Abstract
Brief screening instruments for personality disorders could potentially have great value in community and clinical settings.This is a correlational study. One purposeful community sample (N=399; 299 teachers of primary and secondary schools in Pristina and 100 students of the European University of Tirana) and one clinical sample (N=41; patients of one private clinic) filled out the IIP-PD-25 questionnaire (Pilkonis et al.; 1996). They were randomly selected. All data was analyzed by SPSS 21 and Excel 2007.PD index screen resulted with Personality Disorder definite score 29.2% of community sample (12.5 % male vs. 16.7 % females) vs. 43.9 % of clinical sample (7.3 % male vs. 36.6 % females). Age (youngest) and residence (urban) showed significant negative correlations only for the community sample. Mann-Whitney U test did not find statistically significant differences regarding levels of PD screen index based on gender in the both samples; the same case was for differences regarding levels of PD screen index between community and clinical samples, despite the higher levels in the clinical sample. Clinical cases showed significantly higher score for the following dimensions of interpersonal sensitivity, aggression, needs for social approval and lack of sociability. Only in the case of interpersonal ambivalence, the community sample scored higher.
Keywords: personality disorders, screening, clinical, community
Introduction
Research studies have shown that the prevalence of personality disorders is significantly higher in clinical as compared to community samples (Lewin et al., 2005; Zimmerman et al, 2005). The prevalence of personality disorders in the general population varies from 7 to 15 % (Johnson et al., 2008; Adel et al., 2006; Zimmerman et al, 2005). Conversely the outpatient population shows a prevalence from 50 % to 80 % (Zimmerman et al, 2008; Alnaes & Torgersen, 1988). Finally for inpatients values as high as 70 % are reported (Thuo et al., 2008; Adel et al., 2006; Zimmerman et al, 2005) and in forensic setting (Adel et al., 2006; Zimmerman et al, 2005).
Although definitive estimates about the sex ratio of personality disorders cannot be made because ideal epidemiological studies do not exist, some personality disorders are believed to be more common in clinical settings among men and others among women (Oldham, Skodol & Binder, 2009). Zimmerman and Coryell (1989) observed higher prevalence of any personality disorders among males and results were replicated by Jackson and Burgess (2000) (ICD-10 screening) However, differences between genders were very small, and Torgersen et al. (2001) did not observe any differences.
Apparent manifestations of personality disorders must be considered in the context of a patient’s cultural reference group; indeed certain sociocultural contexts may elicit or reinforce behaviors that might be mistaken for personality disorders (Oldham, Skodol & Binder, 2009).
Zimmerman and Coryell (1989) observed that individuals with personality disorders were younger than those without. Jackson and Burgess (2000) found the same using a short ICD-10 screening instrument (IPDE screener). Torgersen et al. (2001), however, observed the opposite.
The study of Torgersen et al. (2001) showed that those living in the overcrowded city centers more often had a personality disorder.
Consequently, epidemiological surveys carried out among the general population may require very large samples in order to identify a sufficient number of cases to study demographic correlates and the association of PD with other psychiatric disorders (Loranger, Janca & Sartorius; 1997).
Comorbidity rates between personality disorders and other psychiatric disorders are well known (13–81%) (Dolan-Sewell et al., 2001). The presence of personality disorders negatively influences the treatment process and success of comorbid conditions (Kasen et al., 2007; Newton-Howes et al., 2006; Reich, 2003; Reich & Vasile, 1993; Andreoli et al, 1989; Reich & Green, 1991).There is ample evidence that patients with PDs are at higher risk for a number of maladaptive behaviors, such as substance abuse and suicidal behavior , which can interfere or complicate the course of treatment (Bell, 2005; Harris & Barraclough, 1997). Therefore screening for personality disorders represents an important aspect of the clinical psychiatric examination.
