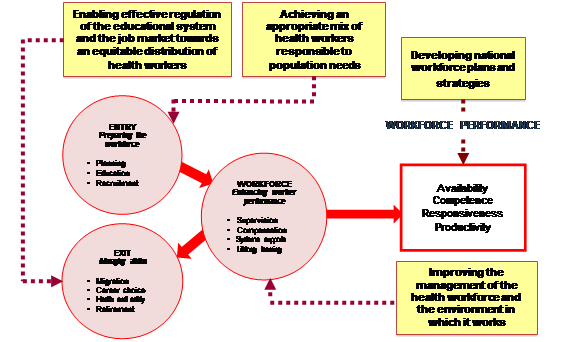
Stages of development of health`s manpower resources connected with effectiveness improvement of human resource management and reflected in the recommendations of the World Health Organization (fig. 4). National staffing strategies need to take into account features of the education system and the labor market, the real needs in health care of population, as well as to improve workforce management system and working conditions.
Assessing indexes of the health system presented above, it is necessary to notice, that workforce plays an essential role in enhancing effectiveness of the healthcare system (of the region). However, identified trends in public health, workers’ attitudes to their work and professional development demand managerial decisions, aimed at improving the effectiveness of labor.
Improving the healthcare labor resources effectiveness of the Tomsk oblast and of the country requires the adoption of certain strategies including:
determination of adequate amounts of financing of the healthcare system;
maintenance of the existing medical staff, keep them in the workplaces and motivate to work effectively;
capacity building in management and ICT, continuous medical education,
paying attention to the preparation of medium nurses and strain after achieving the optimal ratio of physicians and nurses (by recommendations of WHO 1:4-5);
conducting continuous monitoring of the labor market and to coordinate the actions of stakeholders for saving health manpower resources and strengthen the healthcare system;
development of measures oriented to harmonize the quality of staff and the distribution of staff across regions and institutions;
contribution of approval and abidance of fair labor practices for all healthcare workers.
Currently, the healthcare system is being upgraded. The changing socioeconomic conditions are serious challenges for the healthcare system. The level of professional competence of the administrative and medical staff must comply with the advanced level of socioeconomic development of the country. Effective management of human resources and its capacity building is a crucial aspect for successful reforming, modernization and enhancement of healthcare, improving the quality of population`s health and wellbeing.
References
- Engelbrecht, R., Hasman, A., Mantas, J., & Nicholson, L. (2014). International Aspects of Education and Training in Telemedicine, IJBH – International Journal on Biomedicine and Healthcare, 2(2), 41-4.
- Eremina, S., & Kudelina, O. (2014a). Effectiveness of healthcare system. Regional aspect. Society and Economics, 4, 141-57. [In Russian].
- Eremina, S., & Kudelina, O. (2014b). Evaluation of Healthcare Systems Effectiveness. A Global Experience. ECO, 10, 133-46. [In Russian].
- Figueras, J., Saltman R., Busse, R., & Dubois H. (2004). Patterns and Performance in Social Health Insurance Systems. Social Health Insurance Systems in Western Europe, 81–140.
- FSSS. (2015). Territorial body of the Federal State Statistics Service in the Tomsk oblast. Tomskstat.
- Knies, E., & Leisink, P. (2009). People management activities of police and healthcare middle managers. EGPA Annual Conference «Reinventing Government in the Information Age», Malta, 2-5 September 2009.
- Kudelina, O.V., Mytypova I.B., & Khlynin, S.M. (2013). About the attitude of Federal healthcare institutions employees to ongoing reforms. Bulletin of Siberian Medicine, 12, 1, 122–7. [In Russian].
- OECD. (2015). StatExtracts. Complete databases available via OECD's iLibrary.
- Schofield C. (2002). Contextual, policy and management reforms in the public sector: The case of the national health service. Manchester Metropolitan University Working Paper Series.
- Siburina, T.A., Miroshnikova Yu.V., & Lokhtina, L.K. (2014). Composition of executive staff in healthcare: analysis, problems and vector of development. Social Aspects of Population Health, 3(37). [In Russian].
- Starodubov, V.I., Schepin, O.P. et al. (2013). Public Health and Healthcare. National Manual. Moscow, GEOTAR-Media.
- The World Bank. (2015). Working for a World Free of Poverty. Health expenditure, total (% of GDP).
- UISIS. (2015). Unified Interdepartmental Statistical Information System. http://www.fedstat.ru/indicators/start.do.
- Wendt, C. (2009). Mapping European healthcare systems: a comparative analysis of financing, service provision and access to healthcare. Journal of European Social Policy, 19, 432-45.
- WHO. (2006) Tools and guidelines for human resources for health. http://www.who.int/hrh/tools/en/.
- WHO. (2009) Health in times of global economic crisis: implications for the WHO European Region. Meeting report.
- WHO. (2011a). Cause-specific mortality: regional estimates for 2008. Geneva, World Health Organization.
- WHO. (2011b). Causes of death 2008: data sources and methods. Geneva, World Health Organization.
- WHO. (2013a). The European health report 2012: charting the way to well-being. http://www.euro.who.int/en/data-and-evidence/european-health-report-2012.
- WHO. (2013b). World Health Statistics 2012.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
20 February 2016
Article Doi
eBook ISBN
978-1-80296-006-8
Publisher
Future Academy
Volume
7
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-513
Subjects
Social welfare, social services, personal health, public health
Cite this article as:
Kudelina, O., Eremina, S., Engelbrecht, R., & Golovkina, J. (2016). Healthcare Effectiveness as a Wellbeing Factor. Workforce. In F. Casati (Ed.), Lifelong Wellbeing in the World - WELLSO 2015, vol 7. European Proceedings of Social and Behavioural Sciences (pp. 22-30). Future Academy. https://doi.org/10.15405/epsbs.2016.02.4