: A patient’s PD status, however, may not always be easily detected and the presence of the disorder may go undetected for some time (Baer & Blais; 2010). There is a considerable debate, however, about the choice and feasibility of methods for diagnosing PDs (Baer & Blais; 2010). Self-administered tests may represent valuable screening devices (Loranger, 1992). The literature suggests that personality disorder inventories are especially prone to false-positive diagnoses (Loranger, 1992). Nonetheless several measures exist including the Millon Clinical Multiaxial Inventory (MCMI) (Millon et al., 1997) , Personality Disorder Questionnaire-4 (PDQ-4) (Hyler, 1994), International Personality Disorder Examination (IPDE) (Loranger, 1999), Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II) (First et al., 1995), and the Structured Interview for DSM Personality-IV (SIDP-IV) (Pfohl et al., 1997). Short interviews were then developed, in which specific items from the above-mentioned interview were compiled into a brief screening interview (Morse and Pilkonis, 2007). Among these short interviews are the Iowa Personality Disorder Screen (IPDS) (Langbehn et al., 1999), the Rapid Personality Assessment Schedule (PAS-R) (Van Horn et al., 2000), the Standardized Assessment of Personality Abbreviated Scale (SAPAS) (Moran et al., 2003), an interview that was developed on the basis of 15 DSM criteria (Nurnberg et al., 2000) and Inventory of Interpersonal Problems (IIP-PD), consisting of 25 items (Pilkonis et al., 1996). Even so self-reports continue to be the most widely used in the assessment of PDs, outperforming interviews in terms of their psychometric properties (Widiger & Samuel, 2005), although they are prone to criticism because they grossly over-diagnose (Hyler, Skodol, Kellman, Oldham, & Rosnick, 1990; Wang et al., 2012).
Problem Statement
Research on Personality disorders in Kosovo is quite scarce despite the fact that psychiatrists encounter these disorders quite often. In this context, screening for personality disorders in Kosovo represents a great challenge in clinical practice. Only four studies focusing on personality disorders in Kosovo have been identified and they only consider PD in forensic contexts (Drevinja et al, 2014; Haxhibeqiri et al, 2014; Ibishi & Musliu, 2011; Ibishi, Musliu, Hundozi & Çitaku, 2014); on the other hand, no similar studies have been found in Albania.
Research Questions
What is the prevalence of personality disorders (IIP-PD-25 measure) in a community and clinical outpatient sample? Are there any differences between the clinical and community samples? Which features measured through the IIP-PD-25 are most prevalent in both samples? Does the questionnaire have discriminating validity as regards clinical and community samples.
Purpose of the Study
Brief screening instruments for personality disorders could potentially have great value in community and clinical settings. The purpose of the present study is screening for personality disorders and specific dimensions in a clinical and a community sample.
Research Methods
This is a correlational study. Data has been analyzed by SPSS 21 and Excel 2007.
Sample and procedure
One purposeful community sample (N=399; 299 teachers of primary and secondary schools in Pristina and 100 students of UET in Tirana) and one clinical sample (N=41; patients of one private outpatient clinic in Prizren) filled out IIP-PD-25 questionnaire (Pilkonis et al.; 1996). In terms of gender composition there were151 men (34.3 %) and 289 women (65.7 %). As regards residence, 397 participants lived in urban areas and, 90.2 % and 43 in rural areas (9.8 %). The age range of participants was between 16 and65 years old (Mage =37.93; SD=14.25). The clinical sample included cases with anxiety disorders (N=27, 65.9 %), assessment phase (N=8, 19.5 %), substance abuse (N=2, 4.9 %) depressive disorders (N=2, 4.9 %), conversion disorder (N=2, 4.9 %), conduct disorder (N=2, 4.9 %) and bulimia nervosa (N=2, 4.9 %).
Measuring instrument
The measuring instrument used in the present study was the Inventory of Interpersonal Problems-Personality Disorders -25 (IIP-PD-25) (Pilkonis, Kim, Proietta, & Barkham, 1996). This is a self-report instrument designed to measure the level of interpersonal distress (Pilkonis, Kim, Proietta, & Barkham, 1996; Stern, Kim, Trull, Scarpa, & Pilkonis, 2000; Baer & Blais, 2010). The version used for the purpose of the present study was developed by Pilkonis in1996 and specifically discriminates between individuals with and without personality disorders (Pilkonis, Kim, Proietta, & Barkham, 1996; Stern, Kim, Trull, Scarpa, & Pilkonis, 2000; Baer & Blais, 2010). The IIP-PD-25test measures several personality dimensions including: Interpersonal Sensitivity, Interpersonal Ambivalence, Aggression, Need for Social Approval, and Lack of Sociability. The test includes 25 items with response options from 0 to 4; results are scored according to the 5 subscales mentioned above. The first three subscales might also be considered in conjunction (mean) and they represent a screening index for the presence of personality disorders. Results are ranked in three groups : no personality disorders (less than 0.7), possible to probably (0.7-1.1), definitely (mbi 1.1). The scale might also be scored continuously, and the classification is as follows: no personality disorder (0-4), possible to probably (5-6) definitely (mbi 7).The questionnaire was translated into Albanian by using the translation back translation method to ensure correct translation. The scale has very good internal consistency (alfa=.818) similar to that reported in other studies.
Study design
The study was a cross-sectional correlational study, with age, gender, place of residence (urban, rural), community vs clinical setting as independent variables and Personality Screen Index as the dependent variable.
Findings
Descriptive analyses
The following table shows the classification of participants in terms of each variable
investigated in the study.
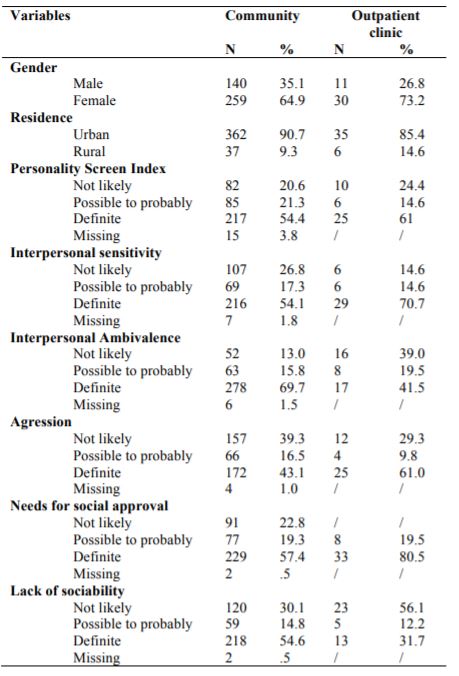
In terms of classification by PD screen index level, 217 (54.4%) of participants in the community sample reported definitely possibility for PD, 85 (21.3 %) possibly to probably and 82 participants (20.6 %) were not likely to have PD; 15 (3.8%) were dismissed because they did not answer correctly. As regards the clinical sample classification by PD screen index level, 25 (61%) of participants reported definitely possibility for PD, 6 (14.6 %) possibly to probably and 10 participants (24.4 %) were not likely to have PD.
Comparative analysis for PD screen index
Mann-Whitney U test did not find statistically significant differences regarding levels of
PD screen index and the five subscales based on gender in both samples. Similarly no differences were found regarding levels of PD screen index between community and clinical sample, despite the higher levels in clinical sample.
However there were significant differences across all subscales between the clinical and community samples More specifically there are significant differences at the level of Interpersonal sensitivity (Mdcommunity=7; N=392; Mdclinic=8; N=41) as cases from clinical sample had significantly higher Interpersonal sensitivity as compared to cases from community sample (Z=-2.291, p < .022, r = .01). Also there are significant differences in levels of Interpersonal Ambivalence (Mdcommunity=9; N=393; Mdclinic=6; N=41) as cases from community sample had significantly higher Interpersonal Ambivalence as compared to cases from the clinical sample (Z=-3.824, p < .000, r = .01). Also the clinical sample had significantly higher agresivity as compared to the community sample (Mdcommunity=6; N=395; Mdclinic=9; N=41) as (Z=-2.704, p < .007, r = .01). Significant differences were also noted at the level Need for Social Approval (Mdcommunity=7; N=397; Mdclinic=11; N=41) as the clinical sample had significantly higher Need for Social Approval as compared to the community sample (Z=-4.958, p < .000, r = .02). Finally the community sample also had significantly (Mdcommunity=7; N=397; Mdclinic=4; N=41) as cases from community sample had significantly higher Lack of Sociability as compared to cases from clinical sample (Z=-4.958, p < .000, r = .01).
Kruskal-Wallis test also found significant differences in PD screen index by participants
(students in community; teachers in community and outpatient cases (X2 (2, n=425) = 53.323, p=.000). Students had the highest scores (Md=29), followed by outpatient cases - (Md=23), and teachers community (Md=20).
Chi-square test for goodness-of-fit
A chi-square goodness-of-fit test indicated significant differences in the proportion of PD cases in the community sample (54.4%) as compared with the value of 61% that was identified in a clinical sample, X2 (2 /n = 384) = 20.299, p < .00.
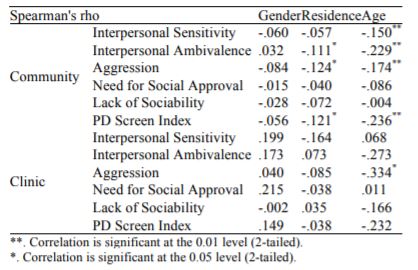
Correlations between variables
Correlational analyses indicated no significant correlations between PD screen index and gender in both samples. The same case was for all five subscales. However the PD index shows a significant negative correlation with residence in the community sample (but not the clinical one) (r=-.12, p < .01), i.e., participants from urban areas show higher rates of personality disorders. Additionally, place of residence has a significant negative correlation with ambivalence (r=-.11, p < .01) and aggression (r=-.12, p < .01), as participants from urban areas score higher in both. The finding holds only for community but not clinical settings. Age also shows a significant negative correlation with PD index at the community but not the clinical sample (r=-.23, p < .00). Age also negatively correlates to ambivalence (r=-.22, p < .00), interpersonal sensitivity (r=-.15, p < .00) and aggression (r=-.17, p < .00) at the community sample. In the clinical sample the only significant correlation is with aggression. (r=-.33, p < .03), i.e., younger age reports higher rates.
The classification of clinical and community participants based on the Personality Disorder Screen Index has been tested through the Receiver Operating Characteristic (ROC) The table indicates that the Personality Disorder Screen Index does not reliably distinguish between clinical and nonclinical cases (sig=.478).
Conclusions
Personality disorders often cause problems for others and are costly to society; early screening, identification and treatment is highly valued public health topic to be addressed. Screening with the IIP-PD-25 gives the possibility to conclude a high presence of Personality Disorders in both our samples. The study did not find significant differences between the clinical and community settings. The findings might be explained in terms of sampling limitations; convenience samples do not allow for epidemiological conclusions. (Loranger, Janca & Sartorius; 1997). The high prevalence of PD in the community sample (54.4 %) as compared to the prevalence reported in literature (7-15 %) (Johnson et al., 2008; Adel et al., 2006; Zimmerman et al, 2005) is quite concerning and requires further research. On the other hand, the prevalence rate of PD in the clinical sample (61 %) is in line with other research in the area (Zimmerman et al, 2008; Alnaes & Torgersen, 1988). The absence of gender differences is in line with the study of Torgersen et al. (2001). Findings on urban areas and young age (exclusive to the community sample) have been also reported by Torgersen et al. (2001) (for residence) Zimmerman and Coryell (1989) Jackson and Burgess (2000) (for age). However Torgersen et al. (2001) reported opposite findings on age. The age differences may explain the fact of significant higher levels in students in community. The measure used in the study also does not show discriminating validity, i.e., does not distinguish between clinical and community samples. Future research with improved methodology (both as regards sampling and measures) is required, especially considering the high prevalence rates found in the present study.
References
Adel, A., Grimm, G., Mogge, N. L., & Sharp, T. (2006). Prevalence of Personality Disorders at a Rural State Psychiatric Hospital, Journal of Rural Community Psychology, 9(1).
Alnaes, R. & Torgersen, S. (1988) DSM-III symptom disorders (Axis I) and personality disorders (Axis II) in an outpatient population. Acta Psychiatr Scand, 78:348–355.
Andreoli, A., Gressot, G., Aapro, N., Tricot, L. & Gognalons, M.Y. (1989) Personality disorders as a predictor of outcome. Journal of Personality Disorders,3: 307-20.
Baer,L. Blais, M.A. (eds.),(2010) Handbook of Clinical Rating Scales and Assessment in Psychiatry and Mental Health, Current Clinical Psychiatry, Humana Press, a part of Springer Science+Business Media, LLC
Bell, S.A.( 2005). Personality traits, problems, and disorders: Clinical application to substance use disorders. Journal of Research in Personality; 39: 84–102.
Dolan-Sewell, R.T., Krueger, R.F. & Shea, M.T. (2001) Co-occurrence with syndrome disorders, in Handbook of Personality Disorders: Theory, Research, and Treatment. Edited by Livesley WJ. NewYork, Guilford, pp 84–104.
Drevinja, F., Haxhibeqiri, Sh., Fanaj, N., Halilaj, G., Pepaj, N. & Haxhibeqiri, V. (2014) Difficulties in treatment of people with personality borderline and antisocial disorder at Dubrava prison (Kosovo). http://www1.borderline-congress.org/guest/ ID19c2e508120e10/ID7f52abaa411211/ AbstractView ? ABSID =9909
Harris, E.C. & Barraclough, B. (1997) Suicide as an outcome for mental disorders. A meta-analysis. British Journal of Psychiatry; 170: 205–228.
Haxhibeqiri, Sh., Drevinja, F., Fanaj, N., Halilaj, G., Statovci, Sh., Haxhibeqiri, V., Karameta, M., Radoniqi, B. & Rexhepi, S. (2014). Hospitalization of patient with personality disorder in university psychiatric clinic in Pristina between January 2013 until February 2014. http://www1.borderline-congress.org/guest/ID19c2e508120e10/ ID937e5f5d120ecc/AbstractView? ABSID = 9908
Hyler, S.E. (1994). Personality Diagnostic Questionnaire—4 (PDQ-4). New York, New York State Psychiatric Institute,
Hyler, S.E., Skodol, A.E., Kellman, H.D., Oldham, J.M., & Rosnick, L. (1990). Validity of the Personality Diagnostic Questionnaire-Revised: Comparison with two structured interviews. American Journal of Psychiatry, 147, 1043-1048.
First, M., Gibbon, M., Spitzer, R.L., et al. (1997). User’s Guide for the Structured Clinical Interview for DSMIV Axis II Personality Disorders. Washington, DC, American Psychiatric Press,
Ibishi, N.F., Musliu, N.R., Hundozi, Z. & Çitaku, K. (2014). Prevalence of the hospitalisation of mentally ill offenders in the Forensic Unit of the Clinic of Psychiatry in Pristina over a three-year period and long-term strategy implications for the management of the Forensic Mental Health System Service. Med Sci Law. 2014 Apr 30.
Ibishi, N. & Musliu, N.R. (2014). Prevalence of violent committed acts by inpatients in forensic setting department of psychiatry -in kosova. http://www.europsy-journal.com/article/S0924-9338 (11) 72487-7/abstract?cc=y
Jackson, H.P. & Burgess, P.M. (2000) Personality disorders in the community: a report from the Australian National Survey of Mental Health and Well Being. Soc Psychiatry Psychiatr Epidemiol 35:531–538
Johnson, J.G., Cohen, P., Kasen, S., et al. (2008) Cumulative prevalence of personality disorders between adolescence and adulthood. Acta Psychiatr Scand;118:410–413.
Kasen S, Cohen P, Skodol AE, et al (2007). Comorbid personality disorder and treatment use in a community sample of youths: a 20-year follow-up. Acta Psychiatr Scand 115:56–65,
Langbehn, D.R., Pfohl, B.M., Reynolds, S.,et al. (1999) The Iowa Personality Disorder Screen: development and preliminary validation of a brief screening interview. J Person Disord; 13:75±89.
Lewin, T,J,, Slade, T., Andrews, G., Carr, V.J. & Hornabrook, C.W. (2005) Assessing personality disorders in a national mental health survey. Social Psychiatry and Psychiatric Epidemiology; 40:87–98.
Loranger, A.W. (1999). International Personality Disorder Examination (IPDE). Odessa, FL, Psychological Assessment Resources,
Loranger, A.W., Janca, A. & Sartorius, N. (editors). (1997). Assessment and diagnosis of personality disorders: the ICD-10 International Personality Disorder Examination (IPDE). Cambridge: University Press.
Loranger,A.W. (1992) A recurrent self-report and interview measures adequate for epidemiological studies of personality disorders? Journal of Personality Disorders,6:313-25.
Millon, T., Millon, C. & Davis, R. (1997) MCMI-III Manual, 2nd Edition. Minneapolis, MN, National Computer Systems,
Moran, P., Leese, M., Lee, T., Walters, P., Thornicroft, G., Mann, A. (2003) Standardised Assessment of Personality Scale (SAPAS): Preliminary validation of a brief screen for personality disorder. British Journal of Psychiatry; 183: 228–232.
Morse, J.Q.& Pilkonis, P.A. (2007) Screening for personality disorders. Journal of Personality Disorders; 21: 179–198.
Newton-Howes, G., Tyrer, P.& Johnson, T. (2006) Personality Disorders and the outcome of depression: meta-analysis of published studies. British Journal of Psychiatry; 188: 13–20.
Nurnberg, H.G., Martin, G.A., Somoza, E., et al. (2000) Identifying personality disorders: towards the development of a clinical screening instrument. Compr Psychiatry; 41:137–146.
Oldham, J.M., Skodol, A.E. & Bender, D.S. (eds.) (2009) Essentials of personality disorders. American Psychiatric Publishing, Inc.
Pfohl, B., Blum, N. & Zimmerman, M. (1997). Structured Interview for DSM-IV Personality. Washington,DC, American Psychiatric Press,
Pilkonis, P.A., Kim, Y., Proietti, J.M., & Barkham, M. (1996) Scales for personality disorders developed from the Inventory of Interpersonal Problems. J Pers Disord;10: 355–369.
Reich, J.H. (2003) The effects of Axis II disorders on the outcome of treatment of anxiety and unipolar depressive disorders: A review. Journal of Personality Disorders; 15:387–405.
Reich, J.H. & Vasile, R.G. (1993) Effects of personality disorders on the treatment outcome of Axis I conditions: An update. Journal of Nervous and Mental Disease; 181: 475–484.
Reich, J.H. &Green, A.I. (1991) Effect of personality disorders on outcome of treatment. Journal of Nervous and Mental Disease,179:74-82.
Stern, B.L., Kim, Y., Trull, T.J., Scarpa, A. & Pilkonis, P. J. (2000) Pers Assess. Inventory of Interpersonal Problems Personality Disorder scales: operating characteristics and confirmatory factor analysis in nonclinical samples. Jun;74(3):459-71. http://www.ncbi.nlm.nih.gov/ pubmed/10900572
Van Horn, E., Manley, C., Leddy, D., Cicchetti, D. & Tyrer, P. (2000) Problems in developing an instrument for the rapid assessment of personality status. Eur Psychiatry. 15: 29-33.
Wang, L., Ross, C.A., Zhang, T., Dai, Y., Zhang, H., Tao, M., Xiao, Z. (2012). Frequency of borderline personality disorder among psychiatric outpatients in Shanghai. Journal of Personality Disorders, 26(3), 393-401.
Widiger, T.A., & Samuel, D.B. (2005). Evidence-based assessment of personality disorder. Journal of Personality Assessment, 17, 278-287.
Thuo, J., Ndetei, D.M., Maru, H., et al. (2008) The prevalence of personality disorders in a Kenyan inpatient sample. J Pers Disord; 22:217–220
Torgersen, S., Kringlen, E. & Cramer, V. (2001) The prevalence of personality disorders in a community sample. Arch Gen Psychiatry 58:590–596,
Zimmerman, M., Rothschild, L. & Chelminski, I. (2005) The Prevalence of DSM-IV Personality Disorders in Psychiatric Outpatients. American Journal of Psychiatry; 162: 1911–1918.
Zimmerman, M., Chelminski, I., Young, D. (2008) The frequency of personality disorders in psychiatric patients. Psychiat Clin N Am, 31:405–420.
Zimmerman, M. & Coryell W (1989). DSM-III personality disorder diagnoses in a nonpatient sample: demographic correlates and comorbidity. Arch Gen Psychiatry 46:682–689,
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
About this article
Publication Date
06 January 2015
Article Doi
eBook ISBN
978-1-80296-001-3
Publisher
Future Academy
Volume
2
Print ISBN (optional)
-
Edition Number
1st Edition
Pages
1-218
Subjects
Educational psychology, education, psychology, social psychology, group psychology, collective psychology
Cite this article as:
Shkembi, F., Melonashi, E., & Fanaj, N. (2015). A brief screening for personality disorders: Clinical and one nonclinical sample. In Z. Bekirogullari, & M. Y. Minas (Eds.), Cognitive - Social, and Behavioural Sciences – icCSBs 2015 January, vol 2. European Proceedings of Social and Behavioural Sciences (pp. 114-123). Future Academy. https://doi.org/10.15405/epsbs.2015.01.13

